Abstract
In gastrointestinal stromal tumors (GISTs), the occurrence of an epithelioid/mixed phenotype has been correlated to PDGFRA mutations, gastric localization and favorable outcome. On the other hand, the prognostic significance of an epithelioid/mixed growth pattern occasionally observed in GISTs with KIT mutation is unclear. The aim of this study was to evaluate the prognostic significance of an epithelioid/mixed phenotype in correlation to anatomical localization, genotype, and expression of cell-cycle markers in a series of 116 primary GISTs with KIT mutation on a tissue microarray. Independent of their anatomical localization, the majority of KIT-mutated GISTs displayed a pure spindled phenotype (72%), with the remaining tumors showing an epithelioid/mixed growth pattern. In KIT-mutated GISTs from the stomach, the occurrence of an epithelioid/mixed growth pattern was significantly correlated with larger tumor diameters (P=0.005), higher mitotic counts (P=0.0001), high-risk category (P=0.001), higher expression of the G2-phase cell-cycle marker cyclin B1 (P=0.04), higher expression of the G1 to M-phase proliferation marker Ki67 (P=0.02) and a significantly shorter disease-free survival (P=0.003) compared with tumors with pure spindled morphology. In contrast, there were no significant differences between pure spindled and epithelioid/mixed GISTs from the small/large bowel. Our findings indicate that the epithelioid/mixed phenotype in KIT-mutant gastric GISTs represents a secondary tumor growth pattern associated with tumor progression and adverse outcome, probably through accelerated G1/S-phase restriction point passage.
Similar content being viewed by others
Main
Gastrointestinal stromal tumors (GISTs) represent the most common mesenchymal gastrointestinal neoplasms. In general, GISTs display pure spindled (70%), pure epithelioid (20%) and mixed phenotypes.1 However, this distribution varies greatly with the anatomical site. In the largest series published by the Armed Forces Institute of Pathology (AFIP), the spindled, epithelioid and mixed phenotypes comprised 43, 27 and 30% of gastric, and 86, 5 and 9% of small bowel GISTs, respectively.2, 3
The majority of GISTs harbor oncogenic mutations in KIT (70–80%)4 and, less commonly, in the platelet-derived growth factor receptor alpha (PDGFRA) (8–10%).5 The remainder are wild type for both genes. The histological spindled subtype correlates with the presence of KIT mutations.6 On the other hand, the majority of PDGFRA-mutated GISTs display epithelioid or mixed (predominantly epithelioid) phenotypes.7, 8 Intriguingly, data on the correlation of the histological subtype with the clinical outcome have been inconsistent. The presence of an epithelioid/mixed morphology/component in GISTs was associated with malignant behavior in GISTs in several studies.6, 9, 10, 11, 12 On the other hand, PDGFRA-mutated epithelioid GISTs frequently exhibit a less aggressive behavior.7, 8, 13, 14, 15
Recently, we identified a morphological shift from spindled to epithelioid phenotype in GISTs that were composed of well-circumscribed spindled and epithelioid components.16 The epithelioid component displayed unfavorable histological features (higher cellularity, higher mitotic activity and higher Ki67 index), and was associated with more aggressive clinical course. In that study, secondary epithelioid components revealed a higher degree of chromosomal instability, associated with additional, secondary chromosomal copy number changes. In the current study, our aim was to analyze the prognostic significance of histomorphological phenotypes (pure spindled, pure epithelioid, mixed) in a series of 116 primary surgically resected, imatinib-naive GISTs with KIT mutation on a tissue microarray. PDGFRA mutants and wild-type GISTs were not included in this study. Furthermore, we analyzed the expression of cell-cycle proteins from different phases of the cell cycle.
Materials and methods
Tumor Samples
This study was performed on formalin-fixed and paraffin-embedded tissue samples from GISTs with KIT mutations. The cases have been retrieved from a consecutive series of 198 surgically resected primary GISTs originating from different sites along the GI tract. Of the 198 tumors, the mutation status was known in 156 cases; 116 (74%) had a KIT mutation, 26 (17%) had a PDGFRA mutation and 14 (9%) were wild type for both genes. All 116 primary GISTs with a KIT mutation irrespective of tumor site were used for this study. PDGFRA mutants, wild-type GISTs and tumors with unknown mutation status were excluded from further analysis. Mitoses were counted in 50 high power fields, corresponding to a total area of 11.9 mm2. Risk of clinically aggressive behavior was evaluated based on tumor size and mitotic activity according to the National Institute of Health (NIH) consensus criteria published in 2002,1 and the malignant potential was estimated according to the updated AFIP criteria published in 2006.6 The study has been approved by the review boards of our institutions.
