Abstract
The 2009 International Society of Urological Pathology Consensus Conference in Boston, made recommendations regarding the standardization of pathology reporting of radical prostatectomy specimens. Issues relating to surgical margin assessment were coordinated by working group 5. Pathologists agreed that tumor extending close to the ‘capsular’ margin, yet not to it, should be reported as a negative margin, and that locations of positive margins should be indicated as either posterior, posterolateral, lateral, anterior at the prostatic apex, mid-prostate or base. Other items of consensus included specifying the extent of any positive margin as millimeters of involvement; tumor in skeletal muscle at the apical perpendicular margin section, in the absence of accompanying benign glands, to be considered organ confined; and that proximal and distal margins be uniformly referred to as bladder neck and prostatic apex, respectively. Grading of tumor at positive margins was to be left to the discretion of the reporting pathologists. There was no consensus as to how the surgical margin should be regarded when tumor is present at the inked edge of the tissue, in the absence of transected benign glands at the apical margin. Pathologists also did not achieve agreement on the reporting approach to benign prostatic glands at an inked surgical margin in which no carcinoma is present.
Similar content being viewed by others
Main
Surgical margin status in radical prostatectomy specimens is a known prognostic parameter for postoperative biochemical recurrence and disease progression of prostate cancer.1, 2, 3, 4, 5, 6, 7 Generally defined as tumor cells reaching the inked surgical margin of the prostatectomy specimen,2 11–38% of radical prostatectomy specimens are reported to have positive surgical margins on pathologic evaluation.8 Progression-free probability for men with surgical margin positivity on radical prostatectomy ranges from 58 to 64%, which contrasts with 81–83% for patients whose radical prostatectomy specimens are surgical margin negative for tumor.9, 10 Additionally, preoperative serum prostate-specific antigen (PSA) levels and percentage of cancer in the core biopsy specimen have been shown to predict surgical margin status, and can be factored into treatment considerations.11
Despite widespread consensus as to the importance and clinical relevance of accurate documentation of surgical margin status of radical prostatectomy specimens in pathology reports, there still exists variability in its articulation by pathologists practicing in different institutions. The requirement for adopting a uniform approach in the evaluation of prognostic features of radical prostatectomy specimens is imperative.8
International Society of Urological Pathology (ISUP) Consensus Conference
To identify the methods and practices most commonly used by urological pathologists worldwide, a web-based survey on handling and reporting of radical prostatectomy specimens was distributed to 255 members of ISUP.
The ISUP survey was followed up with a consensus conference held in conjunction with the 2009 Annual Scientific Meeting of the United States and Canadian Academy of Pathology held in Boston, MA, USA. The aim was to obtain consensus relating to the handling, staging and reporting of radical prostatectomy specimens. Those who completed the electronic survey were invited to attend the consensus conference, which was held on 8 March. The detailed process related to the survey and consensus meeting are reported in an introductory paper.12
Representatives from five working groups appointed to coordinate the consensus process presented background information and results from detailed literature reviews to the meeting. The survey results were then discussed with the objective of achieving agreement on controversial issues. Following this, a ballot was taken on a series of questions that were designed to address these controversial issues and an achievement of 65% agreement on voting was considered to be consensus. With a few exceptions, there was agreement between the survey results and the consensus conference results. The results of the individual working group reports related to specimen handling, T2 substaging, extraprostatic extension and seminal vesicle and lymph node involvement are reported separately.13, 14, 15, 16
Many recommendations of this consensus conference have already been incorporated into international guidelines, including the recent College of American Pathologists protocol and checklist for reporting adenocarcinoma of the prostate, and the structured reporting protocol for prostatic carcinoma from the Royal College of Pathologists of Australasia.17, 18
Definition and criteria for positive surgical margins
A positive surgical margin can be defined as tumor that extends to the surface of the prostate wherein the surgeon has cut across the tissue plane.3 This includes failure to excise extraprostatic extension of prostate carcinoma, as well as intraprostatic (‘capsular’) incision into otherwise organ-confined tumor. Although this appears to be a relatively simple definition, it has practical challenges in its application, as the prostate is surrounded by vital structures such as the urogenital diaphragm distally, the pelvic sidewall laterally, the rectum posteriorly and the bladder neck superiorly. This means that in radical prostatectomy specimens, there is scanty periprostatic tissue, usually <1 mm in width. This results from the deliberate attempt by the surgeon to avoid important adjacent structures and dissect the prostate as closely to its surface as possible.
