Abstract
Bcl-2 is an antiapoptotic protein that promotes cell survival, but also may block proliferation. In breast cancer, bcl-2 expression correlates with favorable prognosis and estrogen receptor (ER) positivity. However, experimental data have paradoxically suggested that bcl-2 promotes chemoresistance and metastasis. A direct and comprehensive comparison of bcl-2 expression between primary breast carcinomas and paired distant metastases has not been performed. We completed rapid autopsies on 17 patients with archived primary tumors and metastatic breast carcinoma, and created single-patient tissue microarrays containing each patient's primary tumor and matched metastases. Expression of bcl-2, ER, progesterone receptor, and HER-2 in primary tumors and matched metastases were compared by immunohistochemistry. All 11 ER-positive cases showed bcl-2 labeling in the primary tumor, whereas only 3 of 6 ER-negative cases did (P=0.029). In 10 cases, bcl-2 labeling in metastases was similar to that of the primary, although 3 cases showed significant variation among metastases. In six other cases, bcl-2 labeling was lost or significantly diminished in metastases. Five of the latter cases were Luminal A (ER-positive, HER-2-negative) primaries, three of which lost hormone receptors in metastases. Only 1 of 17 cases showed an increase in bcl-2 labeling in metastases compared with the paired primary tumor. In conclusion, bcl-2 is infrequently upregulated in metastatic breast carcinoma. Instead, downregulation of bcl-2 expression may occur in the setting of hormone therapy resistance. Our findings call into question the potential utility of anti-bcl-2 therapy in metastatic breast cancer.
Similar content being viewed by others
Main
Apoptosis, which has a central role in the development of normal tissues as well as cancers, is regulated by a large family of both proapoptotic and antiapoptotic proteins.1 Bcl-2 is one such protein which is able to block most proapoptotic stimuli,2 and therefore promote cell survival. Bcl-2 family proteins regulate the intrinsic mitochondrial apoptosis pathway that responds to numerous stress stimuli, such as DNA damage or deprivation of growth factors.3 When activated, this pathway leads to permeabilization of the mitochondrial outer membrane and release of proapoptotic factors such as cytochrome c that activate the caspase cascade.3 Prosurvival family members, such as bcl-2, maintain the integrity of mitochondria by preventing proapoptotic proteins such as bax or bak from initiating this pathway.3
Although bcl-2 protein prevents apoptosis, it also inhibits proliferation;4, 5, 6 these two processes involve independent pathways that are regulated differently.7, 8 Indeed, the antiproliferation and antiapoptosis actions of bcl-2 can be dissociated.9 Expression of bcl-2 has been shown to arrest cells in the G0 or G1 stage of the cell cycle, when deprived of growth factors.10 Other studies have similarly shown that bcl-2 can delay progression to S phase,11 and inhibit growth of some solid tumors.12 Hence, bcl-2 has two activities, one (anti-apoptotic) that promotes tumorigenesis, and another (antiproliferative), which is antitumorigenic.
In normal breast tissue, bcl-2 is detected in normal epithelial and myoepithelial cells.7 Its expression is transcriptionally regulated by estrogen receptor (ER).13 In breast cancer, bcl-2 expression also correlates with ER positivity.14 Numerous studies have shown that women with bcl-2-positive tumors have better overall survival compared with those with bcl-2-negative tumors,15, 16, 17 which makes sense, given that bcl-2-positive tumors tend to be of lower grade. Moreover, bcl-2 expression has correlated with favorable prognosis even in multivariate regression analyses.16, 18, 19 This data suggests that bcl-2 expression correlates with indolent biology in breast cancer and thus might have antimetastatic properties.
Contrary to the above favorable prognostic data is laboratory-based data that suggests that bcl-2 expression correlates with aggressive, prometastatic behavior in breast cancer. In vitro data have shown that bcl-2 expression promotes resistance of tumor cell lines to chemotherapy.20, 21, 22 Other studies found that bcl-2 mRNA is upregulated in lymph node metastases relative to matched primary breast carcinomas.23 Finally, in a mouse model, expression of bcl-2 in mammary epithelial cells did not increase proliferation or invasion in vitro, but specifically did enhance spontaneous lung metastases from orthotopically implanted primary tumors.24 Hence, the favorable prognostic data regarding bcl-2 is difficult to reconcile with these prometastatic activities, and the role of bcl-2 in breast cancer metastases in humans is not clear. Given the utilization of targeted therapy against bcl-2 in recent clinical trials,25 in vivo investigations of the function of bcl-2 have particular relevance.
