Abstract
Diffuse large B-cell lymphoma can be subclassified into at least two molecular subgroups by gene expression profiling: germinal center B-cell like and activated B-cell like diffuse large B-cell lymphoma. Several immunohistological algorithms have been proposed as surrogates to gene expression profiling at the level of protein expression, but their reliability has been an issue of controversy. Furthermore, the proportion of misclassified cases of germinal center B-cell subgroup by immunohistochemistry, in all reported algorithms, is higher compared with germinal center B-cell cases defined by gene expression profiling. We analyzed 424 cases of nodal diffuse large B-cell lymphoma with the panel of markers included in the three previously described algorithms: Hans, Choi, and Tally. To test whether the sensitivity of detecting germinal center B-cell cases could be improved, the germinal center B-cell marker HGAL/GCET2 was also added to all three algorithms. Our results show that the inclusion of HGAL/GCET2 significantly increased the detection of germinal center B-cell cases in all three algorithms (P<0.001). The proportions of germinal center B-cell cases in the original algorithms were 27%, 34%, and 19% for Hans, Choi, and Tally, respectively. In the modified algorithms, with the inclusion of HGAL/GCET2, the frequencies of germinal center B-cell cases were increased to 38%, 48%, and 35%, respectively. Therefore, HGAL/GCET2 protein expression may function as a marker for germinal center B-cell type diffuse large B-cell lymphoma. Consideration should be given to the inclusion of HGAL/GCET2 analysis in algorithms to better predict the cell of origin. These findings bear further validation, from comparison to gene expression profiles and from clinical/therapeutic data.
Similar content being viewed by others
Main
Diffuse large B-cell lymphoma is the most common adult B-cell lymphoma and has been recognized as heterogeneous on clinical, morphological, immunophenotypic and molecular grounds.1 At least two main molecular subgroups of diffuse large B-cell lymphoma were characterized based on gene expression profiling studies: one with a profile resembling germinal center B cells and another expressing genes typically seen in activated peripheral blood B-cells.2 Other investigators subsequently confirmed these findings.3, 4, 5 The relevance of these findings is that the activated blood B-cells subtype is associated with a significantly worse clinical outcome even after the introduction of immunochemotherapy.3, 6, 7, 8, 9 Therefore, the molecular subtyping of diffuse large B-cell lymphoma may become important for therapeutic decision-making, as has already been demonstrated in several recent studies.7, 8, 10
The germinal center B-cell-like and activated blood B-cells-like subgroups cannot be reliably distinguished by morphology alone. For example, the immunoblastic and centroblastic morphological variants of diffuse large B-cell lymphoma, particularly those with a polymorphic centroblast-like cells and/or a higher content of immunoblasts, are more commonly seen in the activated blood B-cells-subgroup but are also observed in the germinal center B-cell-subgroup.5, 11 Although gene expression profiling has been a useful tool in a number of ways and has helped refine diagnostic and prognostic categories and furnished novel markers and treatment targets, this high-throughput technology is not readily applicable to routine clinical practice.1, 12 Therefore, much effort has been directed at separating diffuse large B-cell lymphoma prognostic subgroups using protein expression as assessed by immunohistochemistry, a more widely accessible method than gene expression profiling.7, 11, 13, 14, 15, 16, 17, 18 The correlation between gene expression profiling subgroups of diffuse large B-cell lymphoma, and those defined as germinal center-like and non-germinal center-like diffuse large B-cell lymphoma by immunohistochemistry, is highly variable depending on the selection of markers1, 11, 14, 16 and consequently is also highly controversial.
