Abstract
Mucinous adenocarcinoma is an uncommon type of endometrial adenocarcinoma for which precursor lesions have yet to be clarified. During a review of noncancerous endometrial lesions in postmenopausal women, we found that mucinous endometrial glands showed variable degrees of epithelial changes that ranged from the formation of simple tubular glands to the formation of complex glands with papillary tufts, and some of the glands with papillary tufts were architecturally similar to low-grade mucinous adenocarcinomas. Based on histological similarities, we have postulated that mucinous metaplasia could be a precursor lesion of mucinous adenocarcinoma. To explain the pathogenetic significance of endometrial mucinous metaplasia, we analyzed the immunohistochemical expression of ER, PR, MKI67, PTEN, β-catenin, P16INK4A, TP53, and PAX2 in 21 endometrial mucinous metaplasias, screened for KRAS (n=16) and PTEN (n=14) mutations, and compared expression patterns between samples with simple mucinous glands, those with complex glands having intraglandular papillary tufts, and endometrioid adenocarcinomas. Compared with the surrounding flat mucinous epithelium and simple mucinous metaplasia, the intraglandular papillary tufts associated with papillary mucinous metaplasia were characterized by selectively decreased expression of PAX2 (P=0.029) and PR (P<0.001), and overexpression of P16INK4A (P=0.014). There were no significant differences in the levels of expression of ER, PTEN, β-catenin, TP53, and MKI67 between the two groups. In contrast with endometrioid adenocarcinomas, rates of MKI67 proliferation were very low in both groups. Mutations in KRAS were identified in 89% of cases with papillary mucinous metaplasia, in contrast to 14% in simple mucinous metaplasia (P=0.001). No PTEN mutations were observed in either of the two groups. In conclusions, immunohistochemical and molecular genetic profiling suggest that papillary mucinous metaplasia is a possible precancerous lesion in a subset of endometrial carcinomas.
Similar content being viewed by others
Main
Endometrial carcinoma is classified into two major groups, types I and II, according to clinicopathological features and molecular pathogenetic mechanisms. Most type I tumors are characterized by an endometrioid histology and are frequently associated with PTEN mutations, whereas type II tumors show a serous histology and are frequently associated with the altered expression of TP53 tumor-suppressor genes. Endometrial hyperplasia and endometrial intraepithelial carcinoma are thought to be precursor lesions of type I and II endometrial carcinomas, respectively. However, this simplified classification and their precursor lesions cannot explain the pathogenesis of all endometrial carcinomas.
Mucinous adenocarcinoma, an uncommon type of endometrial adenocarcinoma comprising <10% of endometrial carcinomas, includes specific variants such as low-grade mucinous adenocarcinoma1 and microglandular adenocarcinoma, which simulates microglandular endocervical hyperplasia of the cervix.2, 3, 4, 5 These tumors occur more frequently in postmenopausal or perimenopausal women than in premenopausal women.6, 7 Histologically, the tumors frequently show mild-to-moderate architectural complexity but have bland cytological features compared with most endometrioid adenocarcinomas. Frequently, the obvious malignant features of the tumors are only recognizable by myometrial invasion, lymphovascular involvement, lymph node or omental metastasis, or cervical stromal invasion in hysterectomy specimens.1 By contrast, diagnosis of endometrial mucinous metaplasia is often complicated by cytologically bland but architecturally complex mucinous epithelium. Owing to their bland cytomorphological features and a failure to define clear diagnostic criteria, mucinous adenocarcinoma and mucinous epithelial metaplasia can be mutually misdiagnosed in curettage specimens.
Some series suggested that mucinous epithelial metaplasias were correlated strongly with subsequent carcinomas,8, 9, 10 whereas others insisted that papillary proliferations devoid of malignant nuclear features are more closely related to endometrial metaplasia and mild-to-moderate nuclear atyia is acceptable in the metaplasia without warranting a diagnosis of atypical papillary hyperplasia.11 Thus, biological characteristics of endometrial mucinous metaplasia and its relationship with endometrial mucinous adenocarcinoma should be further clarified to draw a clear distinction between mucinous metaplasia and adenocarcinoma.
During a review of noncancerous endometrial lesions in postmenopausal women, we noted that mucinous metaplasia of the endometrial glands showed variable degrees of epithelial change with or without intraglandular micropapillary tufts. Moreover, some showed complex glandular architecture similar to the characteristics of low-grade mucinous adenocarcinoma.1 These histological similarities raised the suspicion that papillary mucinous metaplasia could be a precancerous lesion of mucinous adenocarcinoma.