The concept of considering a surgical margin as negative if the carcinoma does not reach the surface of the radical prostatectomy specimen, despite microscopically close distances of <0.1 mm, has been supported by studies that have documented an absence of residual tumor with a lack of any postoperative disease progression.3, 19 In a study of 278 consecutive margin-negative whole-mount radical prostatectomy cases, Emerson et al20 found that the closest distance between tumor and resection margin, which ranged from 0.02 to 5 mm, did not significantly predict PSA recurrence in univariate or multivariate logistic regression analysis, and concluded that routine pathologic reporting of this distance was not required. It was suggested that even a very close margin is likely to be truly negative, as surgery results in considerable tissue destruction from cautery, vascular disruption and subsequent inflammation. The studies by Epstein19 and Epstein and Sauvageot21 also support the lack of correlation of margin distance with disease recurrence and residual cancer.
Survey and Consensus Conference Results
In the online survey, there was a consensus among respondents that they do not report the actual distance from a negative margin to an adjacent focus of carcinoma (Table 1). In the specific case of posteriorly located tumor separated from the ink by only one fibroblast with a smooth and round prostatic surface, 60% of respondents reported that they regard this as a negative margin, a further 27% stated that they would report the margin as ‘close’, either with or without a measurement, and 4% considered this a positive margin. These responses emphasize the fact that, despite the tumor not reaching the inked margin, almost one-third of respondents were uncomfortable in accepting the separation of carcinoma from the surgical margin by only a single fibroblast as a negative margin.
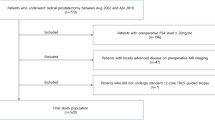
During the consensus conference, there was consensus that tumor extending close to the ‘capsular’/surgical margin, yet not to it (Figure 1a), should be reported as a negative margin.
(a) Although tumor extends close to the inked surface, this has a smooth rounded border and the margin should be diagnosed as negative for tumor without a comment on the proximity of tumor to the margin. (b) Perpendicular margin from the bladder neck showing tumor extending to the inked surface. (c) Shave margin from the bladder neck in which any tumor present is considered to be a positive margin. Note the thick muscle bundles of bladder neck. (d) Focal extraprostatic extension with a positive margin. Note malignant glands at the margin adjacent to adipose tissue. (e) Non-focal extraprostatic extension with a positive margin anteriorly (upper right). Cauterized tumor extends to the margin. Note tumor associated with adipose tissue indicating extraprostatic extension (arrow, lower left). (f) Intraprostatic incision with carcinoma and adjacent benign glands present at the inked surface.
Location of positive surgical margins
Radical prostatectomy specimens are routinely evaluated for margin status at the prostatic apex (distal margin), base (proximal margin at the bladder neck), and circumferentially around the organ—the latter categorized broadly into anterior, posterior, anterolateral and posterolateral. Transition zone and stage T1c tumors have a tendency to show a higher likelihood of positive anterior margins when compared with stage T2 cancers, with the apex being the most common site of a positive margin in both T1c and T2 disease. Other common sites of positive margins include the posterior and posterolateral aspects of the prostate.3 The surgical approach has also been found to impact on the likelihood of location-specific margin positivity, with perineal access being more frequently associated with anterior and bladder neck positive margins, when compared with a retropubic approach.22 Further, Smith et al23 found that the most common location of a positive surgical margin in robotic-assisted laparoscopic and retropubic radical prostatectomy was at the apex. Inter-institutional variation in the specific classification of margins, in particular the circumferential ones, makes it difficult to compare the location of positive margins in radical prostatectomy specimens in various reported series.3
Published reports on the impact of location of positive surgical margins on outcome have been conflicting. Pettus et al4 found that a positive apical margin was unable to independently predict biochemical recurrence. The lack of influence of a positive apical margin on cancer progression has been corroborated by other workers.2 Obek et al24 concluded that positive margins at multiple sites, bladder neck or the posterolateral surface of the prostate increased the risk of disease progression. Other authors have confirmed the significantly increased risk of biochemical recurrence associated with a positive posterolateral margin.25 Saether et al5 reported a greater likelihood of postoperative PSA recurrence with positive margins at the anterior prostate and apex of the prostate on univariate analysis, but that this significance was lost when other risk factors were factored into the multivariate analysis. Somewhat in support of this, Sofer et al26 noted that the location of surgical margin positivity did not independently predict biochemical recurrence.