Immunohistochemical algorithms have been proposed with different levels of concordance with studies. The three most used are the Hans classifier,11 the Choi algorithm,14 and the recently proposed Tally algorithm16—all three algorithms employ a small panel of immunohistological markers to translate the information from gene expression profiling studies to an assay amenable for routine clinical practice. Hans et al11 demonstrated that by using a combination of three immunostains (CD10, BCL6 and MUM1), it is possible to find concordance with gene expression profiling results in 71% of germinal center B-cell and 88% of non-germinal center B-cell cases; the general concordance was estimated at 86%. In Choi algorithm, five markers were included (GCET1, CD10, MUM1, BCL6 and FOXP1, in a predetermined order),14 and the overall concordance with gene expression profiling was 93%. When the Choi algorithm was applied to patients treated with R-CHOP, the concordance with gene expression profiling results remained high (88%), and the high sensitivity, specificity, and negative predictive value of the algorithm were maintained.14 Meyer et al16 built another modification, known as the Tally algorithm, which incorporates CD10 and GCET1 as germinal center markers and, FOXP1 and MUM1 as activated B-cell markers. In this algorithm, the staining results are not examined in a particular order in addition to which another germinal center B-cell marker, LMO2, is included as a tiebreaker when an equal number of germinal center and activated markers were positive. The Tally algorithm was built on cases of diffuse large B-cell lymphoma treated with standard chemotherapy including rituximab and showed 93% concordance with gene expression profiling results from the same cases.16
HGAL (also know as GCET2) is a B-cell specific marker whose expression is observed in the cytoplasm of normal germinal center B-cells and in lymphomas of germinal center B-cell derivation, including subsets of diffuse large B-cell lymphoma, primary mediastinal B-cell lymphoma, follicular lymphoma, and Burkitt lymphoma.19, 20, 21 In the current study, we incorporated HGAL/GCET2 to the three previously described algorithms across a cohort of 424 nodal diffuse large B-cell lymphoma cases. The aim of the study was to evaluate the potential utility of HGAL/GCET2 in recognizing cases of germinal center B-cell-type diffuse large B-cell lymphoma above and beyond those cases classified as germinal center B-cell-type diffuse large B-cell lymphoma using the three original algorithms.
Materials and methods
Case Material and Clinical Data
We studied a total of 424 cases of nodal diffuse large B-cell lymphoma from the files of Consultoria em Patologia (from 2005 to 2008), a large anatomic pathology reference laboratory located in the State of São Paulo, Brazil. All cases had available material for tissue microarray construction. No cases of extranodal diffuse large B-cell lymphoma were included. Primary mediastinal B-cell lymphomas were not included. Available hematoxylin and eosin stained slides of each case from the original paraffin block were reviewed, and representative areas were selected for tissue microarray. The diagnosis was made using the criteria proposed by the WHO 2008 classification for hematopoietic neoplasia.1
Tissue Microarray Construction
Six tissue microarray blocks were constructed using a tissue arrayer (Beecher Instruments, Sun Prairie, WI, USA). Three tumor cores of 0.6 mm that had been taken from the original paraffin blocks represented each individual case. Serial sections of 3 μm were cut from the tissue array blocks and used for the immunohistochemical analysis. Proper positive and negative control cores for each marker were also included in the array block to provide an assessment of the adequacy of the antibodies used in the immunohistochemical study.
Immunohistochemistry and In situ Hybridization
Immunohistochemical studies were performed on the tissue microarray using the Novolink polymer® (Novocastra, Leica Microsystems, Buffalo, IL, USA) as the detection system, and an epitope-retrieval method was applied as needed for each specific antibody; diaminobenzidine (DAB) was the chromogen. The specifications of primary antibodies used in this study are shown in Table 1. MUM1, CD10, BCL-6, HGAL/GCET2, LMO2, and BCL-2 were considered positive above a 30% cutoff of staining. GCET1 and FOXP1 were considered positive above 80% of stained cells, according to Choi et al14 At least 10 high-power fields, including tumors, were evaluated. The Ki-67 proliferative index (PI) was evaluated using the monoclonal antibody MIB1, assigning a percentage value calculated by scoring 500 tumor cell nuclei. Sections from the tissue microarray were examined for the expression of Epstein–Barr viral (EBV) RNA by in situ hybridization using the EBER-1 probe, as previously described.22
Algorithms Methodological Description