In an effort to explain the pathogenetic significance of mucinous metaplasia of the endometrium, we analyzed the immunohistochemical expression of ER, PR, MKI67, PTEN, β-catenin, P16INK4A, TP53, and PAX2 in 21 endometrial mucinous metaplasias, and screened for KRAS (n=16) and PTEN (n=14) mutations in some of the same samples. We compared expression patterns between samples with simple mucinous glands (simple mucinous metaplasia), those with complex glands having intraglandular papillary tufts (papillary mucinous metaplasia), and samples with endometrioid adenocarcinomas.
Materials and methods
Case Selection
We searched the surgical pathology files of the Department of Pathology, at the University of Ulsan Collage of Medicine, Asan Medical Center, Seoul, Korea for noncancerous mucinous endometrial lesions reported over a 3.5-year period (from 1 January 2008 to 30 June 2011). Given that low-grade mucinous adenocarcinomas and mucinous metaplasias of the endometrium occur more frequently in postmenopausal women,6, 9, 12 we restricted our search to data from women aged 50 years or older. From the 360 cases of noncancerous endometrial lesions reviewed by three pathologists (SHY, BHP, and K-RK), we identified 21 endometrial mucinous metaplasias. We used histopathology to classify endometrial lesions as either simple mucinous metaplasia (n=7) or papillary mucinous metaplasia (n=14). Simple mucinous metaplasia referred to cases in which the endometrial glands had a simple tubular shape and were lined by single layer of columnar epithelium and a flat luminal border with mucin-containing cytoplasm. By contrast, papillary mucinous metaplasia referred either to cases showing intraluminally projecting papillary tufts with or without fibrovascular cores, or to the cases showing complex or cribriform mucinous glandular patterns without malignant nuclear features. In one case, where it was difficult to differentiate papillary mucinous metaplasia from mucinous adenocarcinoma because of the complex glandular architecture, a low-to-near-zero MKI67 proliferation index in the mucinous glands was used as the defining feature of noncancerous glands. Ten cases with features of both simple and papillary mucinous metaplasias were classified as papillary mucinous metaplasia.
To compare the cytologic features between the two groups, we analyzed various nuclear features of the glandular epithelium, including nuclear size, the presence or absence of polymorphism, pseudostratification, nucleolar prominence, and mitotic rates per 20 high-power fields. We included four samples of endometrioid adenocarcinoma obtained from hysterectomies (the International Federation of Gynecology and Obstetrics; FIGO grade 1, n=2; FIGO grade 2, n=1; FIGO grade 3, n=1) to compare expression patterns determined using immunohistochemistry.
Clinical information, including the ages of patients, menopausal status, and follow-up results (wherever possible), was obtained from clinical records.
Immunohistochemical Staining
Immunohistochemical staining was performed on formalin-fixed, paraffin-embedded tissue sections, using a Benchmark automatic immunostaining device (Ventana Medical Systems, Tucson, AR, USA). Briefly, 5 μm sections were transferred onto adhesive slides and dried at 62 °C for 30 min. After standard heat-mediated epitope retrieval for 30 min in ethylene diamine tetraacetic acid (pH 8.0) in an autostainer, the samples were incubated with antibodies to ER (1:50; Novocastra Laboratories, Newcastle, UK), PR (1:200; Novocastra Laboratories), PTEN (1:100; Abcam, Cambridge, UK), MKI67 (1:100; Zymed, San Francisco, CA, USA), TP53 (1:250; Epitomics, Burlingame CA, USA), β-catenin (1:400; Pharmingen, Franklin Lakes, NJ, USA), PAX2 (1:10; Pharmingen), and P16INK4A (1:10; Pharmingen). The sections were subsequently incubated with biotinylated anti-mouse immunoglobulins, peroxidase-labeled streptavidin (LSAB kit, DAKO, Glostrup, Denmark), and 3, 30-diaminobenzidine. Negative control samples were generated by omitting the primary antibody. As positive controls, we used normal breast tissue for ER and PR, cervical mucosa showing high-grade cervical intraepithelial neoplasia for P16INK4A and MKI67, normal proliferative phase endometrium for PAX2 and PTEN, and normal tonsil for β-catenin. Slides were counterstained using Harris hematoxylin. Diffuse nuclear expression confined to the glandular epithelium was interpreted as positive for PAX2 and TP53, whereas diffuse nuclear staining in glandular epithelium was considered positive for PTEN, ER, and PR.
Expression levels of PAX2 and PTEN were divided into four scores to stratify the degree of expression. These were defined as follows: 0, no staining; 1, low-intensity staining in <50% of cells; 2, low-intensity staining in >50% of cells; 3, high-intensity staining in >95% of cells.
For the expression of P16INK4A, a score of 0 was assigned to cases showing no expression at all. Expression in <30% of cells in mucinous glands was scored as 1, expression in 30–90% of cells in mucinous glands was scored as 2, and expression in >90% of the cells in mucinous glands was scored as 3.