The bladder neck or prostatic base is an uncommon site for a positive surgical margin (Figures 1b and c). When present, this is usually encountered in the context of positive margins in other parts of the prostate.9 In a study of 364 patients, bladder neck involvement was documented in 6% of cases, with its presence being an independent predictor of early PSA recurrence.27 Although a positive bladder neck margin has been associated with a higher risk for biochemical progression than positive margins observed at other locations, there is some evidence to suggest that this should not be designated as pathologic stage T4. This was affirmed by Aydin et al28 who reported that patients with an isolated positive bladder neck margin had a greater risk of biochemical progression than patients with one or more positive margins at other sites, but that the risk was not as adverse as that associated with stage T4 disease. A recent report by Zhou et al29 supports this view, with time to recurrence of patients in their study, whose radical prostatectomy specimens showed microscopic bladder neck involvement, being similar to those with pT2 disease with positive surgical margins, or pT3a cancer with negative margins. In addition, although bladder neck margin positivity was associated with adverse pathologic parameters, it was not independently predictive of PSA recurrence. A further study by Buschemeyer et al30 concluded that a positive bladder neck margin was associated with progression, similar to that of patients with seminal vesicle invasion.
Survey and Consensus Conference Results
Pathologists who participated in the online survey reported that they generally specify the site in which a positive surgical margin occurs, with 92 and 98% doing so for intraprostatic incision into tumor and extraprostatic extension, respectively.
Consensus agreement was reached at the conference for the uniform reporting of the location of positive margins as posterior, posterolateral, lateral, anterior at the apex and mid-portion of the prostate and the bladder neck.
Although there is no incontrovertible evidence that the specific site of surgical margin positivity independently predicts disease progression, it is still recommended that pathologists specify the location of positive surgical margins in the pathology report, as this provides feedback to the urologist and may assist in facilitating a modification of surgical technique.
Extent of tumor at positive surgical margins
Several studies have shown that the extent of tumor at the surgical margin correlates with postoperative disease recurrence. Epstein et al demonstrated 5-year recurrence-free rates of 87% for margin-negative, 60% for focal margin-positive and 35% for patients with extensive margin-positive tumors, in which focal positivity was defined as limited involvement, with only one or two areas showing tumor extending to margins.9, 19, 21 Emerson et al20 similarly found the extent of positive margins to be a significant prognostic indicator on univariate analysis, though the predictive value of this parameter became marginal when adjusted for Gleason score. Babaian et al,31 using a measurement of 3 mm as a cut point, showed that patients with margin positivity of 3 mm or less had an overall recurrence rate of 14%, in contrast to those with >3 mm of margin involvement, who had an overall recurrence rate of 53%. Corroborating the significance of focal versus extensive margin involvement, Weldon et al6 found PSA recurrence in none of margin-negative, in 26% of focally margin-positive and in 69% of extensively margin-positive patients. Chuang et al32 also confirmed that greater tumor extent at the site of intraprostatic incision with a positive surgical margin was associated with a less favorable prognosis. At variance with the above studies, Marks et al33 evaluated the linear extent of margin positivity in a series of 174 consecutive margin-positive radical prostatectomy specimens, and concluded that extent of margin positivity was not a prognostic factor for PSA recurrence, and hence need not be included in the final pathology report.
Survey and Consensus Conference Results
In the survey it was found that there was consensus among respondent pathologists who specified the extent of margin positivity in areas of extraprostatic extension and intraprostatic incision into tumor. Of these, 42 and 37% respectively reported providing a subjective quantification of the extent of margin positivity, that is, whether there is ‘focal’ versus ‘extensive’ involvement (Figures 1d and e). An almost equal proportion of pathologists (29 and 27%, respectively) noted that they objectively evaluated the amount of tumor at the inked margin either by a measurement in mm, or by stating the number of slides involved.
On the basis of the balance of data, there was a consensus at the conference that the extent of a positive margin be recorded as mm of involvement.
Grade of tumor at positive surgical margins
A study by Chuang et al32 evaluated the impact of capsular/intraprostatic incision, on otherwise organ-confined disease. They found that a Gleason score of 6 versus 7 at the site of intraprostatic incision was not a significant predictor of outcome, but conceded that this conclusion was limited by the small number of cases in their series. To date, there are no firm data relating to the prognostic significance of Gleason pattern and Gleason score of tumor present at the positive surgical margin site, distinct from the established prognostic importance of the Gleason score of tumor within the radical prostatectomy. It is clear that further work is necessary on this topic, but until such time that there are data to indicate otherwise, it would appear reasonable that the grade at the site of surgical margin positivity not be reported.
Survey and Consensus Conference Results
In the survey, there was a consensus among pathologists who reported that they do not provide Gleason pattern or Gleason score of tumor at the site of margin positivity. Furthermore, 85% reported that they did not grade margin-positive tumor in which extraprostatic extension occurs, and 88% did not provide a grade for positive margins resulting from intraprostatic incision into tumor. A small cohort of pathologists stated that they provided a Gleason pattern and Gleason score only when the tumor at the surgical margin is high grade.