Initially, the cases of diffuse large B-cell lymphoma were separated using three previously described immunohistochemical algorithms. In the ‘Hans classifier’,11 germinal center-subtype was defined as either all cases expressing CD10 or cases that were CD10 negative, BCL-6 positive, and MUM-1 negative. All cases that were CD10 negative and MUM1 positive, irrespective of BCL-6, were considered to be of non-germinal-center subtype; Choi et al14 used GCET1, CD10, BCL6, MUM1, and FOXP1 in a specific order to separate germinal-center subtype from non-germinal-center subtype cases. The cases positive for GCET1 without MUM1 expression, or CD10 positive or BCL6 positive without FOXP1 expression, were classified as germinal-center subtype. The cases with GCET1 and MUM1 positivity and the cases with GCET1 negative, CD10 negative, BCL6 negative or CD10 negative, and BCL6 positivity with FOXP1 positive, were assigned to the non-germinal-center subtype group. The Tally algorithm proposed by Meyer et al16 combines CD10 and GCET-1 as germinal center markers and MUM1 and FOXP1 as non-germinal-center subtype markers, and score cases on a scale of 0 (both negative), 1 (only one positive), and 2 (positive for both) marker pairs; it includes another germinal center marker LMO223 as a tie-breaker when an the score is equal for germinal center and non-germinal-center subtype markers. We then reclassified all cases after including HGAL/GCET2 to the three algorithms. The inclusion of HGAL/GCET2 as another germinal center marker was done as follows: in the Hans classifier, HGAL/GCET2 was equivalent to CD10; when positive, the case was then classified as germinal-center subtype. In the Choi algorithm, HGAL/GCET2 was included after GCET1, and in the Tally algorithm, it was considered equivalent to LMO2. When scores were equal, an HGAL/GCET2-positive result was considered to define a case as germinal-center subtype type. The strategy of how HGAL/GCET2 immunostaining was used in the three algorithms is summarized in Figure 1.
Diagrams of modified Hans (a), Choi (b), and Tally (c) algorithms with the inclusion of HGAL/GCET2. The introduction of HGAL/GCET2 in each algorithm is highlighted in yellow, showing it position and how the cases being separated according to the expression (+) or absence (−) for the different markers used in each algorithm.
Statistical Analysis
The χ2 test was used to compare the results of the different algorithms as originally proposed and with the addition of HGAL/GCET2. As a measure of concordance, the κ test was applied. The relationship between the markers was obtained based on the Breslow's linear adjust model considering the markers as independent variants in univariate and multivariate analysis. The significance level used in the study was 5%.
Results
The 424 nodal diffuse large B-cell lymphoma cases included 203 females with a mean age of 61.3 years old (ranging from 20 to 90) and 221 males with a mean age of 56.4 years old (ranging from 9 to 92). The female mean age was significantly higher than the male mean age (P=0.004).
All the cases were CD20-positive in the neoplastic cells with no expression of CD3. The expression of the other markers is shown in Table 2. Applying the Hans classifier11 to this series, 114 (27%) cases were categorized as germinal-center subtype and 310 cases (73%) as non-germinal-center subtype. Applying the Choi algorithm,14 144 cases were classified as germinal-center subtype (34%) and 280 cases (66%) as activated B-cell. The Tally16 algorithm identified 79 cases (19%) as germinal-center subtype and 345 cases (81%) as activated B-cell. For the original algorithms, the association between the Hans and Choi's classifiers was statistically significant, P<0.001 (χ22=160.5), with the percentage of concordant results of 84%. The discordant cases were 12% of the patients that were classified as germinal-center subtype type by the Choi algorithm and non-germinal-center subtype type by the Hans algorithm, but the concordance measure, κ, was still high (κ=0.612; P<0.001). In the comparison of the Hans and Tally's algorithms, the association was also statistically significant (χ2=134.7; P<0.001). The frequency of concordant results was 84%. The non-concordant cases corresponded mainly to those cases considered germinal-center subtype by the Hans algorithm and non-germinal-center subtype by the Tally algorithm and included 12% of the patients (κ=0.555, P<0.001). When the Choi and Tally's algorithms were compared, the concordance was lower by 73%, but remained statistically significant (κ=0.356, P<0.001). The non-concordant cases corresponded mainly to those cases considered germinal-center subtype by the Choi algorithm and non-germinal-center subtype by the Tally algorithm, corresponding to 21% of the cases. All three algorithms showed positive association and the higher concordance was between Choi and Hans followed by Hans and Tally's algorithms; the lowest concordance was between the Choi and Tally's algorithms.