ER were uniformly expressed in the endometrial stroma in most cases, but decreased in some mucinous endometrial glands. Thus, cases showing a complete loss of ER in mucinous glands were scored as 0, cases with some glands showing partial loss were scored as 1, and cases with all glands and stroma showing diffuse immunopositive staining were scored as 2.
PR were uniformly expressed in the endometrial stroma in most cases, but expression in mucinous endometrial glands was variable. Thus, cases showing a complete loss of PR in mucinous glands were scored as 0, cases where some glands were immunopositive were scored as 1, and cases with diffuse immunopositive staining in all glands and stroma were scored as 2.
The MKI67 labeling index was expressed as a percentage of immunopositivity, although both scores were very low in both groups. For the expression of TP53, complete negativity was scored as 0, expression in <5% of the glandular epithelium as 1, and expression in >5% of the glandular epithelium as 2. Levels of expression of PAX2, P16INK4A, ER, and PR were compared between simple mucinous metaplasia, papillary mucinous metaplasia, and endometrioid adenocarcinomas.
Mutational Analysis
Paraffin-embedded tissues were available for molecular genetic analysis in 16 cases, including nine papillary mucinous metaplasia and seven simple mucinous metaplasia samples. Polymerase chain reaction (PCR) was performed using genomic DNA extracted from each lesion to amplify regions of KRAS flanked by the sites recognized by the following primers: forward, 5′-ACATGTTCTAATATAGTCAC-3′; reverse, 5′-ACAAGATTTACCTCTATTGTTG-3′. All nine exons of PTEN were amplified separately using flanking intronic primers. Primers used for PCR amplification were as follows: exon 1: forward primer, 5′-TTCCATCCTGCAGAAGAAGC-3′, reverse primer, 5′-CAGCCGCAGAAATGGATAC-3′; exon 2: forward primer, 5′-ACTCCAGCTATAGTGGGGAAA-3′, reverse primer, 5′-TTTTCTGTGGCTTAGAAATCTTTT-3′; exon 3: forward primer, 5′-TGATTACTACTCTAAACCCATAGAAGG-3′, reverse primer, 5′-TTGTTTTAGAAGATATTTGCAAGC-3′; exon 4: forward primer, 5′-AAAGATTCAGGCAATGTTTGTT-3′, reverse primer, 5′-TCTCACTCGATAATCTGGATGAC-3′; exon 5: forward primer, 5′-TCCAGTGTTTCTTTTAAATACCTGTT-3′, reverse primer, 5′-GATCCAGGAAGAGGAAAGGAA-3′; exon 6: forward primer, 5′-TTGGCTTCTCTTTTTTTTCTG-3′, reverse primer, 5′-ACATGGAAGGATGAGAATTTC-3′; exon 7: forward primer, 5′-TCATTAAAATCGTTTTTGACAGTTT-3′, reverse primer, 5′-TCTGTCCTTATTTTGGATATTTCTC-3′; exon 8: forward primer #1, 5′-TTAAATATGTCATTTCATTTCTTTTTC-3′, forward primer #2, 5′-ACCAGGACCAGAGGAAACCT-3′, reverse primer #1, 5′-ACACATCACATACATACAAGTC-3′, reverse primer #2, 5′-GACTTGTATGTATGTGATGTGT-3′; exon 9: forward primer, 5′-TGTTCATCTGCAAAATGGAATAA-3′, reverse primer, 5′-CACAATGTCCTATTGCCATTAAA-3′.
Genomic DNA was amplified by PCR in 25-μl reaction volumes containing 100 ng genomic DNA, 0.5 μl of primers, 2.5 μl of × 10 Ex Taq buffer (Mg2+-free), 2 μl of deoxyribonucleotide triphosphate (dNTP) mixture (2.5 mM each), 2 μl of MgCl2 (25 mM), and 0.17 μl of Ex Taq (5 units/μl; TaKaRa Korea Biomedicals, Seoul, Korea). The PCR conditions involved incubation at 5 min at 95 °C for 1 cycle, followed by 40 cycles of denaturation for 15 s at 95 °C, annealing for 40 s at 56 °C (exons 2 and 4), 57 °C (exons 1, 3, 6, 7, and 9), 59 °C (exon 8), or 60 °C (exon 5), and extension for 45 s at 72 °C. The 40 cycles were followed by incubation at 72 °C for 7 min. We loaded 5 μl of the PCR-amplified product onto a 1.8% agarose gel along with 100-base pair (bp) DNA ladder (Bioneer, Daejeon, Korea) as a standard reference, and electrophoresed the samples at 100 V for 30 min in 0.5% Tris-borate-ethylenediamine tetraacetic acid buffer (Bioneer). For purification of PCR-amplified products, 1 μl of exonuclease I (1 unit/μl; USB, Cleveland, OH, USA) was incubated with 1 μl of PCR-amplified product in a 10 μl reaction for 40 min at 37 °C and then for 15 min at 85 °C. Sequencing reactions were performed using 1 μl of treated PCR-amplified product, 1 μl of exonuclease I, 0.5 μl of BigDye ready reaction mix (ABI PRISM BigDye Terminator version 3.1; Applied Biosystems, Foster City, CA, USA), 1.5 μl of × 5 sequencing buffer (ABI PRISM BigDye Terminator version 3.1; Applied Biosystems), 1 μl of primer (1 pmol/μl), and 6 μl of double-distilled H2O. Sequencing conditions were 25 cycles of initial denaturation at 96 °C for 10 s, followed by 50 °C for 5 s and 60 °C for 4 min. For purification, 10 μl of the sequencing products was incubated with 1 μl of 3 M sodium acetate (pH 4.6; Bioneer) at room temperature for 10 min, and centrifuged at 13 000 r.p.m. for 30 min at 25 °C. After centrifugation, the pellets were washed with 200 μl of 70% ethanol and air dried. The purified sequencing products were dissolved in 10 μl of Hi-Di formamide (Applied Biosystems) as the injection solvent. The products were sequenced using an ABI PRISM Genetic Analyzer 3100 automatic DNA sequencer (Applied Biosystems).
