Abstract
Chromosomal rearrangements leading to constitutive activation of anaplastic lymphoma receptor tyrosine kinase (ALK) define a category of lung adenocarcinomas that may be amenable to targeted therapy with the ALK inhibitor crizotinib. Defining distinctive features of ALK-rearranged (ALK+) lung adenocarcinomas may help identify cases that merit molecular testing. However, data describing the morphologic features of ALK+ lung adenocarcinomas are conflicting and are primarily based on analysis of resected primary lung tumors. It is unclear whether the findings from prior studies are applicable to metastatic lung tumors or to small biopsy/cytology specimens. To address these issues, we examined resection, excision, small biopsy, and cytology cell block specimens from 104 ALK+ and 215 ALK− lung adenocarcinomas from primary and metastatic sites. All cases were evaluated for ALK rearrangements by fluorescence in situ hybridization. The predominant histologic subtypes and distinctive cytomorphologic features were assessed in each case. Primary ALK+ lung adenocarcinomas showed a significant association with solid, micropapillary, and papillary-predominant histologic patterns and tumor cells with a signet ring or hepatoid cytomorphology. Among metastatic lung tumors and small biopsy/cytology specimens, the only distinguishing morphologic feature of ALK+ tumors was the presence of signet ring cells. Based on these results, we developed a morphology-based scoring system for predicting ALK rearrangements in lung adenocarcinomas. The scoring system predicted ALK rearrangements in a new cohort of 78 lung adenocarcinomas (29 ALK+ and 49 ALK−) with a sensitivity of 88% and a specificity of 45%. In conclusion, ALK+ lung adenocarcinomas have distinctive morphologic features, with signet ring cells showing a significant association with ALK rearrangements irrespective of tumor site (primary vs metastatic) or specimen type. However, morphologic screening alone will not detect a minority of ALK+ lung adenocarcinomas, and the routine use of ancillary studies may be warranted to identify all patients who may benefit from crizotinib treatment.
Similar content being viewed by others
Main
Lung cancer remains a leading cause of cancer-related mortality worldwide.1 Although cancer is known to develop by the accumulation of complex genetic and epigenetic changes, in some cases the malignant phenotype appears to be dependent on the activity of critical oncogenic signaling pathways.2 The development of therapeutic agents capable of targeting the activity of specific oncoproteins has prompted efforts to classify lung cancers according to the genetic changes that activate these signaling pathways. In 2007, two groups independently identified a subset of lung adenocarcinomas harboring chromosomal translocations involving the anaplastic lymphoma receptor tyrosine kinase (ALK) gene.3, 4 Many of the cases of lung adenocarcinoma with ALK rearrangements involve a paracentric inversion affecting chromosome 2p21 and 2p23 that results in a fusion between the 5′ portion of the echinoderm microtubule-associated protein like 4 (EML4) gene and the 3′ portion of the ALK gene. The EML4–ALK fusion results in dimerization and ligand-independent activation of the ALK tyrosine kinase domain, leading to constitutive engagement of downstream signaling pathways that promote cell survival and proliferation, such as the JAK3/STAT3, PI3K/AKT, and Ras/Mek/Erk pathways.5 A recent phase I clinical trial of crizotinib, a small-molecule tyrosine kinase inhibitor with potent activity against ALK, demonstrated a significant objective response rate in patients with lung adenocarcinomas harboring ALK rearrangements.6 Subsequently, crizotinib was approved by the US Food and Drug Administration (FDA) to treat locally advanced or metastatic ALK+ lung adenocarcinomas. Thus, the identification of ALK rearrangements is emerging as an important component of the pathologic analysis of lung adenocarcinomas.
Given the FDA approval of crizotinib with a companion diagnostic test—fluorescence in situ hybridization (FISH) using the Vysis ALK Break Apart FISH Probe Kit (Abbott Molecular)—ALK FISH has been firmly established as the gold standard for detecting ALK rearrangements in the United States. However, it is currently impractical for most pathology laboratories to screen all lung adenocarcinoma specimens for ALK rearrangements using FISH (College of American Pathologists (CAP)/International Association for the Study of Lung Cancer (IASLC)/Association for Molecular Pathology (AMP) Lung cancer biomarkers guideline draft recommendations), as ALK rearrangements reportedly occur in only 2–7% of lung adenocarcinomas6 and the cost of ALK FISH is approximately $1500. Therefore, recognizing distinctive clinicopathologic features of ALK+ lung carcinomas may help oncologists and pathologists enrich for cases that will be positive for ALK rearrangements by molecular testing. Some features previously reported to be associated with ALK rearrangements include young age of onset, reduced smoking history, advanced stage at presentation, adenocarcinoma histology, and mutual exclusivity with activating mutations in EGFR and KRAS.4, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16
In spite of the common findings among the above studies, the results of detailed pathologic analyses have varied. Previously, our microscopic analysis of 20 ALK+ lung adenocarcinomas revealed a strong association with a solid-predominant architecture and the presence of signet ring cells with intracytoplasmic mucin vacuoles and peripherally displaced and flattened nuclei.11 This study included a variety of specimen types with the majority consisting of biopsies of both primary and metastatic tumors. In contrast, morphologic analysis of resected primary ALK+ lung adenocarcinomas from a predominantly Asian patient cohort identified acinar-predominant architecture and abundant mucin production as morphologic features significantly associated with ALK rearrangements.8, 13, 17 It is unclear whether these conflicting results are due to differences in tumor stage (early vs advanced), specimen source (primary vs metastatic tumor), or ethnicity in the study populations. Furthermore, at least 70% of patients with lung cancer present at an advanced stage with unresectable disease.18 In these patients, tumors are frequently sampled from either primary or metastatic sites by minimally invasive procedures such as transthoracic and endobronchial biopsies, and the pathologic diagnosis must be made on limited amounts of tissue.18 Therefore, any histologic and cytologic screening criteria for ALK rearrangements in lung adenocarcinomas must be applicable to specimens from metastatic sites as well as small samples. To address these issues, we performed a detailed cytologic and histologic analysis of the largest cohort of ALK+ tumors reported to date and assessed whether any distinctive features associated with ALK rearrangements could be extended to metastatic tumors and small biopsy/cytology specimens.