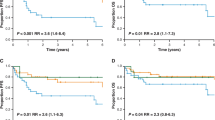
The addition of HGAL/GCET2 significantly increased the frequency of cases classified as germinal-center subtype subtype in all three algorithms (Table 3) (Figure 2). The distribution of germinal-center subtype and non-germinal-center subtype subtypes classified by the Hans algorithm with HGAL/GCET2 (modified Hans) showed 162 cases (38%) of germinal-center subtype and 262 cases (62%) of non-germinal-center subtype subtypes. The addition of HGAL/GCET2 to the Choi algorithm (modified Choi) showed 202 cases of germinal-center subtype (48%) and 222 of non-germinal-center subtype (52%) subtypes. The Tally algorithm with the inclusion of HGAL/GCET2 (modified Tally) showed 150 (35%) germinal-center subtype cases and 274 (65%) non-germinal-center subtype cases.
The impact of classifying cases of the germinal-center subtype in the modified algorithms is related with the number of cases that had the status of non-germinal-center subtype modified to germinal-center subtype. The increment of germinal-center subtype cases with the introduction of HGAL/GCET2, in Hans algorithm, was estimated at 17%, in the modified Choi algorithm, 13.9%, and in the modified Tally algorithm, 16.7%, and the difference between originally and modified algorithm was statistically significant in all of the algorithms (P<0.001), for recognizing germinal-center subtype cases. The concordance between the Hans and Choi's algorithms was also increased from κ=0.612 (without HGAL/GCET2) to κ=0.714 (with HGAL/GCET2) (P<0.001). The concordance between the Hans and Tally's algorithms changed from κ=0.555 (without HGAL/GCET2) to κ=0.858 (with HGAL/GCET2) (P<0,00). Between the Choi and Tally's algorithms, where the initial concordance was the lowest, the modified algorithms (with HGAL/GCET2) showed a significantly increased proportion of cases (κ=0.675, P<0.001).
In multivariate analyses comparing the four germinal center markers, CD10 was the only independent marker (P<0.001). The mean value of Ki-67-proliferation index was 56%, ranging from 20 to 90% with a non-significant difference comparing germinal-center subtype and non-germinal-center subtype subtypes. The immunohistochemical result of single antigens is detailed in Table 2, comparing with the literature.
BCL-2 expression was observed in 181 cases—60 cases (33%) of germinal-center subtype and 121 cases (67%) of non-germinal-center subtype. Taking all germinal-center subtype cases, BCL2 expression was observed in 42% (60/144); in non-germinal-center subtype cases, BCL2 was positive in 43% of the cases (121/280), with no statistically significant difference. In situ hibridization for EBER was negative in all the cases.
Discussion
In the last decade, the success of gene expression profiling in identifying molecular subtypes of diffuse large B-cell lymphoma that are of clinical and prognostic significance2, 3, 4 prompted many investigators to attempt the development of immunohistological algorithms for this purpose.11, 13, 14, 16, 24 This task, however, has proven to be far more challenging than initially anticipated, at least in part owing to the limited numbers of antibody reagents available for immunohistochemistry. Subtyping diffuse large B-cell lymphoma into prognostic groups based on immunohistological algorithms has the great advantage that the methodology is readily available in diagnostic pathology laboratories and can be easily performed on formalin-fixed, paraffin-embedded tissue. Nevertheless, there has been significant controversy over the selection of the most appropriate panel of markers to be employed for immunohistochemistry, differences in methodology and scoring criteria, and the degree to which each algorithm approximates gene expression profiling-derived prognostic subgroups. In addition, improvement in the treatment strategies for diffuse large B-cell lymphoma, such as the initiation of immunochemotherapy, further confounded the ability to separate prognostic subgroups with markers defined in a previous treatment era. Data from large prospective clinical trials to validate these findings are also lacking. We set out to test whether the addition of HGAL/GCET2 to previously defined algorithms could improve the accuracy of detection of the germinal center B cell subtype, and our findings indeed support that conclusion.