Statistical Analysis
Data were analyzed using the software package SPSS version 17.0 for windows (SPSS, Chicago, IL, USA). Immunoexpression patterns and molecular analysis between simple and papillary mucinous metaplasias were compared using Fisher’s exact test. Expression patterns between the papillary tufts in papillary mucinous metaplasia and the surrounding flat mucinous epithelium in the same glands were compared using Fisher’s exact test. A probability (P) value <0.05 was considered statistically significant.
Results
Clinical Findings
The mean ages of patients in papillary and simple mucinous metaplasia groups were 59.6 and 57.6 years, respectively. All patients were postmenopausal. Endometrium was obtained from curettings for 11 patients, a pipelle biopsy for 1 patient, a polypectomy for 1 patient, and a hysterectomy in 8 patients. The clinical reasons for the hysterectomies included uterine prolapse (n=1), leiomyoma (n=3), ovarian tumors (n=2), and endometrioid adenocarcinoma (n=1). In one case, hysterectomy was performed because papillary mucinous metaplasia was diagnosed as complex endometrial hyperplasia. Among the hysterectomy specimens, mucinous metaplasia was either an incidental finding (n=7) or an associated finding (n=1) identified in the vicinity of endometrioid adenocarcinoma as a separated lesion. Three patients were received tamoxifen treatment following breast cancer surgery. During the follow-up period (4–33 months), tumor progression to overt adenocarcinoma was not identified in any of the patients.
Microscopic Features
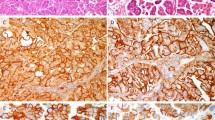
We defined simple mucinous metaplasia by the observation of differently sized simple tubular endometrial glands lined by a single layer of columnar or cuboidal epithelium containing intracytoplasmic mucin. The luminal surface was flat and smooth, with no papillary projections (Figure 1a). Nuclei were uniformly round with finely dispersed chromatin and one or two small conspicuous nucleoli, but no nuclear pleomorphism or mitosis was identified (Figure 1b). Stainings with Alcian blue and d-PAS revealed abundant apical mucin within the glandular epithelium.
Variable morphologies of simple mucinous metaplasia (a, b) and papillary mucinous metaplasia (c–h). Simple mucinous metaplasia is characterized by simple tubular glands lined by a single layer of columnar epithelium with mucin containing cytoplasm (a). Cytologic atypia are not identified (b). Mucinous epithelium in papillary mucinous metaplasia can be slightly elevated above the surrounding flat epithelium (c, arrows) or has prominent intraglandular papillary tufts (d). Papillary projections showing more complex glandular architecture form in a cribriform-like arrangement at the periphery (e, arrow). Squamous metaplasia is often identified beneath the glands (f, arrows). Some cystically dilated simple mucinous glands at the periphery are admixed with glands showing papillary mucinous metaplasia. (g, arrows) The nuclear details of papillary mucinous metaplasia were similar to those of simple mucinous metaplasia showing round uniform nuclei, finely dispersed chromatin, and one or two small conspicuous nucleoli (h).
Papillary mucinous metaplasias were characterized by a spectrum of architectural alterations of the endometrial glands. In some areas, the glandular epithelium was slightly raised above the surrounding flat mucinous epithelium (Figure 1c, arrows), and some showed small distinct papillary tufts with or without fibrovascular cores (Figure 1d). In four cases, cystically dilated glands with intraluminally projecting papillary structures formed a complex cribriform-like glandular arrangement at the periphery of the glands (Figures 1e and f). Squamous metaplasia often formed beneath these glands (Figure 1f, arrows). In 10 cases, simple and papillary mucinous metaplasias were admixed in the same patient (Figure 1g).