Materials and methods
Study Design and Case Selection
This study was approved by the Massachusetts General Hospital (MGH) Institutional Review Board. The study consisted of two phases. The purpose of the first phase of the study was to identify histologic and cytologic features significantly associated with ALK+ lung adenocarcinomas. Our study group consisted of 319 cases of lung adenocarcinoma that had been genotyped by the MGH Molecular Pathology Laboratory, 104 of which were ALK+ and 215 of which were ALK−. ALK rearrangements were detected using FISH, as described below. In most cases, the presence of mutations in other cancer genes was determined by direct sequencing or with the SNaPshot genotyping platform.19 The 104 ALK+ cases included primary lung tumors (n=54) and lung tumors sampled from metastatic sites (n=44). In six of those referred from outside institutions, we could not determine whether the biopsy was taken from a primary or metastatic site. The specimen types varied and consisted of lung resections (n=29) or excisions of metastatic deposits (n=25) and small biopsy (n=40) or cytology (n=10) specimens. The 215 ALK− cases also included primary lung tumors (n=172), lung tumors from metastatic sites (n=43), resections of the lung primary (n=145), excisions of metastases (n=16), and small biopsy (n=33) or cytology specimens (n=7). In 14 ALK− cases, both small biopsy and cell block material were available for review. Please see Supplementary Table S1 for a detailed breakdown of small biopsy and cytology specimen types. For patients whose medical records were available for review, we collected clinical data including sex, age at the time of specimen procurement, smoking history, and clinical stage of disease.
On the basis of the findings from the first phase of the study, we developed a two-tier scoring system for predicting the presence of ALK rearrangements in lung adenocarcinomas. The scoring system was based on a combination of cytologic and histologic features as well as specimen type and was designed to classify cases as having a low vs high probability of harboring ALK rearrangements. We tested the scoring system on 78 additional cases of lung adenocarcinoma that consisted of 29 ALK+ and 49 ALK− lung cancer specimens. Of these, 60 cases represented samples of primary lung tumors (21 ALK+ and 39 ALK−), and 18 cases represented samples from metastatic sites (8 ALK+ and 10 ALK−).
Of note, almost all lung adenocarcinomas have been screened for ALK rearrangements by FISH (reflex testing) at our hospital since 2009. Although we did not prescreen patients before testing for ALK rearrangements, both testing and validation cohorts were enriched for ALK+ cases most likely due to the fact that our hospital and molecular pathology laboratory have served as a referral center and a central laboratory, respectively, for the enrollment of patients in the clinical trials investigating the ALK inhibitor crizotinib.
Morphologic Analysis
In the first phase of the study, two of the authors (MMK, and MN or VEK) jointly performed comprehensive histologic subtyping of 319 lung adenocarcinomas, based on recommendations by the recent classification strategy proposed by the IASCLC, American Thoracic Society (ATS), and European Respiratory Society (ERS).18 In brief, we semiquantitatively determined the proportion of any particular histologic pattern in 10% increments and recorded the predominant histologic pattern (lepidic, acinar, papillary, micropapillary, solid, invasive mucinous adenocarcinoma, or the other variants). In light of the recent report that ALK+ tumors are strongly associated with the presence of abundant extracellular mucin and a cribriform pattern (together comprising the ‘mucinous cribriform’ pattern), we also examined each of our cases for the presence of extracellular mucin and cribriform architecture (counted in the acinar category for histologic subtyping). Tumors that showed both extracellular mucin and cribriform architecture were noted to have a mucinous cribriform component; these cases were recorded as a subcategory of tumors with a cribriform component.15 We also noted the presence of necrosis and calcifications (including psammoma bodies). For each case, we also applied a three-tier scoring system for nuclear grade (low, intermediate, and high grade) and recorded the highest grade for the analysis.20 Additional cytologic features that were recorded include the presence of tumor cells with signet ring or hepatoid (exhibiting abundant cytoplasm, round nuclei, and conspicuous nucleoli) morphology. The percentage of tumors involved by signet ring cells was assessed semiquantitatively into three tiers: none, present but <10%, and ⩾10%. In the 14 ALK− cases in which both biopsy and cell block specimens were available, both specimen types were used to render an overall assessment of morphologic features.