The three most commonly used algorithms collectively employ the following immunohistological markers: CD10, BCL6, MUM1, BCL2, FOXP1, GCET1, and LMO2. Although the first four of these markers have been used in lymphoma diagnosis for a number of years, FOXP1, GCET1, and LMO2 have not; they were identified by germinal expression profiling or selected RT-PCR studies to be of significance in the context of prognostication in diffuse large B-cell lymphoma. FOXP1 is a winged-helix transcription factor that is differentially expressed in resting and activated B cells. FOXP1 (forkhead box P1) expression has been demonstrated in a subset of diffuse large B-cell lymphoma and is more common in the non-germinal center subgroup, as in our series. It has been suggested that FOXP1 expression is an independent prognostic factor in diffuse large B-cell lymphoma patients.25, 26 GCET-1 is highly restricted to germinal center B-cell and to germinal center B cell-derived cell lines and lymphomas.27, 28 Its expression has been observed in variable proportions of diffuse large B-cell lymphoma (20-50%) in different studies, most likely due to differences in scoring criteria.28, 29 In addition, we also assessed the expression of LMO2, which was incorporated into the Tally algorithm. LMO2 expression in diffuse large B-cell lymphoma ranges in frequency from 40 to 55%.23, 29, 30 In the current study, we introduced HGAL/GCET2 in addition to the other previously described markers. HGAL/GCET2 protein is specifically expressed in lymphocytes within the germinal center in normal lymphoid tissue revealing cytoplasmic expression by immunohistochemistry. It has also been observed in a wide range (40 to 70%) of diffuse large B-cell lymphoma, with variable expression from strong reactivity in the majority of lymphoma cells to localized and even weak reactivity in a subset of the cells.20, 23, 29
The Hans classifier11 was one of the initially proposed algorithms with 87% of concordance with germinal expression profiling results; germinal center B subtype was defined as all cases expressing CD10 and cases that were CD10-negative, BCL6-positive, and MUM1- negative. All cases that were CD10-negative and MUM1-positive, irrespective of the BCL-6 result, were considered to be of non-germinal center-B-subtype origin.
The Choi algorithm considered the expression of GCET-1 and FOXP1 in addition to CD10, BCL6 and MUM1, thereby adding one marker each from germinal center B subtype and activated B cell-derived gene signatures. GCET-1 (germinal center B-cell-expressed transcript 1) is also highly restricted to germinal center B-cells and germinal center B cell-derived cell lines and lymphomas.27 The LMO2 protein has been described as highly expressed in lymphocytes within the germinal center in normal tonsils and lymph nodes. In germinal center B-cell-derived cell lines and lymphomas, the staining is localized to the nucleus.23 Besides the use of markers, Choi algorithm also considers the order of interpretation, being that GCET1 is the first one evaluated followed by MUM1 or CD10, and then in cases where GCET1/CD10 are negative, BCL6 followed by FOXP1 is applied sequentially. In the Choi algorithm, the overall concordance with GEP was 93 and 88% when R-CHOP-treated cases were analyzed.14 Meyer et al 16 built another algorithm (Tally) using CD10 and GCET1 as germinal center B-cell-markers and FOXP1 and MUM1 as activated B-cell markers. The immunostaining results are not examined in a particular order and include another germinal center B-cell-marker, LMO2,23 as a tiebreaker when an equal number of germinal center and activated antigens present a positive result.
The use of an immunohistochemistry algorithm has been variably adopted diagnostically and has been incorporated into the British Committee on Standards in Hematology guidelines for lymphoma diagnosis.24 It proposed the use of the same three markers as Hans; however, the guidelines suggest that the cases that are negative for all germinal center markers and those that have one positive germinal center marker and expresses MUM1, should be designated unclassifiable cases.27
In a series of 157 cases of diffuse large B-cell lymphoma studied by Gutierrez-Garcia et al,29 the application of Colomo and Hans algorithms was similar—41% of germinal center B-subtype and 59% of non-germinal center B-subtype immunophenotype. In the same study using Choi and Tally's algorithms, the proportion of non-germinal center B subtype assigned was significantly higher—67% and 63% respectively. In our cases, by applying the Choi algorithm without HGAL/GCET2, we found similar result, 34% germinal center B subtype and 66% of non-germinal center B subtype, but when HGAL/GCET2 was included, cases designated as germinal center B subtype increased to 48%.