The nuclear features of papillary mucinous metaplasia were similar to those of simple mucinous metaplasia, showing round uniform nuclei and finely dispersed chromatin with one or two small conspicuous nucleoli (Figure 1h). The nuclei in both simple and papillary mucinous metaplasia groups were slightly larger than those in the surrounding atrophic glandular epithelium.
Mitotic figures of the glandular epithelium were extremely rare in both simple and papillary mucinous metaplasias. Only a single mitotic figure was identified throughout entire fields in two cases of papillary mucinous metaplasia. Although papillary mucinous metaplasia was characterized by enlarged and variable-sized nuclei, pseudostratification, and a greater frequency of prominent nucleoli than observed in simple mucinous metaplasia, the differences were not statistically significant (Table 1).
Gene Expression, as Determined Using Immunohistochemistry
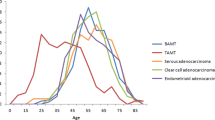
The MKI67 proliferation indices of the glands were extremely low both in simple and papillary mucinous metaplasias, occurring in some glands (Figures 2a and b). The proliferation indices of the glands were not significantly different from those associated with senile atrophy, but are significantly lower than those associated with endometrioid adenocarcinoma. In one case of papillary mucinous metaplasia, in which endometrioid adenocarcinoma was associated as a separate lesion, MKI67 proliferation indices between the two lesions were significantly different, being significantly lower in papillary mucinous metaplasia area (<1%) than in area of endometrioid adenocarcinoma (>60%).
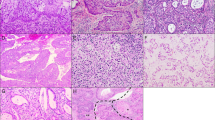
Immunohistochemical expression of MKI67, PAX2, P16INK4A, PR, ER, PTEN, TP53, and β-catenin of simple and papillary mucinous metaplasia. Proliferating indices defined by MKI67 were very low in both groups (a, b). Papillary tufts in papillary mucinous metaplasia showed selectively decreased expressions of PAX2 (d, arrow) and PR (f, arrow) and increased expressions of P16INK4A (h, arrow) compared with simple mucinous metaplasia or surrounding flat mucinous epithelium (c, e, g). Expression of PTEN was decreased both in simple and papillary mucinous metaplasia (k, l). Expression patterns for ER (i, j), TP53 (m, n), and β-catenin (o, p) were not significantly different between simple and papillary mucinous metaplasia.
The distributions and intensities of the expression were significantly different between the simple and papillary mucinous metaplasia groups for PAX2, PR, and P16INK4A, but not for PTEN, ER, TP53, MKI67, and β-catenin (Table 2, Figure 2). We observed that PAX2 was diffusely expressed in all atrophic endometrial glands and glands of simple mucinous metaplasia (Figure 2c), and that PR was expressed in both glands and stroma in most areas of atrophic endometrium and simple mucinous metaplasia (Figure 2e). However, levels of expression of both PAX2 and PR were selectively decreased in the papillary tufts within papillary mucinous metaplasia, compared with levels of expression in the surrounding flat epithelium within the same glands (P=0.029), or with levels of expression in simple mucinous metaplasia (P<0.001) (Figures 2d and f, arrows). P16INK4A was expressed with an intervening pattern in glands of simple mucinous metaplasia, but it was significantly overexpressed in papillary mucinous metaplasia, especially in the intraglandular papillary tufts (Figure 2h, arrow).
There were no significant differences in the distributions or intensities of expression of ER, PTEN, MKI67, TP53, and β-catenin between simple and papillary mucinous metaplasias (Figures 2i–p). We observed diffuse expression of ER in most of the endometrial glands and the stroma in both simple and papillary mucinous metaplasias (Figures 2i and j), although two cases of simple mucinous metaplasia and five cases of papillary mucinous metaplasia were characterized by decreased expression of ER. We noted that PTEN was expressed diffusely in the endometrial stroma in both groups, but only weakly in the entire glandular epithelium, including the flat mucinous epithelium and papillary tufts (Figures 2k and l). The positivity of TP53 was very low in both simple and papillary mucinous metaplasias (Figures 2m and n). β-Catenin showed strong membranous and cytoplasmic staining in both simple and papillary mucinous metaplasias, and there was no difference in the expression patterns between the two groups (Figures 2o and p).
Immunohistochemical expression of PAX2 and P16INK4A in the papillary tufts within papillary mucinous metaplasia samples was significantly different from expression in the surrounding flat mucinous epithelium within the same glands (Table 3).
In the four cases of endometrioid adenocarcinoma, the MKI67 labeling index was >60% of all tumor cells. These four cases were also characterized by complete or partial loss of PAX2 expression and decreased PR expression in glandular epithelium. Expression of P16INK4A in neoplastic glands was noted in 30–50% of all epithelial cells.