In the second phase of the study, hematoxylin and eosin-stained slides were reviewed with the authors being blinded to the results of ALK FISH for all cases. Two of the authors (MMK and MN) scored each slide for parameters that were determined to be predictive of ALK rearrangements during the first phase of the study, including predominant histologic subtype, signet ring cells, hepatoid cells, and specimen type (resection/excision vs small biopsy specimen).
In Situ Hybridization
FISH was performed on 5-μm sections of formalin-fixed paraffin-embedded tissues. The area of the slide enriched for tumor cells was selected based on review of a corresponding hematoxylin and eosin-stained section. A dual-color break apart probe specific for the ALK locus on chromosome 2p23 (Vysis LSI ALK Break Apart FISH Probe, Abbott Molecular, Abbott Park, IL, USA) was hybridized according to the manufacturer's protocol, and at least 50 tumor cells were scored for the presence of split signals. A case was considered positive for ALK rearrangement if >15% of cells showed split signals.
Statistical Analysis
In the first phase of the study, Fisher's exact test and Wilcoxon rank-sum test were used to compare categorical and continuous clinicopathologic data, respectively, between ALK+ and ALK− cases. Univariate analysis was performed on each of the following groups: lung adenocarcinomas from primary site; lung adenocarcinomas from metastatic sites; ‘large’ specimens (resections of primary tumors and excisional biopsies of metastatic tumors); and ‘small’ biopsy and cytology specimens. The specimen type was included as a covariate in the data analysis of both primary and metastatic lung adenocarcinomas, given the notion that the amount and quality of tissue obtained by a particular type of procedure may influence the cytomorphologic evaluation of the specimen. For the second phase of the study, morphologic factors associated with a P-value ≤0.05 in the univariate analysis of primary tumors (predominant histologic subtype, presence of signet ring cells, hepatoid cytology, and specimen type) were assessed by logistic regression in the multivariate analysis. Backward elimination was used to identify independently significant factors based on a removal criterion at the P=0.05 level. Although univariate analysis showed a significant difference in the presence of psammoma bodies and calcifications between ALK+ and ALK− primary tumors, this variable was excluded from the regression model because of numerical constraints as only one ALK− case demonstrated psammoma bodies and calcifications. On the basis of the final regression model, a scoring system was developed by assigning points to each predictive factor proportional to the magnitude of their parameter estimate. All P-values were based on two-sided hypothesis tests, and the computations were performed using SAS 9.2 (SAS Institute, Cary, NC, USA).
Results
Clinicopathologic Features of ALK+ Lung Adenocarcinomas
The clinical features of the ALK+ and ALK− cases are summarized in Table 1. Comprehensive demographic data were not available for the subset of ALK+ specimens that were submitted to the MGH Molecular Pathology Laboratory exclusively for molecular testing with incomplete clinical information. Of the cases with clinical data available, ALK+ tumors were associated with a younger age at presentation, higher stage at diagnosis, and reduced history of smoking compared with patients with ALK− tumors, in line with our previous report.12 Patients with ALK+ tumors had an age range of 21–86 years and mean and median ages of 52 and 55 years, respectively (compared with mean age of 64 years and median age of 65 years for patients with ALK− tumors, P<0.0001). Of the 81 patients with ALK+ tumors and available clinical staging data, 69 (85%) presented at advanced stage (IIIB or IV), compared with 30% (64/214) of patients with ALK− tumors and available clinical staging data (P<0.0001). A smoking history was available for 39 patients with ALK+ and 214 patients with ALK− tumors. Of the 39 patients with ALK+ tumors and an available smoking history, 69% (27/39) were never smokers with a lifetime history of smoking <100 cigarettes, 10% (4/39) were light smokers with 10 pack-years or less of smoking, and 21% (8/39) were smokers with >10 pack-years of smoking. In contrast, for the 214 patients with ALK− tumors, only 20% (42/214) were never smokers, 13% (27/214) were light smokers, and 67% (145/214) were smokers (P<0.0001). ALK rearrangements were not significantly associated with sex. Of the 53 ALK+ specimens for which clinical data were available, 47% (25/53) were from male and 53% (28/53) were from female patients. For ALK− tumors, 40% (85/215) were from male and 60% (130/215) were from female patients (P=0.3508).
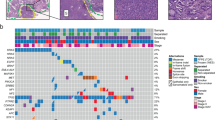
Molecular Profiles of Cases Examined in the Study
The molecular profiles of 104 ALK+ and 215 ALK− lung adenocarcinomas examined in the study are summarized in Supplementary Table S2. In all ALK+ cases, no concurrent activating mutations in EGFR or KRAS were detected. Among ALK− cases, activating mutations in EGFR were identified in 44 cases, and activating mutations in KRAS were detected in 70 cases. Tumors with no ALK rearrangements or activating mutations in EGFR or KRAS comprised 99 of the cases. In two ALK− cases, the status of EGFR or KRAS mutations was unknown. Among the ALK− cases, activating and sometimes concurrent mutations in CTTNB1 (beta-catenin, n=7), TP53 (n=8), PIK3CA (phosphatidylinositol 3-kinase, n=7), ERBB2 (human epidermal growth factor receptor 2, n=2), and BRAF (n=3) were also detected.