Mutation Analysis of KIT
Mutation analysis of KIT exons 9, 11, 13 and 17, and of PDGFRA exons 12, 14 and 18 was performed using direct sequencing of PCR products as previously described.17
Evaluation of Histomorphological Growth Pattern and Immunohistochemistry
Tissue microarrays were constructed from paraffin-embedded tumor blocks using a semiautomated manual tissue arrayer (Alphametrix GmbH, Rodgau, Germany). For each of the tumor samples, four to six tissue punches (mean: 4.8) with a diameter of 0.1 cm from different tumor areas were analyzed. Histomorphological growth pattern was evaluated on H and E stainings of the tissue microarrays by AA without knowledge of the other clinicopathological variables. The growth pattern was classified as mixed (Figures 1a and d), pure epithelioid (Figures 1b and e) or pure spindled (Figures 1c and f). Tumors that showed a pure pattern on the tissue microarray cores (either epithelioid or spindled) were reevaluated using conventional slides to look for missed components. A comparison of the histomorphological classification on the tissue microarrays with the histomorphological classification on larger sections revealed a high agreement. Only four tumors (one from the stomach and three from the small bowel) displayed a pure epithelioid growth pattern on the tissue microarray cores. In each of these four cases, a careful evaluation of conventional slides revealed spindled areas, which were not represented on the tissue microarray cores (all the four tumors were large lesions measuring 4–12 cm). In contrast, none of the tumors with pure spindled growth pattern on the tissue microarray cores showed epithelioid growth pattern on the conventional slides. Immunohistochemistry was performed using standard procedures on the tissue microarrays. The following primary antibodies and conditions were used: anti-E2F1 (1:200 dilution, pH 6.1, clone KH95; Dianova, Hamburg, Germany), anti-Ki67-antigen (1:50 dilution, pH 6.1, clone Mib1; DakoCytomation, Hamburg, Germany), anti-cyclin D1 (1:100 dilution, pH 6.1, SP4; NeoMarkers, Medac GmbH, Wedel, Germany) and anti-cyclin B1 (1:100 dilution, pH 9.0, clone Y106; BioMol, Hamburg, Germany). Before incubation with the primary antibody, the slides underwent heat treatment for antigen retrieval (15 min at 95°C in 0.1 mol sodium citrate buffer pH 6.1 or pH 9.0). The DakoChemMate Kit was used for detection of the primary antibodies (DakoCytomation), with hemalaun as counter staining. From each tissue punch, a digital photo was taken, and a self-written computer program was used to count positively stained nuclei and also the counterstained nuclei.18 This approach enabled a quantitative analysis of the percentage of tumor cells with nuclear expression of the analyzed protein.
Statistics
Descriptive statistics, tests and graphs were performed with Statistica 6.0 (StatSoft, Hamburg, Germany). Associations between the clinicopathological and the molecular genetic parameters were evaluated using the Wilcoxon test, or the Fisher test in the case of categorical variables. Disease-free survival rates were plotted by the Kaplan–Meier method, and associations of patient and tumor parameters with disease-free survival times were assessed with the log-rank test.
Results
Clinicopathological Parameters
This study comprises a series of 116 surgically resected primary GISTs with KIT mutation. In all, 65 (56%) GISTs were from the stomach, 38 (33%) from the small bowel, 10 (8%) from the large bowel (8 rectum) and 3 (3%) from the mesentery/omentum. All tumors had been completely resected (R0). None had received imatinib therapy before surgery. Follow-up was available for 83 patients. Of these, 28 patients (34%) had tumor progress (tumor recurrence, liver metastasis or peritoneal metastasis) at a mean of 17 (±21, range 0–84) months, whereas the remainder 55 patients (66%) had no tumor progress after a mean follow-up of 46 (±37, range 0–156) months.
Comparison of Histomorphology with Clinicopathological Variables and Expression of Cell-Cycle Markers
None of the 116 GIST KIT mutants in this study showed a pure epithelioid phenotype. The epithelioid cytomorphology in tumors with epithelioid/mixed phenotypes frequently revealed a high nuclear–cytoplasmic ratio and a high degree of nuclear atypia. Most commonly, these tumors displayed a monotonous hypercellular round cell morphology with generally scanty cytoplasm and indistinct cell borders consistent with the hypercellular and sarcomatous epithelioid subtypes described by Miettinen et al2 for gastric GISTs.