A comprehensive comparison of bcl-2 expression between primary breast carcinomas and paired distant metastases has not been performed. In this study, we examined bcl-2 expression by immunohistochemistry to directly compare metastases with matched primary tumors using our unique rapid autopsy cohort.
Materials and methods
Autopsies
We performed rapid autopsies on 17 patients with widely metastatic breast cancer, who consented to have autopsies performed within a short post-mortem interval (generally 1–4 h), so that fresh tissue could be harvested for research. The interval is similar to a typical time span between removal of tissues during surgery and processing in surgical pathology. This protocol was approved by the Institutional Review Boards of The Johns Hopkins Hospital and the Department of Defense. Initial biomarker analysis of the first 10 cases of this cohort (not including bcl-2 expression) recently has been published.26
Tissue Microarrays
Single-patient tissue microarrays were constructed as previously described.26 Each microarray contained 99 tissue cores, each 1.4 mm in diameter. These were arranged as 9 rows, each with 11 columns. Column 6 consisted of various unrelated control tissues, leaving 90 cores on the array for samples from each patient's archived primary breast carcinoma and multiple different metastases harvested at autopsy. Four to five cores of each tumor were placed on the array to control for lesional heterogeneity. Tissue from normal organs was also included for each case.
Case Categorization
All microarrays were evaluated for expression of ER, progesterone receptor (PR), and HER-2. Immunohistochemistry labeling for ER and PR were performed on the Benchmark XT autostainer (Ventana Medical Systems Inc., Tucson, AZ, USA) using I-View detection kit. The antibodies, dilutions, and sources were as follows: ER, monoclonal antibody; 1:1 dilution, Ventana Medical Systems Inc., catalog no. 76O-2596; PR, monoclonal antibody, 1:60 dilution, DAKO, catalog no. M3569. Infiltrating ductal carcinomas demonstrating weak, moderate, or strong nuclear labeling for ER or PR in greater than 1% of cells were considered ER-positive or PR-positive, respectively. HER-2 immunohistochemistry was performed using the DAKO Herceptest kit according to the manufacturer's standard protocol. The carcinomas were scored using established criteria as 0 or 1+ (negative), 2+ (equivocal), and 3+ (positive). Fluorescence in situ hybridization analysis for HER-2 amplification was also performed on the cases with positive or equivocal immunohistochemical HER-2 results using the Path Vysion kit (Des-Plaines, IL, USA). Cytokeratin 5/6 (CK 5/6) immunohistochemistry was performed on primary tumors that were negative for ER, PR, and HER-2 to identify Basal-like carcinoma cases, using the Benchmark XT autostainer (prediluted monoclonal antibody, DAKO, catalog no. M7237) as previously described.27
The cases were categorized by the immunohistochemical surrogate profile of their primary tumor (ER, PR, HER-2, CK 5/6) into one of four groups (Luminal A, Luminal B, HER-2, or Basal-like), which correlate with groups defined by gene expression profiling. The immunohistochemical surrogate profiles are as follows:
Luminal A tumors: ER-positive, HER-2-negative
Luminal B tumors: ER-positive, HER-2-positive
HER-2 tumors: ER-negative, PR-negative, HER-2-positive
Basal-like tumors: ER-negative, PR-negative, HER-2-negative, CK5/6-positive.
Labeling for ER and PR were also evaluated in metastases to determine loss or gain of expression. Cases with a Luminal A phenotype that lost expression of either ER and/or PR in metastases were categorized as Luminal A, loss cases.