Morphologic Features of ALK+ Lung Adenocarcinomas
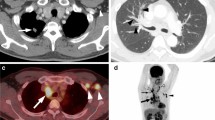
The morphologic features of ALK+ and ALK− primary lung tumors are summarized in Table 2. Among primary lung tumors, a solid-predominant histology (Figures 1a and b) was seen in 44% of ALK+ tumors (compared with only 16% in ALK− tumors, P<0.0001), and a micropapillary-predominant histology (Figure 1c) was seen in 22% of ALK+ tumors (compared with only 9% in ALK− tumors, P=0.0175). In contrast, ALK+ tumors were less likely to show acinar-predominant (15%, compared with 35% in ALK− tumors, P=0.0063), lepidic (formerly non-mucinous bronchioloalveolar)-predominant (7%, compared with 23% in ALK− tumors, P=0.0158), and invasive mucinous adenocarcinoma (formerly mucinous bronchioloalveolar)-predominant (0%, compared with 8% in ALK− tumors, P=0.0417) patterns.
Morphology of lung adenocarcinomas harboring ALK rearrangements. (a) Solid pattern with signet ring cells in a primary lung adenocarcinoma. Inset shows cells with intracytoplasmic mucin and peripherally displaced nuclei (hematoxylin and eosin; enlarged in inset). (b) Solid pattern with hepatoid tumor cells in a primary lung adenocarcinoma. Inset shows cells with abundant eosinophilic cytoplasm, round nuclei, and prominent nucleoli (hematoxylin and eosin; enlarged in inset). (c) Micropapillary and (d) papillary patterns in a primary lung adenocarcinoma (hematoxylin and eosin). (e) Papillary pattern with hepatoid tumor cells and focal signet ring cells (arrows) in a primary lung adenocarcinoma. Abundant extracellular mucin is present in this case (hematoxylin and eosin). (f) Solid pattern with signet ring cells in metastatic lung adenocarcinoma in a mediastinal lymph node, sampled by fine needle aspiration biopsy (hematoxylin and eosin).
ALK+ tumors were also associated with distinctive cytologic features. Among primary lung tumors, 72% of ALK+ tumors showed at least partial involvement by signet ring cells (Figures 1a, e, and f). In contrast, only 15% of ALK− primary tumors showed any signet ring cells (P<0.0001). The majority (54%) of ALK+ tumors with signet ring cells demonstrated a solid-predominant pattern, but other histologic patterns, including micropapillary (18%), acinar (15%), papillary (8%), and lepidic (5%) predominant patterns, were also seen in ALK+ tumors with signet ring cells. Signet ring cells comprised 10% or more of the examined tumor cells in 35% of ALK+ but only 2% of ALK− primary lung tumors (P<0.0001).
Among primary lung cancer specimens, 15 (28%) of ALK+ tumors contained at least a focal population of hepatoid tumor cells with abundant eosinophilic cytoplasm, round nuclei, and prominent nucleoli (Figures 1b and e). These hepatoid features were seen in a predominantly solid architectural pattern in 9 of these 15 (60%) cases. Conversely, only 6% of ALK− tumors exhibited hepatoid cytomorphology (P<0.0001). ALK rearrangements were also significantly associated with the presence of psammoma bodies (P<0.0001) and lower nuclear grade (P=0.0427) in primary lung tumors. Conversely, neither the presence of extracellular mucin nor cribriform glands was a predictor of ALK rearrangements in our cohort.
Among metastatic tumors, the only significant morphologic feature associated with ALK rearrangements was the presence of signet ring cells, with 71% of ALK+ metastases showing at least focal signet ring cells (compared with 21% of ALK− metastases, P<0.0001) and 30% of ALK+ metastases showing abundant signet ring cells comprising 10% or more of the tumor (compared with 5% of ALK− metastases, P=0.0034) (Table 3). Predominant histologic subtype, hepatoid cytology, and the presence of psammoma bodies were not significantly different between ALK+ and ALK− lung adenocarcinomas from metastatic sites.
Next, we determined whether any of these morphologic features were distinguishable on the subset of specimens procured by minimally invasive procedures, including endobronchial and transthoracic biopsies, core biopsies of metastatic disease in lymph node, bone, and soft tissue, and cell blocks of fine needle aspiration biopsies and pleural fluid. In these ‘small’ specimens, the only significant morphologic feature associated with ALK rearrangement was the presence of signet ring cells (Supplementary Table S3). The predominant histologic pattern of the tumor, the presence of hepatoid tumor cells, and the presence of psammoma bodies were not significant factors distinguishing ALK+ from ALK− tumors in these small specimens.