Mutational Analysis
The frequency of KRAS mutations was significantly different between simple and papillary mucinous metaplasia samples, being identified in only one of seven simple mucinous metaplasia cases (14%) but in eight of the nine papillary mucinous metaplasia cases tested (89%) (P=0.001, Table 4). Although only one simple mucinous metaplasia case had a glycine-to-alanine substitution at codon 12 (G12A), we identified seven papillary mucinous metaplasia cases with point mutations that caused amino-acid substitutions at codon 12. These comprised three cases with G12V mutations, three with G12D mutations, and one with a G12C mutation (Figure 3a). One papillary mucinous metaplasia case contained a G13D mutation (Figure 3b).
We screened for PTEN mutations in six simple mucinous metaplasia cases and eight papillary mucinous metaplasia cases, but did not identify any PTEN missense mutations in any of the simple and papillary mucinous metaplasia samples, although two cases of the four endometrioid adenocarcinomas tested had R130Q mutations in the PTEN gene.
Discussion
The endometrial epithelium can undergo various types of cellular differentiation toward squamous, mucinous, ciliated, hobnail, and clear cells, as well as papillary changes in both normal and diseased conditions.8, 13 Metaplastic changes can complicate diagnosis, although generally, endometrial lesions with architecturally simple and cytologically bland epithelial changes are considered benign.13 Despite the bland cytologic features of the associated glands, mucinous differentiation may introduce serious diagnostic challenges because it is often associated with a complex papillary or glandular architecture.8, 9, 11, 14 Clear diagnostic criteria to differentiate between mucinous adenocarcinoma and mucinous metaplasia have not been defined. We diagnosed one difficult case showing complex glands and intraglandular papillary tufts as papillary mucinous metaplasia rather than mucinous adenocarcinoma based on almost absent MKI67 proliferation index. In one case in which papillary mucinous metaplasia was associated with a typical endometrioid adenocarcinoma, MKI67 proliferation indices were significantly different between the two lesions. Although complex glandular architecture and bland cytologic features can be seen in both mucinous adenocarcinoma and papillary mucinous metaplasia, we propose that the MKI67 proliferating index can differentiate the two lesions. Nearly absent proliferating cells in the papillary mucinous metaplasia can be interpreted as an oncogene-induced cellular senescence that needs to be overcome during malignant transformation.
Nucci et al8 tried to correlate the architectural complexity of mucinous endometrial glands with data from follow-up studies. They found that whereas normal or complex mucinous lesions with small papillary tufts (type A) in the absence of cytologic atypia had a low risk of progression to invasive carcinoma, lesions with more complex glandular patterns and high-grade cytologic atypia were frequently associated with endometrial carcinomas.8 Most cases of papillary mucinous metaplasia used in our study corresponded to the ‘type A’ category in that previous study,8 although in our study, none progressed to overt carcinoma during the follow-up period. Uneventful follow-up may not necessarily mean that the lesions are not precancerous lesions because the follow-up period in our study, as well as in others, was rather short. Many of the lesions could have been completely removed at the precancerous stage by curettage or hysterectomy.
In the interpretation of endometrial mucinous metaplasia, a three-grading system has been proposed, depending on the presence or absence of architectural complexity and cytologic atypia.8 However, we propose that it can be simplified into two groups, simple and papillary mucinous metaplasia, based on the presence or absence of intraglandular papillary tufts or complex glandular architecture. Although simple mucinous metaplasia is characterized by simple, round glands lined by tall columnar mucinous epithelium, papillary mucinous metaplasia has intraglandular papillary projections with or without fibrovascular cores, or complex glandular architecture at the periphery of cystically dilated glands producing back-to-back arrangements. Cytological features of the two tissue types were not significantly different. Those two groups were well correlated with the absence or presence of genetic changes, including loss of PAX2 and PR, overexpression of P16INK4A, and KRAS mutation.
The tumor-suppressor protein P16INK4A can be overexpressed in proliferating cells in the context of the deregulation of retinoblastoma by human papilloma virus (HPV).15 For this reason, diffuse P16INK4A expression is used as a surrogate marker for high-risk HPV infection, and immunopositivity for P16INK4A in uterine cancers is usually considered as a cervical origin. However, in settings unrelated to either HPV infection or deregulation of Rb, P16ink4A has a function as a negative regulator of cell proliferation, and its expression can be linked to oncogene-induced senescence, causing irreversible growth arrest.16, 17, 18, 19 The induction of P16INK4A in premalignant lesions and its loss during malignant transformation have been demonstrated in carcinogenesis of the liver, lung, and pancreas.16, 17, 18, 19 In the previous study,1 P16INK4A expression was completely lost in 50% of low-grade mucinous adenocarcinomas, and the remaining cases showed very patchy expression.1 In our study, P16INK4A was specifically expressed in papillary tufts, and not in the surrounding flat mucinous epithelium. Its expression tended to be inversely correlated with an expression of PR and PAX2, suggesting that papillary tufts may be a site of initiation of tumorigenesis.