Overall, the pure spindled phenotype occurred significantly more often compared with the epithelioid/mixed morphology (72 vs 28%, respectively). The distribution of spindled vs epithelioid/mixed phenotypes showed similar frequencies in tumors from different anatomical localizations (72 vs 28% for stomach, 74 vs 26% for small bowel, 70 vs 30% for large bowel and 67 vs 33% for mesentery/omentum; Table 1). Irrespective of the anatomical localization of the tumors, GISTs with an epithelioid/mixed morphology were significantly larger (P=0.008; Table 2), and had significantly higher mitotic counts (P=0.0002) compared with GISTs with a pure spindled morphology. Epithelioid/mixed GISTs were significantly more often of the high-risk categories according to Fletcher et al (P=0.001) and Miettinen and Lasota (P=0.001).1, 6 While there was no significant difference in the expression of G1-phase cyclin D1 or the G1/S-phase transcription factor E2F1, the epithelioid/mixed GISTs had a significantly higher expression of the G2-phase cyclin B1 (P=0.04), and also of the G1- to M-phase proliferation marker Ki67 (P=0.005).
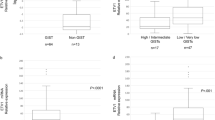
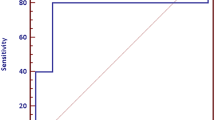
To evaluate whether there was a site-dependent difference, we analyzed KIT-mutated GISTs from the stomach and from the small and large bowel separately. The three tumors from omentum/mesentery were not further analyzed according to the small number of cases. In the group of gastric GISTs, tumors with epithelioid/mixed growth pattern remained significantly larger (P=0.005; Table 2; Figure 2a) and had higher mitotic counts (P=0.0001; Figure 2b) compared with tumors with pure spindled morphology. Epithelioid/mixed GISTs from the stomach were significantly more often of the high-risk categories according to Fletcher et al (P=0.001; Figure 3a) and Miettienen and Lasota (P=0.001).1, 6 Regarding the expression of cell-cycle proteins, there was no significant difference in the expression of the G1-phase cyclin D1 (P=0.07; Figure 2c) or the G1/S-phase transcription factor E2F1 (P=0.6; Figure 2d). On the other hand, there was a significantly higher expression of the G2-phase cyclin B1 (P=0.04; Figure 2e) and of the G1- to M-phase proliferation marker Ki67 (P=0.02; Figure 2f) in gastric GISTs with KIT mutation and epithelioid/mixed morphology. Regarding tumors located in the small/large bowel, there was no significant difference between pure spindled and epithelioid/mixed-type GISTs for any of the tested clinicopathological parameters or cell-cycle markers (P>0.05; Table 2; Figures 2a and f; Figure 3b).
Site-dependent comparison of tumor size (a), mitotic counts (b), expression of the G1-phase cell-cycle marker cyclin D1 (c), expression of the G1/S-phase marker E2F1 (d), expression of the G2-phase marker cyclin B1 (e) and expression of the G1- to M-phase proliferation marker Ki67 (f) in KIT-mutated GISTs with pure spindled vs epithelioid/mixed-type growth patterns. Significant differences were observed only in gastric GISTs (*P<0.05), but not in small/large bowel GISTs. Epi./mix., epithelioid/mixed; sp., spindled. Shown are box-plots with 0, 25, 50, 75 and 100% quartiles.
KIT-mutated GISTs with epithelioid/mixed-type growth pattern (black boxes) were significantly more often of the high-risk category according to Fletcher et al1 compared with the pure spindled GISTs (gray boxes) in the stomach (a), but not in the small/large bowel (b). Epi./mix., epithelioid/mixed; interm., intermediate; sp., spindled.
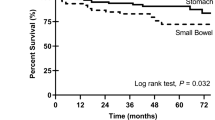
Follow-Up
GISTs with epithelioid/mixed histomorphology had a significantly shorter disease-free survival compared with GISTs with pure spindled histology (P=0.02). A detailed evaluation according to anatomical localization revealed that in gastric GISTs with KIT mutation, an epithelioid/mixed histomorphology was significantly associated with shorter disease-free survival (P=0.003; Figure 4a), whereas among GISTs from small/large bowel, there was no statistically significant difference between spindled and epithelioid/mixed GISTs (P=0.3; Figure 4b).