Multivariate Analysis and Morphologic Model for Predicting ALK Rearrangements
We next used multivariate data modeling on our analysis of primary lung tumors to identify variables that could independently predict the presence of ALK rearrangements. The multivariate analysis identified the presence of signet ring cells, micropapillary-predominant histology, and hepatoid tumor cells as the most predictive independent factors of ALK rearrangements. Solid- and papillary-predominant histology (Figures 1d and e) and small biopsy specimens were also significant independent factors predictive of ALK status. With respect to specimen type, ‘small’ specimens such as endobronchial biopsies, CT-guided core biopsies, and cytology specimens comprised 48% of ALK+ tumors but only 25% of ALK− tumors in our study (P<0.001). The association between specimen type and ALK rearrangements likely reflects the fact that patients with ALK+ tumors frequently present at an advanced stage with unresectable disease12 and are more likely to be diagnosed by minimally invasive biopsies rather than excision or resection specimens.
On the basis of the multivariate analysis, we developed a scoring system in which variables were assigned points proportional to their estimated ability to predict ALK rearrangements (Table 4). To optimize the sensitivity of the scoring system in detecting patients who may benefit from molecular testing, cases with a total score of 2.5 points or higher were considered ‘highly probable’ for having ALK rearrangements, corresponding to predicted probability >10%. With this threshold, a ‘highly probable’ score was associated with ALK rearrangements with sensitivity of 89% and specificity of 75% in our group of 226 primary lung tumors.
We validated the scoring system on a new cohort of 78 lung adenocarcinoma cases (29 ALK+, 49 ALK−) that had undergone FISH analysis for ALK rearrangements. These cases consisted of 60 primary lung tumors and 18 metastatic tumors. Small biopsy specimens comprised 31 of the cases. Two pathologists blinded to the status of ALK rearrangements independently applied the scoring system to each case. The scoring system predicted ALK rearrangements with an average sensitivity of 88%, specificity of 45%, positive predictive value (PPV) of 49%, and negative predictive value (NPV) of 87% (Table 5). Subset analysis revealed that the scoring system showed high sensitivity for predicting ALK+ tumors in primary tumors (88%) and small biopsy specimens (93%). Interestingly, although the scoring system was based on multivariate analysis of primary tumors, it predicted ALK rearrangements in metastatic tumors with sensitivity comparable to that of primary tumors (88%).
We examined whether the detection of signet ring cells was also predictive of ALK rearrangements in the validation cases. Overall, the detection of signet ring cells showed a lower sensitivity but higher specificity for predicting ALK rearrangements compared with the multivariate model-based scoring system (Table 5). Subset analysis showed similar values for sensitivity and specificity for primary and metastatic tumors as well as small biopsy specimens. Semiquantitative assessment of the percentage of signet ring cells in each tumor showed that the presence of at least 10% signet ring cells in a tumor predicted ALK rearrangements with a high specificity (92%) but low sensitivity (31%). This direct relationship between the amount of tumor composed of signet ring cells and specificity for ALK rearrangements was preserved in the subset analyses of primary, metastatic, and small biopsy samples.
Discussion
Our analysis of a large cohort of primary and metastatic lung adenocarcinomas confirms that chromosomal rearrangements involving the ALK gene are associated with distinctive morphologic features that may be helpful in selecting specimens for more definitive molecular testing, especially when available tissue samples are limited. Multivariate analysis identified specimen type, the presence of signet ring and hepatoid cytomorphology, and micropapillary-, solid-, or papillary-predominant architectures as features independently associated with ALK+ lung adenocarcinomas. A phenotypic scoring system based on these characteristics predicted the ALK-rearrangement genotype with a sensitivity of 88%. Notably, although the validation set was not perfectly matched to the initial cohort on which the multivariate analysis was performed, the multivariate analysis-based scoring system predicted ALK+ tumors with a comparable sensitivity, albeit lower specificity.
The presence of tumor cells with signet ring morphology was the most significant independent feature of ALK rearrangement in primary lung adenocarcinomas as well as metastatic tumors and small biopsies obtained by minimally invasive procedures. In fact, the presence of signet ring cells showed a higher specificity for the ALK+ genotype compared with the multivariate model-based scoring system. Furthermore, the proportion of tumor involvement by signet ring cells directly correlated with specificity for ALK rearrangements in both the initial cohort of 319 patients (data not shown) and the validation cases. These findings underscore the recent recommendations in the IASLC/ATS/ERS lung adenocarcinoma classification system to record the presence and extent of signet ring cells in lung adenocarcinomas.18 Although signet ring cells can be seen in many architectural patterns of lung adenocarcinoma and do not appear to define a subtype of lung adenocarcinoma per se, documenting the approximate percentage of signet ring cells may allow pathologists to identify cases that have a higher probability of harboring ALK rearrangements. Nevertheless, the assessment of signet ring cells alone has a relatively low sensitivity for predicting ALK rearrangements and is insufficient as a sole screening parameter for ALK rearrangements.