Bcl-2 Labeling and Interpretation
Immunohistochemical labeling for bcl-2 was performed on the Benchmark XT autostainer (Ventana Medical Systems Inc.) using the I-View detection kit. Using the monoclonal antibody from Ventana (prediluted, catalog no. 760–2693), bcl-2 labeling was scored for each separate lesion on a scale of 0 to 300, calculated by percentage labeling (0–100%) multiplied by intensity (0=none, 1=weak, 2=moderate, 3=strong). Expression was scored by two authors (APS and PA) in 17 primary breast carcinomas (comprising 161 microarray spots) and matched metastases (comprising 897 microarray spots from 193 different metastatic sites). On the basis of these data, the labeling patterns of bcl-2 in the paired metastases were evaluated as overall similar to the primary, increased, or decreased. Labeling was considered similar if the difference between the primary and the overall average of all metastases was within an absolute score of ±30. If different metastases’ bcl-2 labeling scores were both higher and lower than that of the primary, the metastases were considered to be similar overall to the primary, but heterogeneous. Reactive lymphocytes in each section served as an internal control for staining; tissue microarray spots that did not demonstrate adequate control staining were excluded from analysis.
Results
Demographics
The clinicopathological details of the 17 cases are summarized in Table 1. The average post-mortem interval before autopsy was 3.4 h, with all cases within the range of 1 and 4 h except for Case 9. Of the 17 primary tumors, there were 16 infiltrating ductal carcinomas and 1 infiltrating lobular carcinoma. Nine cases were Elston Grade 2 and eight were Elston Grade 3. The average age at diagnosis was 45.8 years, and the average age at time of death was 52.3 years. The clinical course varied with survival times ranging from 1 year for three of the cases (an intermediate grade infiltrating ductal carcinoma diagnosed at advanced stage (Case 4), a high grade infiltrating ductal carcinoma of Luminal B subtype (Case 11), and a Basal-like case (Case 16)) to 17 years for an intermediate grade infiltrating ductal carcinoma (Case 5), with an average survival interval of 6.5 years. Four of the cases had negative axillary nodes at diagnosis, 12 had axillary metastases, and 1 did not have axillary node sampling. An average of 12 metastatic sites were identified at autopsy per case, with a range of 3–18.
Primary Tumors
There were 10 ER+, HER-2– (Luminal A) cases; 1 ER+, focally HER– 2+ (Luminal B) case; 5 ER–, PR–, HER-2–, CK5/6+ (Basal-like) cases; and 1 ER–, PR–, and HER-2+ (HER-2) case. The results of bcl-2 expression in the primary tumor for each case are summarized in Table 2. All 11 ER+ cases (10 Luminal A, 1 Luminal B) showed bcl-2 expression in the primary tumor, whereas only 3 of the 6 ER– cases (5 Basal-like, 1 HER-2) did, the latter 3 cases in patchy and/or weak manner. This difference was statistically significant (P=0.029), and consistent with the previously referenced published literature, in which bcl-2 expression correlates with ER expression.
Metastases
Five Luminal A cases lost expression of ER and/or PR in their metastases, and thus were classified as Luminal A, loss cases. Two of these (Cases 1 and 5) showed loss of bcl-2 expression in their distant metastases (1 of these cases (Case 1) is shown in Figure 1). Case 3 demonstrated downregulation of bcl-2 in some metastases, and Case 4 maintained similar expression of bcl-2 in the metastases. Case 2 demonstrated heterogeneous bcl-2 expression in metastases, on average considered to be similar to that of the primary tumor.
A Luminal A, loss case showing bcl-2 loss in metastases (Case 1). This primary infiltrating lobular carcinoma (a) gave rise to numerous metastases, including one in the gallbladder (b). The primary tumor expressed ER (c), but the metastases did not (d). Similarly, PR was positive in the primary (e) but lost in the metastases (f). Bcl-2 expression was strong in the primary (g) but was lost in the metastases (h). Note the intact bcl-2 expression in this cluster of native lymphocytes in the gallbladder metastasis (h inset), serving as an internal control for staining.
Five Luminal A cases retained ER expression in their metastases; Cases 8 and 9 showed bcl-2 downregulation in a subset of metastases, Case 10 showed similar bcl-2 expression in its metastases. Cases 6 and 7 demonstrated heterogeneous bcl-2 expression in metastases, with some metastases labeling more and some less than the primary, but on average the metastases were considered similar to the primary tumor. Interestingly, in Case 6, bcl-2 expression was increased in a subset of metastases showing increased PR expression (Figure 2). As previously shown,26 this case was an infiltrating ductal carcinoma primary that gave rise to E-cadherin-positive ductal metastases and E-cadherin-negative lobular metastases. The ductal metastases showed increased PR and bcl-2 expression.