In conclusion, our findings show that HGAL/GCET2 is an excellent germinal center B-cell-specific marker whose inclusion in immunohistological algorithms may be employed in the prognostic stratification of diffuse large B-cell lymphoma to improve the detection of the germinal center B subtype subgroup compared with the three other commonly used immunohistological algorithms. The addition of HGAL/GCET2 may, therefore, translate to a better approximation of immunohistologically classified cases with that of gene expression profiling. These findings, however, should be confirmed in an independent cohort of well-characterized cases and compared with gene expression profiling results from the same cases for appropriate validation before being used in the clinical setting.
References
Stein H, Warnke RA, Chan WC, et al. In: Swerdlow S, Campo E, Harris, NL, Jaffe E, Pileri S, Stein H, Thiele J, Vardiman J (eds). WHO Classification of Tumours of Hematopoietic and Lymphoid Tissues. IARC Press: Lyon, 2008, pp 233–251.
Alizadeh AA, Eisen MB, Davis RE, et al. Distinct types of diffuse large B-cell lymphoma identified by gene expression profiling. Nature 2000;403:503–511.
Rosenwald A, Wright G, Chan WC, et al. The use of molecular profiling to predict survival after chemotherapy for diffuse large-B-cell lymphoma. N Engl J Med 2002;346:1937–1947.
Wright G, Tan B, Rosenwald A, et al. A gene expression-based method to diagnose clinically distinct subgroups of diffuse large B cell lymphoma. Proc Natl Acad Sci USA 2003;100:9991–9996.
Hummel M, Bentink S, Berger H, et al. A biologic definition of Burkitt's lymphoma from transcriptional and genomic profiling. N Engl J Med 2006;354:2419–2430.
Lenz G, Wright GW, Emre NC, et al. Molecular subtypes of diffuse large B-cell lymphoma arise by distinct genetic pathways. Proc Natl Acad Sci USA 2008;105:13520–13525.
Nyman H, Adde M, Karjalainen-Lindsberg ML, et al. Prognostic impact of immunohistochemically defined germinal center phenotype in diffuse large B-cell lymphoma patients treated with immunochemotherapy. Blood 2007;109:4930–4935.
Rimsza LM, Wright G, Schwartz M, et al. Accurate classification of diffuse large B-cell lymphoma into germinal center and activated B-cell subtypes using a nuclease protection assay on formalin-fixed, paraffin-embedded tissues. Clin Cancer Res 2011;17:3727–3732.
Shipp MA, Ross KN, Tamayo P, et al. Diffuse large B-cell lymphoma outcome prediction by gene-expression profiling and supervised machine learning. Nat Med 2002;8:68–74.
Dunleavy K, Pittaluga S, Czuczman MS, et al. Differential efficacy of bortezomib plus chemotherapy within molecular subtypes of diffuse large B-cell lymphoma. Blood 2009;113:6069–6076.
Hans CP, Weisenburger DD, Greiner TC, et al. Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 2004;103:275–282.
Orsborne C, Byers R . Impact of gene expression profiling in lymphoma diagnosis and prognosis. Histopathology 2011;58:106–127.
Chang CC, McClintock S, Cleveland RP, et al. Immunohistochemical expression patterns of germinal center and activation B-cell markers correlate with prognosis in diffuse large B-cell lymphoma. Am J Surg Pathol 2004;28:464–470.
Choi WW, Weisenburger DD, Greiner TC, et al. A new immunostain algorithm classifies diffuse large B-cell lymphoma into molecular subtypes with high accuracy. Clin Cancer Res 2009;15:5494–5502.
Colomo L, Lopez-Guillermo A, Perales M, et al. Clinical impact of the differentiation profile assessed by immunophenotyping in patients with diffuse large B-cell lymphoma. Blood 2003;101:78–84.
Meyer PN, Fu K, Greiner TC, et al. Immunohistochemical methods for predicting cell of origin and survival in patients with diffuse large B-cell lymphoma treated with rituximab. J Clin Oncol 2011;29:200–207.