A hepatoid cytomorphology was also identified as a feature independently associated with ALK+ primary lung adenocarcinomas in our cohort. Solis et al21 recently reported 16 cases of primary oncocytic lung adenocarcinomas in which over 50% of the tumor was composed of cells with abundant eosinophilic cytoplasm, round nuclei, and conspicuous nucleoli, similar to the cells we describe as having a hepatoid cytology. Mutation analysis of these oncocytic adenocarcinomas revealed that approximately 40% of these tumors harbored activating mutations in either EGFR or KRAS. It would be interesting to determine the proportion of tumors harboring ALK rearrangements among the remaining cases that lack EGFR and KRAS mutations. Of note, 60% (9/15) of ALK+ primary lung tumors and 92% (12/13) of ALK+ metastatic lung tumors with hepatoid cytomorphology showed a solid-predominant pattern in our cohort. The presence of solid nests or sheets of tumor cells with hepatoid cytomorphology may be misinterpreted as squamous cell carcinoma and may account for at least some previous reports of rare ALK-rearranged tumors with a ‘squamous’ histology.11, 16
Various histologic patterns have been associated with ALK+ lung adenocarcinomas. The majority of ALK+ lung adenocarcinomas in our study showed a solid-predominant architectural pattern, in agreement with previous reports from both Western and Asian patient cohorts.11, 15 We also found that micropapillary-predominant adenocarcinomas were significantly associated with ALK rearrangements. The presence of a micropapillary pattern in lung adenocarcinomas reportedly correlates with increased propensity for metastasis, pleural invasion, and decreased survival among stage I patients.22, 23, 24 Molecular analysis of the 41 lung adenocarcinomas with a micropapillary-predominant pattern in our study cohort revealed ALK rearrangements in 19 (46%) followed by KRAS mutations in 6 (15%) (data not shown), whereas others have demonstrated a strong association between EGFR mutations and the micropapillary pattern in previous studies with resection specimens.25, 26 These findings complement the evolving molecular characterization of micropapillary lung adenocarcinomas and support the recent recommendations by the IASLC/ATS/ERS to consider micropapillary architecture to be a distinct and potentially biologically significant histologic subtype.18
Interestingly, the papillary-predominant pattern emerged as a histologic subtype that was independently associated with ALK+ lung adenocarcinomas after controlling for other morphologic features with the multivariate model. The association between the papillary subtype and ALK rearrangements was not evident in the univariate analysis, likely because dominant histology is not independent of other morphologic parameters, such as the presence of signet ring cells or hepatoid cells. In other words, the cytologic features of ALK+ tumors are frequently associated with certain histologic patterns, as evidenced by prior studies describing combinations of morphologic elements that are characteristic of ALK rearrangements, such as the ‘solid signet ring cell’ pattern.11, 15 Our analysis has also shown that signet ring cells and hepatoid cytology are both significantly associated with solid-predominant histology. Therefore, although the overall prevalence of papillary-predominant tumors is low among ALK+ lung cancers, this histologic subtype may indicate the presence of ALK rearrangements, especially in cases where clinical features are suggestive of ALK rearrangements but other characteristic cytologic features such as signet ring and hepatoid tumor cells are absent.
Our analysis also found that acinar-predominant histology was significantly decreased among ALK+ lung adenocarcinomas, whereas numerous studies from a primarily Japanese patient population have found acinar-predominant tumors to be significantly increased in ALK+ lung adenocarcinomas.8, 13, 15, 17 Furthermore, our analysis did not identify the cribriform pattern, extracellular mucin, or the ‘mucinous cribriform’ pattern to be strong predictors for ALK rearrangements in our patient cohort, in contrast to the findings described by others.15, 17 It is unclear whether the discrepancies between our study and those from Japan represent ethnic or other differences between the study populations. In spite of these differences, the solid, micropapillary, and cribriform patterns were all classified as ‘high-grade’ patterns with increased metastatic potential by a recently proposed histologic grading system for lung adenocarcinomas.27 Therefore, regardless of the apparent morphologic differences among the various studies, there seems to be agreement that ALK+ tumors tend to adopt an aggressive histologic pattern.
In contrast to primary ALK+ lung adenocarcinomas, ALK+ tumors from metastatic foci could not be distinguished from ALK− tumors based on the predominant histologic subtype. As solid and micropapillary patterns of lung adenocarcinoma have been reported to have an increased propensity for metastasis, it is possible that any statistical predilection that ALK+ tumors show for a solid or micropapillary pattern is diminished by the overall higher prevalence of solid and micropapillary patterns at metastatic sites.22, 23, 27 Although ALK+ primary lung adenocarcinomas were associated with the presence of hepatoid tumor cells and psammoma bodies, these associations also failed to be preserved in metastatic tumors. It is currently unclear why these morphologic features help distinguish ALK rearrangements in primary lung tumors but not in metastatic tumors.