A case showing focal upregulation of bcl-2 in a subset of metastases paralleling increased PR expression (Case 6). This primary infiltrating ductal carcinoma (a) had metastases with both ductal (b, pericardium) and lobular (c, liver) morphology. ER was positive in both the primary and the metastases (not shown). PR was weakly positive in the primary (d), and was upregulated in this pericardial metastasis (e), while remaining similar to the primary in other metastases, such as the ones in the liver (f). Bcl-2 was positive in the primary (g), and was upregulated in the pericardial metastasis (h), paralleling the increased PR. By contrast, the liver metastasis showed similar bcl-2 expression to the primary (i). The strong bcl-2 expression in lymphocytes scattered among the tumor cells in the metastasis serves as an internal control for staining (i).
The Luminal B case retained similar, weak ER labeling and bcl-2 expression in its metastases, as was seen in the primary tumor.
Of the six ER– cases, one Basal-like case showed focal upregulation in a minority of metastases (Case 12). One Basal-like case showed downregulation from weak positivity in the primary to loss in the metastases (Case 13), and two Basal-like cases remained bcl-2 negative in their metastases (Cases 14 and 16). Two cases (one Basal-like, one HER-2) showed patchy expression similar to the primary tumor (Cases 15 and 17).
The detailed scoring of bcl-2 expression is presented in Supplementary Table 1, as an overall average of all spots from each tissue location.
In summary, only 1 of 17 cases (a Basal-like carcinoma, Case 12) showed an overall increase in bcl-2 expression in metastases compared with the paired primary tumor. One Luminal A case showed an increase in bcl-2 expression in parallel with an upregulation of PR in certain metastases (Case 6). In six other cases, bcl-2 expression showed loss (Cases 1, 5, and 13) or significant downregulation (Cases 3, 8, and 9) in metastatic lesions. Five of these cases were Luminal A primaries, three of which lost hormone receptors in metastases.
Discussion
Although bcl-2 protein prevents apoptosis, it also can prevent proliferation;4, 5, 6 these two processes involve independent pathways with distinct regulation.7, 8 Indeed, studies have shown that the antiproliferation and antiapoptosis actions of bcl-2 can be dissociated.9
The dual actions of bcl-2, both promoting cell cycle arrest but also preventing apoptosis, suggest that cells may choose to preserve survival at the expense of growth.4 The functions of the protein are also likely to be dictated by the underlying tissue type. Lymphocytes, which receive frequent signals for apoptosis during maturation, may ultimately use bcl-2 as an oncogene, suppressing their own underlying antiproliferative functions; epithelia, on the other hand, may recruit the opposite mechanism to rein in a proliferative phase during hormonally driven cycling.4 These paradoxical actions imply that bcl-2 is delicately situated at the crossroads of several complex physiological pathways, and potential pharmacological interventions to block or modulate its effects may have unforeseen consequences.
Previous studies examining the role of bcl-2 in breast cancer progression have mainly evaluated bcl-2 expression patterns in the primary tumor over a course of therapy/time. Relatively few studies have compared bcl-2 expression between the primary tumor and metastases, and these studies have examined loco-regional axillary lymph node metastases. An increase in bcl-2 mRNA expression has been detected in local axillary metastases as compared with the primary breast tumor;23 and other authors have shown an increase in a small subset of axillary metastases.28 However, it should be noted that the majority of the paired samples in the latter were in fact concordant (ie, if the primary tumor showed high bcl-2 expression, the node metastases showed a similar pattern, and vice versa). A separate study also reported similar bcl-2 expression (but not increased) between the primary tumor and node metastases.29 Similarly, concordance has been shown between primary tumors and their corresponding synchronous axillary lymph node metastasis;30 but only 10 of 76 primary tumors (13%) were positive for bcl-2 expression in the D’Andrea et al30 study, and the authors only evaluated the cases categorically (positive/negative) with no reference to an increase or decrease in expression.