Discussion
In the current study, we evaluated the prognostic impact of the histomorphological growth pattern in a cohort of 116 primary GISTs with KIT mutation on a tissue microarray. Irrespective of the anatomical localization, GISTs with KIT mutation displayed the pure spindled growth pattern in a significantly higher proportion (72%) compared with the epithelioid/mixed growth pattern (28%). Notably, none of the 116 GIST mutants in this study showed a pure epithelioid phenotype. KIT-mutated GISTs with epithelioid/mixed phenotype were of significantly larger diameters and had significantly higher mitotic counts compared with their pure spindled counterparts, and were frequently of the hypercellular and sarcomatous epithelioid subtypes defined by Miettinen et al2 for gastric GISTs. The latter epithelioid subtypes were found to follow a more aggressive course than the sclerosing and dyscohesive epithelioid subtypes in the studies by Miettinen et al.2, 3 In the current study, gastric GISTs with KIT mutation and epithelioid/mixed phenotypes were significantly more often of the high-risk categories, and had a significantly shorter disease-free survival compared with their counterparts with pure spindled phenotypes. Altogether, these observations suggest that the spindled cytomorphology represents the basic (primary) growth pattern in KIT-mutant GISTs, whereas the epithelioid cytomorphology represents a secondary growth pattern. Consistent with this view, several recent studies on minute early-stage incidental and microscopic KIT-mutant GISTs have demonstrated a uniformly spindled morphology.19, 20, 21
We found a significantly higher expression of the G2-phase cyclin B1 and of the G1- to M-phase marker Ki67, but not of the G1-phase cyclin D1 or of the G1/S-phase transcription factor E2F1, in the epithelioid/mixed type GISTs. These observations suggest that genetic events enabling an accelerated progression through the late phases of the cell cycle may be present in KIT-mutated GISTs with epithelioid/mixed phenotype, whereas in GISTs with pure spindled growth pattern, cell proliferation may commonly be halted at the G1/S-phase restriction point. Alterations of the G1/S-phase transition inhibitor p16INK4A, which are frequently observed in high-risk/malignant GISTs, may contribute to this difference.22, 23 These findings are in line with our previous observation that the presence of epithelioid/mixed components in GISTs with biphasic pattern was associated with higher mitotic activity, higher expression of Ki67 and higher number of chromosomal copy number changes compared with the spindled component in the same tumor.16 In that study, our observations suggested a clonal progression through sequential chromosomal alterations, with a shift in the histomorphological growth pattern from spindled to epithelioid/mixed phenotype.16
Interestingly, the differences in tumor diameter, mitotic counts, expression of cell-cycle proteins and disease-free survival between KIT-mutated GISTs with pure spindled vs epithelioid/mixed phenotypes were only observed in gastric GISTs, whereas there were no significant differences comparing tumors with different growth patterns from the small and large bowel. These site-dependant differences in tumor behavior highlight the biological heterogeneity in GISTs from different anatomical localizations along the GI tract. On the other hand, the predominance of the epithelioid/mixed phenotypes in PDGFRA-mutant GISTs demonstrated in several previous studies7, 8, 13, 14, 15 suggests a primary commitment of this subset of GISTs toward an epithelioid phenotype. This view is supported by the generally favorable clinical course of PDGFRA-mutated GISTs, which contrasts with our findings in epithelioid/mixed KIT-mutant GISTs. These apparently discrepant results with regard to the prognostic significance of the epithelioid/mixed phenotype in gastric GISTs are consistent with the view that these two groups of neoplasms (KIT- and PDGFRA-mutant GISTs) probably represent two distinct clinicopathological and molecular genetic disease entities.
In summary, our study demonstrated that the observation of an epithelioid/mixed phenotype in gastric GISTs with KIT mutation is an unfavorable prognostic parameter, and that the prognostic significance of the epithelioid/mixed phenotype in GISTs has to be interpreted in the context of the genotype and anatomical site of the tumor. The adverse prognostic value of the epithelioid/mixed phenotype in KIT-mutated GISTs needs to be independently validated in larger future studies.
References
Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol 2002;33:459–465.
Miettinen M, Sobin LH, Lasota J . Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol 2005;29:52–68.
Miettinen M, Makhlouf H, Sobin LH, et al. Gastrointestinal stromal tumors of the jejunum and ileum: a clinicopathologic, immunohistochemical, and molecular genetic study of 906 cases before imatinib with long-term follow-up. Am J Surg Pathol 2006;30:477–489.
Hirota S, Isozaki K, Moriyama Y, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science 1998;279:577–580.
Heinrich MC, Corless CL, Duensing A, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science 2003;299:708–710.
Miettinen M, Lasota J . Gastrointestinal stromal tumors: pathology and prognosis at different sites. Semin Diagn Pathol 2006;23:70–83.
Wardelmann E, Hrychyk A, Merkelbach-Bruse S, et al. Association of platelet-derived growth factor receptor alpha mutations with gastric primary site and epithelioid or mixed cell morphology in gastrointestinal stromal tumors. J Mol Diagn 2004;6:197–204.