We included the specimen type as a covariate in the statistical analysis of both primary and metastatic lung adenocarcinomas, given the notion that the amount and quality of tissue obtained by a particular type of procedure may influence the cytomorphologic evaluation of the specimen. Interestingly, specimen type turned out to be a significant and independent predictor of ALK rearrangements in our study cohort and was thus included in the scoring system. In our study cohort, 48% of ALK+ tumors were sampled by small biopsies, compared with 25% of ALK− tumors (P<0.0001, data not shown). This association between ALK status and specimen type likely reflects the fact that the majority of ALK+ lung adenocarcinomas present at an advanced clinical stage and are typically diagnosed on specimens obtained from metastatic or primary sites by minimally invasive procedures.11, 12 Notably, small biopsy specimens were sufficient to show a significant association between signet ring cells and ALK+ tumors, although signet ring cells were present only focally (ie, comprised <10% of the examined tumor) in 18 out of 50 (36%) ALK+ small biopsy specimens. In contrast, small biopsy specimens showed no significant association between ALK status and other morphologic features, including predominant histologic patterns. Of note, a small biopsy may not accurately represent the predominant histologic subtype of the entire lesion, and the lack of association between histologic pattern and ALK status may reflect a limitation of the sampling technique. Furthermore, small specimens are susceptible to procedure-related artifacts, and poor preservation of tumor architecture in such samples may have resulted in more frequent classification of tumor histology into the ‘solid’ category.
Although our study highlights the utility of comprehensive morphologic analysis of lung adenocarcinomas, it also underscores the limitations of phenotypic analysis in screening for the genotype of a tumor. Morphologic analysis alone will not detect a minority of ALK+ lung adenocarcinomas and is not sufficient as a sole screening method for ALK rearrangements. With the recent FDA approval of crizotinib, it has become increasingly important to identify all patients who may be eligible for treatment with ALK inhibitors. Considering that compulsory FISH analysis for ALK rearrangement on all lung adenocarcinoma specimens may not be feasible because of financial and/or personnel constraints, correlation with clinical profiles,11, 12 and/or the establishment of immunohistochemical scoring system28, 29, 30, 31 are warranted in order to efficiently triage lung adenocarcinomas for ALK rearrangement studies. To that end, our laboratory is currently validating an anti-ALK monoclonal antibody (clone 5A4, Novocastra, Newcastle Upon Tyne, UK) at 1:50 dilution with Leica automation (Leica BOND-III, Leica Microsystems, Buffalo Groove, IL, USA) for use as an immunohistochemical screening tool for ALK rearrangements. Preliminary analysis in a subset of our FISH-proven ALK+ (N=29) and ALK− (N=110) lung adenocarcinomas show that a two-tier scoring system (any positive vs negative staining) detects ALK rearrangements with a sensitivity, specificity, PPV, and NPV of 100% (data not shown). Although the results need to be validated in larger cohort studies, given the superior sensitivity and specificity of ALK immunohistochemistry compared with morphologic analysis alone, these findings support the use of screening immunohistochemistry with the 5A4 antibody for all lung adenocarcinomas, with confirmation of ALK rearrangements by FISH in positively staining cases.
References
Boyle P, Levin B, (eds) World Cancer Report 2008. WHO Press: Lyon, France, 2008, pp 390–394.
Weinstein IB, Joe A . Oncogene addiction. Cancer Res 2008;68:3077–3080; discussion 80.
Rikova K, Guo A, Zeng Q, et al. Global survey of phosphotyrosine signaling identifies oncogenic kinases in lung cancer. Cell 2007;131:1190–1203.
Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007;448:561–566.
Chiarle R, Voena C, Ambrogio C, et al. The anaplastic lymphoma kinase in the pathogenesis of cancer. Nat Rev Cancer 2008;8:11–23.
Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010;363:1693–1703.
Camidge DR, Kono SA, Flacco A, et al. Optimizing the detection of lung cancer patients harboring anaplastic lymphoma kinase (ALK) gene rearrangements potentially suitable for ALK inhibitor treatment. Clin Cancer Res 2010;16:5581–5590.
Inamura K, Takeuchi K, Togashi Y, et al. EML4-ALK lung cancers are characterized by rare other mutations, a TTF-1 cell lineage, an acinar histology, and young onset. Mod Pathol 2009;22:508–515.
Inamura K, Takeuchi K, Togashi Y, et al. EML4-ALK fusion is linked to histological characteristics in a subset of lung cancers. J Thorac Oncol 2008;3:13–17.
Koivunen JP, Mermel C, Zejnullahu K, et al. EML4-ALK fusion gene and efficacy of an ALK kinase inhibitor in lung cancer. Clin Cancer Res 2008;14:4275–4283.
Rodig SJ, Mino-Kenudson M, Dacic S, et al. Unique clinicopathologic features characterize ALK-rearranged lung adenocarcinoma in the western population. Clin Cancer Res 2009;15:5216–5223.
Shaw AT, Yeap BY, Mino-Kenudson M, et al. Clinical features and outcome of patients with non-small-cell lung cancer who harbor EML4-ALK. J Clin Oncol 2009;27:4247–4253.
Takahashi T, Sonobe M, Kobayashi M, et al. Clinicopathologic features of non-small-cell lung cancer with EML4-ALK fusion gene. Ann Surg Oncol 2010;17:889–897.
Wong DW, Leung EL, So KK, et al. The EML4-ALK fusion gene is involved in various histologic types of lung cancers from nonsmokers with wild-type EGFR and KRAS. Cancer 2009;115:1723–1733.
Yoshida A, Tsuta K, Nakamura H, et al. Comprehensive histologic analysis of ALK-rearranged lung carcinomas. Am J Surg Pathol 2011;35:1226–1234.