Our study patients underwent many cycles of adjuvant therapy over time, developing resistance to therapy and distant metastases over a course of months or years before eventually succumbing to disease. It is likely that the tumor biology of the distant metastases of our patients is more complex, and far more evolved, than that of the untreated local axillary lymph node metastases present at diagnosis that earlier studies have examined. Most importantly, all of these tumors became resistant to hormonal therapy, some associated with loss of ER or PR. The majority of our cases did not show an increase in bcl-2 labeling in metastases, indicating that bcl-2 may not be a promoter of distant metastases as previous laboratory-based data has suggested.
Instead, we found downregulation of bcl-2 expression in metastases in a subset of Luminal A primaries. In three cases, loss of bcl-2 correlated with loss of hormone receptor expression, suggesting a direct cause and effect relationship. Further evidence for linkage to hormone receptor expression comes from Case 6, in which focally increased bcl-2 expression correlated directly with increased PR labeling. We suspect that in these cases, loss of bcl-2 expression reflects alterations in ER signaling, which correlates with resistance to hormone therapy. Perhaps removal of the antiproliferative effect of bcl-2 in some Luminal A cancers (ie, loss of growth inhibition caused by bcl-2 downregulation) promotes metastases more than the loss of the antiapoptotic activity. Regardless, these results suggest potential limitations to utilization of targeted anti-bcl-2 therapy in breast cancer.
References
Basu A, Rowan BG . Genes related to estrogen action in reproduction and breast cancer. Front Biosci 2005;10:2346–2372.
Agarwal ML, Taylor WR, Chernov MV, et al. The p53 network. J Biol Chem 1998;273:1–4.
Frenzel A, Grespi F, Chmelewskij W, et al. Bcl2 family proteins in carcinogenesis and the treatment of cancer. Apoptosis 2009;14:584–596.
Zinkel S, Gross A, Yang E . BCL2 family in DNA damage and cell cycle control. Cell Death Differ 2006;13:1351–1359.
Borner C . Diminished cell proliferation associated with the death-protective activity of Bcl-2. J Biol Chem 1996;271:12695–12698.
Reed JC, Miyashita T, Takayama S, et al. BCL-2 family proteins: regulators of cell death involved in the pathogenesis of cancer and resistance to therapy. J Cell Biochem 1996;60:23–32.
Park S, Kim H, Song B . Down regulation of bcl2 expression in invasive ductal carcinomas is both estrogen- and progesterone-receptor dependent and associated with poor prognostic factors. Pathol Oncol Res 2002;8:26–30.
Strasser A, Huang DC, Vaux DL . The role of the bcl-2/ced-9 gene family in cancer and general implications of defects in cell death control for tumourigenesis and resistance to chemotherapy. Biochim Biophys Acta 1997;1333:F151–F178.
Reed JC . Balancing cell life and death: bax, apoptosis, and breast cancer. J Clin Invest 1996;97:2403–2404.
Vaux DL, Cory S, Adams JM . Bcl-2 gene promotes haemopoietic cell survival and cooperates with c-myc to immortalize pre-B cells. Nature 1988;335:440–442.
Marvel J, Perkins GR, Lopez Rivas A, et al. Growth factor starvation of bcl-2 overexpressing murine bone marrow cells induced refractoriness to IL-3 stimulation of proliferation. Oncogene 1994;9:1117–1122.
Pietenpol JA, Papadopoulos N, Markowitz S, et al. Paradoxical inhibition of solid tumor cell growth by bcl2. Cancer Res 1994;54:3714–3717.
Johnston SR, MacLennan KA, Sacks NP, et al. Modulation of Bcl-2 and Ki-67 expression in oestrogen receptor-positive human breast cancer by tamoxifen. Eur J Cancer 1994;30A:1663–1669.
Leek RD, Kaklamanis L, Pezzella F, et al. bcl-2 in normal human breast and carcinoma, association with oestrogen receptor-positive, epidermal growth factor receptor-negative tumours and in situ cancer. Br J Cancer 1994;69:135–139.
Joensuu H, Pylkkanen L, Toikkanen S . Bcl-2 protein expression and long-term survival in breast cancer. Am J Pathol 1994;145:1191–1198.