PAX2 is a transcription factor that controls the development of the kidney, organs deriving from the mesonephric (Wolffian) duct, and organs related to the Mullerian duct.20, 21 In contrast to the loss of PAX2 expression in other normal adult tissues, persistent expression of PAX2 in normal endometrial glands suggested that this transcription factor may have an important role in normal endometrial proliferation and self-renewal.20 Monte et al22 reported that the concomitant loss of PAX2 and PTEN expression is common in precancerous lesions (31%) and carcinomas (55%) of the endometrium, indicating that PAX2 is a relatively new biomarker recognizing neoplastic endometrial lesions.
The guanine nucleotide-binding protein KRAS has a role in the regulation of cell growth and differentiation.23 Mutations in KRAS are early events in tumorigenesis, and commonly occur in tumors showing mucinous differentiation in various organs, including the pancreas (90%), colon (50%), thyroid (50%), and lung (30%).24 Mutated KRAS is more frequent in ovarian mucinous borderline tumors or carcinomas (75%) than in serous carcinomas (20%) or other non-mucinous ovarian tumors (14%).25 These results suggest that KRAS mutations are closely correlated with a mucinous differentiation of neoplastic epithelium. When KRAS mutations are associated with PTEN mutations, neoplastic glands frequently result in endometrioid glandular morphology, as seen in endometrial hyperplasias, endometrial intraepithelial neoplasia lesions, and endometrioid adenocarcinoma.26, 27, 28 In our study, PTEN mutations were not observed in any cases, which may suggest that papillary mucinous metaplasia is not a direct precursor lesion of endometrioid adenocarcinoma. Nevertheless, papillary mucinous metaplasia may have some correlation with endometrioid adenocarcinoma, because one case of papillary mucinous metaplasia was associated endometrioid adenocarcinoma as separate lesion in the same patient and three patients had received tamoxifen treatment following breast cancer surgery. Moreover, progesterone receptors were specifically lost in the intraglandular papillary tufts of papillary mucinous metaplasia samples.
In conclusion, the high incidence of KRAS mutations in papillary mucinous metaplasia, in association with overexpression of P16INK4A and loss of PAX2 and PR expression in intraglandular papillary tufts, suggest that papillary mucinous metaplasia may be a precancerous lesion of a certain subset of mucinous adenocarcinoma of the endometrium. Based on the overlapping histopathologic features between simple and papillary mucinous metaplasias, and the lower frequency of genetic changes in the simple mucinous metaplasia, simple mucinous metaplasia might be a precursor of papillary mucinous metaplasia. However, for the progression of papillary mucinous metaplasia into the overt adenocarcinoma, the senescence barrier associated with the low proliferation indices in these complex glandular structures may need to be overcome by further genetic alterations.
References
Fujiwara M, Longacre TA . Low-grade mucinous adenocarcinoma of the uterine corpus: a rare and deceptively bland form of endometrial carcinoma. Am J Surg Pathol 2011;35:537–544.
Young RH, Scully RE . Uterine carcinomas simulating microglandular hyperplasia. A report of six cases. Am J Surg Pathol 1992;16:1092–1097.
Qiu W, Mittal K . Comparison of morphologic and immunohistochemical features of cervical microglandular hyperplasia with low-grade mucinous adenocarcinoma of the endometrium. Int J Gynecol Pathol 2003;22:261–265.
Zaloudek C, Hayashi GM, Ryan IP, et al. Microglandular adenocarcinoma of the endometrium: a form of mucinous adenocarcinoma that may be confused with microglandular hyperplasia of the cervix. Int J Gynecol Pathol 1997;16:52–59.
Giordano G, D’Adda T, Gnetti L, et al. Endometrial mucinous microglandular adenocarcinoma: morphologic, immunohistochemical features, and emphasis in the human papillomavirus status. Int J Gynecol Pathol 2006;25:77–82.
Melhem MF, Tobon H . Mucinous adenocarcinoma of the endometrium: a clinico-pathological review of 18 cases. Int J Gynecol Pathol 1987;6:347–355.
Young R, Scully R . Uterine carcinomas simulating microglandular hyperplasia. A report of six cases. Am J Surg Pathol 1992;16:1092–1097.
Nucci MR, Prasad CJ, Crum CP, et al. Mucinous endometrial epithelial proliferations: a morphologic spectrum of changes with diverse clinical significance. Mod Pathol 1999;12:1137–1142.
Mount SL . Mucinous metaplasias of the endometrium: biologically meaningful subsets for the practicing surgical pathologist. Adv Anat Pathol 2000;7:197–200.
Nicolae A, Preda O, Nogales FF . Endometrial metaplasias and reactive changes: a spectrum of altered differentiation. J Clin Pathol 2011;64:97–106.