Yoshida A, Tsuta K, Watanabe S, et al. Frequent ALK rearrangement and TTF-1/p63 co-expression in lung adenocarcinoma with signet-ring cell component. Lung Cancer 2010;72:309–315.
Jokoji R, Yamasaki T, Minami S, et al. Combination of morphological feature analysis and immunohistochemistry is useful for screening of EML4-ALK-positive lung adenocarcinoma. J Clin Pathol 2010;63:1066–1070.
Travis WD, Brambilla E, Noguchi M, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society international multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 2011;6:244–285.
Dias-Santagata D, Akhavanfard S, David SS, et al. Rapid targeted mutational analysis of human tumours: a clinical platform to guide personalized cancer medicine. EMBO Mol Med 2010;2:146–158.
Barletta JA, Yeap BY, Chirieac LR . Prognostic significance of grading in lung adenocarcinoma. Cancer 2010;116:659–669.
Solis LM, Raso MG, Kalhor N, et al. Primary oncocytic adenocarcinomas of the lung: a clinicopathologic, immunohistochemical, and molecular biologic analysis of 16 cases. Am J Clin Pathol 2010;133:133–140.
Amin MB, Tamboli P, Merchant SH, et al. Micropapillary component in lung adenocarcinoma: a distinctive histologic feature with possible prognostic significance. Am J Surg Pathol 2002;26:358–364.
Kamiya K, Hayashi Y, Douguchi J, et al. Histopathological features and prognostic significance of the micropapillary pattern in lung adenocarcinoma. Mod Pathol 2008;21:992–1001.
Miyoshi T, Satoh Y, Okumura S, et al. Early-stage lung adenocarcinomas with a micropapillary pattern, a distinct pathologic marker for a significantly poor prognosis. Am J Surg Pathol 2003;27:101–109.
Motoi N, Szoke J, Riely GJ, et al. Lung adenocarcinoma: modification of the 2004 WHO mixed subtype to include the major histologic subtype suggests correlations between papillary and micropapillary adenocarcinoma subtypes, EGFR mutations and gene expression analysis. Am J Surg Pathol 2008;32:810–827.
Ninomiya H, Hiramatsu M, Inamura K, et al. Correlation between morphology and EGFR mutations in lung adenocarcinomas. Significance of the micropapillary pattern and the hobnail cell type. Lung Cancer 2009;63:235–240.
Sica G, Yoshizawa A, Sima CS, et al. A grading system of lung adenocarcinomas based on histologic pattern is predictive of disease recurrence in stage I tumors. Am J Surg Pathol 2010;34:1155–1162.
Mino-Kenudson M, Chirieac LR, Law K, et al. A novel, highly sensitive antibody allows for the routine detection of ALK-rearranged lung adenocarcinomas by standard immunohistochemistry. Clin Cancer Res 2010;16:1561–1571.
Paik JH, Choe G, Kim H, et al. Screening of anaplastic lymphoma kinase rearrangement by immunohistochemistry in non-small cell lung cancer: correlation with fluorescence in situ hybridization. J Thorac Oncol 2011;6:466–472.
Yi ES, Boland JM, Maleszewski JJ, et al. Correlation of IHC and FISH for ALK gene rearrangement in non-small cell lung carcinoma: IHC score algorithm for FISH. J Thorac Oncol 2011;6:459–465.
McLeer-Florin A, Moro-Sibilot D, Melis A, et al. Dual IHC and FISH testing for ALK gene rearrangement in lung adenocarcinomas in a routine practice: a French study. J Thorac Oncol 2012;7:348–354.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
AJI is a paid consultant for Pfizer and Abbott Molecular. DDS and AJI filed a patent application for the SNaPshot methods used in this study. DDS and AJI are consultants for Bio-Reference Laboratories. The remaining authors declare no conflict of interest.
Additional information
This study was presented in part at 100th annual meeting of the United States and Canadian Academy of Pathology in San Antonio, TX, USA, and at 2011 Biennial Meeting of the Pulmonary Pathology Society in New York, NY, USA.
Supplementary Information accompanies the paper on Modern Pathology website
Rights and permissions
About this article
Cite this article
Nishino, M., Klepeis, V., Yeap, B. et al. Histologic and cytomorphologic features of ALK-rearranged lung adenocarcinomas. Mod Pathol 25, 1462–1472 (2012). https://doi.org/10.1038/modpathol.2012.109
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.109
Keywords
This article is cited by
-
Rare molecular subtypes of lung cancer
Nature Reviews Clinical Oncology (2023)
-
Clinicopathological features and prognostic significance of pulmonary adenocarcinoma with signet ring cell components: meta-analysis and SEER analysis
Clinical and Experimental Medicine (2023)
-
Individualized nomogram for predicting ALK rearrangement status in lung adenocarcinoma patients
European Radiology (2021)
-
Clinicopathological Significance of Micropapillary Pattern in Lung Adenocarcinoma
Pathology & Oncology Research (2018)
-
ALK rearrangement in specific subtypes of lung adenocarcinoma: immunophenotypic and morphological features
Medical Oncology (2017)