Silvestrini R, Veneroni S, Daidone MG, et al. The Bcl-2 protein: a prognostic indicator strongly related to p53 protein in lymph node-negative breast cancer patients. J Natl Cancer Inst 1994;86:499–504.
Zhang GJ, Kimijima I, Abe R, et al. Apoptotic index correlates to bcl-2 and p53 protein expression, histological grade and prognosis in invasive breast cancers. Anticancer Res 1998;18:1989–1998.
Krajewski S, Blomqvist C, Franssila K, et al. Reduced expression of proapoptotic gene BAX is associated with poor response rates to combination chemotherapy and shorter survival in women with metastatic breast adenocarcinoma. Cancer Res 1995;55:4471–4478.
Elledge RM, Green S, Ciocca D, et al. HER-2 expression and response to tamoxifen in estrogen receptor-positive breast cancer: a Southwest Oncology Group Study. Clin Cancer Res 1998;4:7–12.
Kumar R, Vadlamudi RK, Adam L . Apoptosis in mammary gland and cancer. Endocr Relat Cancer 2000;7:257–269.
Knowlton K, Mancini M, Creason S, et al. Bcl-2 slows in vitro breast cancer growth despite its antiapoptotic effect. J Surg Res 1998;76:22–26.
Teixeira C, Reed JC, Pratt MA . Estrogen promotes chemotherapeutic drug resistance by a mechanism involving Bcl-2 proto-oncogene expression in human breast cancer cells. Cancer Res 1995;55:3902–3907.
Mimori K, Kataoka A, Yoshinaga K, et al. Identification of molecular markers for metastasis-related genes in primary breast cancer cells. Clin Exp Metastasis 2005;22:59–67.
Pinkas J, Martin SS, Leder P . Bcl-2-mediated cell survival promotes metastasis of EpH4 betaMEKDD mammary epithelial cells. Mol Cancer Res 2004;2:551–556.
Kang MH, Reynolds CP . Bcl-2 inhibitors: targeting mitochondrial apoptotic pathways in cancer therapy. Clin Cancer Res 2009;15:1126–1132.
Wu JM, Fackler MJ, Halushka MK, et al. Heterogeneity of breast cancer metastases: comparison of therapeutic target expression and promoter methylation between primary tumors and their multifocal metastases. Clin Cancer Res 2008;14:1938–1946.
Subhawong AP, Subhawong T, Nassar H, et al. Most basal-like breast carcinomas demonstrate the same Rb-/p16+ immunophenotype as the HPV-related poorly differentiated squamous cell carcinomas which they resemble morphologically. Am J Surg Pathol 2009;33:163–175.
Kristek J, Dm B, Kurbel S, et al. Tumor growth fraction, expression of estrogen and progesterone receptors, p53, bcl-2 and cathepsin D activity in primary ductal invasive breast carcinoma and their axillary lymph node metastases. Coll Antropol 2007;31:1043–1047.
Arun B, Kilic G, Yen C, et al. Correlation of Bcl-2 and p53 expression in primary breast tumors and corresponding metastatic lymph nodes. Cancer 2003;98:2554–2559.
D’Andrea MR, Limiti MR, Bari M, et al. Correlation between genetic and biological aspects in primary non-metastatic breast cancers and corresponding synchronous axillary lymph node metastasis. Breast Cancer Res Treat 2007;101:279–284.
Acknowledgements
This study was supported by NIH P50 CA88843.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Supplementary information
Rights and permissions
About this article
Cite this article
Subhawong, A., Nassar, H., Halushka, M. et al. Heterogeneity of Bcl-2 expression in metastatic breast carcinoma. Mod Pathol 23, 1089–1096 (2010). https://doi.org/10.1038/modpathol.2010.93
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.93
Keywords
This article is cited by
-
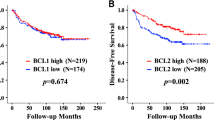
Prognostic significance of Bcl-2 expression in non-basal triple-negative breast cancer patients treated with anthracycline-based chemotherapy
Tumor Biology (2014)
-
MYC gene amplification is often acquired in lethal distant breast cancer metastases of unamplified primary tumors
Modern Pathology (2012)
-
A network-based, integrative study to identify core biological pathways that drive breast cancer clinical subtypes
British Journal of Cancer (2012)