Muris JJ, Meijer CJ, Vos W, et al. Immunohistochemical profiling based on Bcl-2, CD10 and MUM1 expression improves risk stratification in patients with primary nodal diffuse large B cell lymphoma. J Pathol 2006;208:714–723.
Nyman H, Jerkeman M, Karjalainen-Lindsberg ML, et al. Prognostic impact of activated B-cell focused classification in diffuse large B-cell lymphoma patients treated with R-CHOP. Mod Pathol 2009;22:1094–1101.
Lossos IS, Alizadeh AA, Rajapaksa R, et al. HGAL is a novel interleukin-4-inducible gene that strongly predicts survival in diffuse large B-cell lymphoma. Blood 2003;101:433–440.
Natkunam Y, Lossos IS, Taidi B, et al. Expression of the human germinal center-associated lymphoma (HGAL) protein, a new marker of germinal center B-cell derivation. Blood 2005;105:3979–3986.
Temmins C, Zhao S, Lossos IS, et al. HGAL protein expression persists in disorders of germinal center dissolution: potential role of HGAL in the germinal center microenvironment. Appl Immunohistochem Mol Morphol 2011;19:266–272.
Bacchi MM, Bacchi CE, Alvarenga M, et al. Burkitt's lymphoma in Brazil: strong association with Epstein-Barr virus. Mod Pathol 1996;9:63–67.
Natkunam Y, Zhao S, Mason DY, et al. The oncoprotein LMO2 is expressed in normal germinal-center B cells and in human B-cell lymphomas. Blood 2007;109:1636–1642.
Parker A, Bain B, Devereux S, et al. BCSH guidelines: best practice in lymphoma diagnosis and reporting. Royal College of Pathologists: London, 2010; http://www.bcshguidelines.com/documents/Lymphoma.
Barrans SL, Fenton JA, Banham A, et al. Strong expression of FOXP1 identifies a distinct subset of diffuse large B-cell lymphoma (DLBCL) patients with poor outcome. Blood 2004;104:2933–2935.
Banham AH, Connors JM, Brown PJ, et al. Expression of the FOXP1 transcription factor is strongly associated with inferior survival in patients with diffuse large B-cell lymphoma. Clin Cancer Res 2005;11:1065–1072.
Pan Z, Shen Y, Du C, et al. Two newly characterized germinal center B-cell-associated genes, GCET1 and GCET2, have differential expression in normal and neoplastic B cells. Am J Pathol 2003;163:135–144.
Montes-Moreno S, Roncador G, Maestre L, et al. Gcet1 (centerin), a highly restricted marker for a subset of germinal center-derived lymphomas. Blood 2008;111:351–358.
Gutierrez-Garcia G, Cardesa-Salzmann T, Climent F, et al. Gene-expression profiling and not immunophenotypic algorithms predicts prognosis in patients with diffuse large B-cell lymphoma treated with immunochemotherapy. Blood 2011;117:4836–4843.
Morton LM, Cerhan JR, Hartge P, et al. Immunostaining to identify molecular subtypes of diffuse large B-cell lymphoma in a population-based epidemiologic study in the pre-rituximab era. Int J Mol Epidemiol Genet 2011;2:245–252.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Gualco, G., Bacchi, L., Domeny-Duarte, P. et al. The contribution of HGAL/GCET2 in immunohistological algorithms: a comparative study in 424 cases of nodal diffuse large B-cell lymphoma. Mod Pathol 25, 1439–1445 (2012). https://doi.org/10.1038/modpathol.2012.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.119
Keywords
This article is cited by
-
MEF2B is a member of the BCL6 gene transcriptional complex and induces its expression in diffuse large B-cell lymphoma of the germinal center B-cell-like type
Laboratory Investigation (2019)
-
RNA expression profiling in depressed patients suggests retinoid-related orphan receptor alpha as a biomarker for antidepressant response
Translational Psychiatry (2015)
-
New developments in the pathology of malignant lymphoma. A review of the literature published from January 2012–July 2012
Journal of Hematopathology (2012)