Lehman MB, Hart WR . Simple and complex hyperplastic papillary proliferations of the endometrium: a clinicopathologic study of nine cases of apparently localized papillary lesions with fibrovascular stromal cores and epithelial metaplasia. Am J Surg Pathol 2001;25:1347–1354.
Fukunaga M . Mucinous endometrial adenocarcinoma simulating microglandular hyperplasia of the cervix. Pathol Int 2000;50:541–545.
Hendrickson MR, Kempson RL . Endometrial epithelial metaplasias: proliferations frequently misdiagnosed as adenocarcinoma. Report of 89 cases and proposed classification. Am J Surg Pathol 1980;4:525–542.
Vang R, Tavassoli FA . Proliferative mucinous lesions of the endometrium: analysis of existing criteria for diagnosing carcinoma in biopsies and curettings. Int J Surg Pathol 2003;11:261–270.
von Knebel Doeberitz M . New markers for cervical dysplasia to visualise the genomic chaos created by aberrant oncogenic papillomavirus infections. Eur J Cancer 2002;38:2229–2242.
Gutierrez-Reyes G, del Carmen Garcia de Leon M, Varela-Fascinetto G, et al. Cellular senescence in livers from children with end stage liver disease. PLoS One 2010;5:e10231.
Dankort D, Filenova E, Collado M, et al. A new mouse model to explore the initiation, progression, and therapy of BRAFV600E-induced lung tumors. Genes Dev 2007;21:379–384.
Bennecke M, Kriegl L, Bajbouj M, et al. Ink4a/Arf and oncogene-induced senescence prevent tumor progression during alternative colorectal tumorigenesis. Cancer Cell 2010;18:135–146.
Abe K, Suda K, Arakawa A, et al. Different patterns of p16INK4A and p53 protein expressions in intraductal papillary-mucinous neoplasms and pancreatic intraepithelial neoplasia. Pancreas 2007;34:85–91.
Zhai QJ, Ozcan A, Hamilton C, et al. PAX-2 expression in non-neoplastic, primary neoplastic, and metastatic neoplastic tissue: a comprehensive immunohistochemical study. Appl Immunohistochem Mol Morphol 2010;18:323–332.
Dahl E, Koseki H, Balling R . Pax genes and organogenesis. Bioessays 1997;19:755–765.
Monte NM, Webster KA, Neuberg D, et al. Joint loss of PAX2 and PTEN expression in endometrial precancers and cancer. Cancer Res 2010;70:6225–6232.
Malumbres M, Barbacid M . RAS oncogenes: the first 30 years. Nat Rev Cancer 2003;3:459–465.
Bos JL . ras oncogenes in human cancer: a review. Cancer Res 1989;49:4682–4689.
Enomoto T, Weghorst CM, Inoue M, et al. K-ras activation occurs frequently in mucinous adenocarcinomas and rarely in other common epithelial tumors of the human ovary. Am J Pathol 1991;139:777–785.
Hecht JL, Mutter GL . Molecular and pathologic aspects of endometrial carcinogenesis. J Clin Oncol 2006;24:4783–4791.
Lax SF, Kendall B, Tashiro H, et al. The frequency of p53, K-ras mutations, and microsatellite instability differs in uterine endometrioid and serous carcinoma: evidence of distinct molecular genetic pathways. Cancer 2000;88:814–824.
Jarboe EA, Mutter GL . Endometrial intraepithelial neoplasia. Semin Diagn Pathol 2010;27:215–225.
Acknowledgements
This study was supported by a grant from the Asan institute for Life Sciences (2011-230), Seoul, Korea, and an NRF grant funded by the Ministry of Education, Science and Technology (2011-0026130).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Yoo, S., Park, B., Choi, J. et al. Papillary mucinous metaplasia of the endometrium as a possible precursor of endometrial mucinous adenocarcinoma. Mod Pathol 25, 1496–1507 (2012). https://doi.org/10.1038/modpathol.2012.113
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.113
Keywords
This article is cited by
-
A 2-tier subdivision of papillary proliferations of the endometrium (PPE) only emphasizing the complexity of papillae precisely predicts the neoplastic risk and reflects the neoplasia-related molecular characteristics—a single-centered analysis of 207 cases
Virchows Archiv (2022)
-
Emerging relationships between papillary proliferation of the endometrium and endometrial carcinoma: evidence from an immunohistochemical and molecular analysis
Virchows Archiv (2019)
-
Benign endometrial proliferations mimicking malignancies: a review of problematic entities in small biopsy specimens
Virchows Archiv (2018)
-
Long-term effects of repeated superovulation on the uterus and mammary gland in rhesus monkeys
Journal of Assisted Reproduction and Genetics (2017)
-
Frequent KRAS mutation in complex mucinous epithelial lesions of the endometrium
Modern Pathology (2014)