Lasota J, Dansonka-Mieszkowska A, Sobin LH, et al. A great majority of GISTs with PDGFRA mutations represent gastric tumors of low or no malignant potential. Lab Invest 2004;84:874–883.
Yu CC, Fletcher CD, Newman PL, et al. A comparison of proliferating cell nuclear antigen (PCNA) immunostaining, nucleolar organizer region (AgNOR) staining, and histological grading in gastrointestinal stromal tumors. J Pathol 1992;166:147–152.
Singer S, Rubin BP, Lux ML, et al. Prognostic value of KIT mutation type, mitotic activity, and histologic subtype in gastrointestinal stromal tumors. J Clin Oncol 2002;20:3898–3905.
Fujimoto Y, Nakanishi Y, Yoshimura K, et al. Clinicopathologic study of primary malignant gastrointestinal stromal tumor of the stomach, with special reference to prognostic factors: analysis of results in 140 surgically resected patients. Gastric Cancer 2003;6:39–48.
Rutkowski P, Nowecki ZI, Michej W, et al. Risk criteria and prognostic factors for predicting recurrences after resection of primary gastrointestinal stromal tumor. Ann Surg Oncol 2007;14:2018–2027.
Wasag B, Debiec-Rychter M, Pauwels P, et al. Differential expression of KIT/PDGFRA mutant isoforms in epithelioid and mixed variants of gastrointestinal stromal tumors depends predominantly on the tumor site. Mod Pathol 2004;17:889–894.
Penzel R, Aulmann S, Moock M, et al. The location of KIT and PDGFRA gene mutations in gastrointestinal stromal tumors is site and phenotype associated. J Clin Pathol 2005;58:634–639.
Lasota J, Stachura J, Miettinen M . GISTs with PDGFRA exon 14 mutations represent subset of clinically favorable gastric tumors with epithelioid morphology. Lab Invest 2006;86:94–100.
Agaimy A, Haller F, Gunawan B, et al. Distinct biphasic histomorphological pattern in gastrointestinal stromal tumors (GISTs) with common primary mutations but divergent molecular cytogenetic progression. Histopathology 2009;54:295–302.
Haller F, Gunawan B, von Heydebreck A, et al. Prognostic role of E2F1 and members of the CDKN2A network in gastrointestinal stromal tumors. Clin Cancer Res 2005;11:6589–6597.
Cameron S, Haller F, Dudas J, et al. Immune cells in primary gastrointestinal stromal tumors. Eur J Gastroenterol Hepatol 2008;20:327–334.
Kawanowa K, Sakuma Y, Sakurai S, et al. High incidence of microscopic gastrointestinal stromal tumors in the stomach. Hum Pathol 2006;37:1527–1535.
Agaimy A, Wünsch PH, Hofstaedter F, et al. Minute gastric sclerosing stromal tumors (GIST tumorlets) are common in adults and frequently show c-KIT mutations. Am J Surg Pathol 2007;31:113–120.
Abraham SC, Krasinskas AM, Hofstetter WL, et al. ‘Seedling’ mesenchymal tumors (gastrointestinal stromal tumors and leiomyomas) are common incidental tumors of the esophagogastric junction. Am J Surg Pathol 2007;31:1629–1635.
Schneider-Stock R, Boltze C, Lasota J, et al. High prognostic value of p16INK4 alterations in gastrointestinal stromal tumors. J Clin Oncol 2003;21:1688–1697.
Haller F, Löbke C, Ruschhaupt M, et al. Loss of 9p leads to p16INK4A down-regulation and enables RB/E2F1-dependent cell cycle promotion in gastrointestinal stromal tumors (GISTs). J Pathol 2008;215:253–262.
Acknowledgements
We thank Melanie Gebhardt for excellent technical assistance. We also thank Dr Jens Kuhlgatz (Department of Surgery, Albert-Schweitzer-Hospital, Northeim, Germany) and Dr med Bodo Fleischer (Department of Surgery; Evangelisches Krankenhaus Göttingen-Weende, Göttingen, Germany) for their cooperation and provision of surgical specimens.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Haller, F., Cortis, J., Helfrich, J. et al. Epithelioid/mixed phenotype in gastrointestinal stromal tumors with KIT mutation from the stomach is associated with accelerated passage of late phases of the cell cycle and shorter disease-free survival. Mod Pathol 24, 248–255 (2011). https://doi.org/10.1038/modpathol.2010.188
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.188
Keywords
This article is cited by
-
Prognostic value of KIT/PDGFRA mutations in gastrointestinal stromal tumors: a meta-analysis
World Journal of Surgical Oncology (2014)