This approach was endorsed by consensus conference participants, with agreement that the decision to incorporate the tumor grade at the site of margin positivity into the pathology report, be at the reporting pathologist's discretion until more conclusive data are available.
Intraprostatic (‘capsular’) incision and surgical margins
Intraprostatic incision refers to the inadvertent transection of either benign or malignant prostatic tissue by the urologist during the radical prostatectomy procedure, with a small portion of prostatic tissue remaining within the patient.3, 34 Although in the past this has been referred to as ‘capsular incision’, as the prostate lacks a true capsule, a more appropriate term is ‘intraprostatic incision’. When intraprostatic incision occurs at the site of tumor, it results in a positive surgical margin (Figure 1f) and the reported percentage of cases with positive surgical margins from intraprostatic incision into tumor ranges from 0 to 61%.
The significance of intraprostatic incision into tumor in otherwise organ-confined disease has been debated in the literature, with some studies suggesting that it has no prognostic impact, while others have reported increased risk of postoperative progression. Recently, Chuang et al32 showed single intraprostatic incision into tumor to have a higher associated recurrence rate when compared with organ-confined or focal extraprostatic extension, margin-negative disease. This recurrence rate was, however, lower than that for patients with non-focal, extraprostatic extension, margin-positive tumor, but was instead accompanied by a risk of progression comparable to those with a positive margin in an area of focal extraprostatic extension. Earlier, Shuford et al34 found that intraprostatic incision into tumor had a prognostic significance similar to that of pT3a disease with positive margins.
Important issues concerning the prognostic significance of intraprostatic incision relate to histologic interpretation and the site of occurrence.35 Histological interpretive challenges arise when the tumor shows crush artifact at the inked surgical margin, which may result in under-diagnosis of intraprostatic incision (Figure 2a). A further problem may occur when extraprostatic extension reaching the surgical margin elicits a fibrotic reaction, giving the appearance of incision into organ-confined tumor (Figures 2b and c). There may also be difficulty in differentiating extraprostatic extension involving surgical margins, in the anterior part of the prostate, from intraprostatic incision into tumor, because of the vague histoanatomic boundaries at this site (Figure 2d).
(a) High-grade carcinoma showing crush artifact, extending to the inked margin. (b) Extraprostatic extension of tumor with associated desmoplasia extending to the inked margin rather than intraprostatic incision. (c) Tumor extending to the inked margin in an area of extraprostatic extension (right). The outer border of the prostate is marked by condensed bundles of smooth muscle (arrow heads). Tumor is also in the same plane as adipose tissue (arrows), further denoting extraprostatic extension. (d) Tumor-positive anterior margin. Despite the lack of adjacent benign glands, the tumor is considered extraprostatic as typically there are no benign glands in this part of the prostate. (e) Tumor extends to the inked surface at the apex. It is difficult to determine if the positive margin is associated with intraprostatic incision or extraprostatic extension, because of the ambiguous anatomical boundaries of the prostate in this area. (f) Tumor associated with skeletal muscle extends to the inked surface at the apex. Despite the lack of admixed benign glands, it remains difficult to determine whether the positive margin is due to intraprostatic incision or extraprostatic extension.
The method of sampling of the prostatic apex can affect the rate of reported tumor-positive margins, with shave sections giving rise to a higher frequency of false-positive margins than the cone method.3 As for the anterior part of the prostate, the histological boundaries at the prostatic apex are imprecise, with benign prostatic glands admixed with skeletal muscle fibers originating from the urogenital diaphragm.
There has also been some question as to whether residual benign prostatic tissue, resulting from intraprostatic incision, is a possible cause of elevation of serum PSA postoperatively. Kernek et al36 undertook a detailed study of 199 patients, who underwent radical prostatectomy for prostatic adenocarcinoma and who had cancer-free surgical margins. They assessed the presence, anatomical location and extent of benign prostatic tissue at surgical margins and showed that benign prostatic tissue was more frequently present at the prostatic apex and base than the anterior or posterior parts of the prostate, but that the presence of such benign tissue at the surgical margins had no prognostic relevance.
Survey and Consensus Conference Results
Of the pathologists surveyed, 72% noted that they report intraprostatic/‘capsular’ incision into cancer when it is present. Pathologists were divided in their opinions regarding the concept of intraprostatic incision in relation to the prostatic apex. Of those responding, 53% noted that they did not equate a positive apical margin with intraprostatic incision, while 13% of pathologists regarded a positive apical margin as synonymous with intraprostatic incision. In 30% of responses, pathologists stated that they considered a positive apical margin to indicate intraprostatic incision only when both benign and malignant glands were present at the inked tissue margin.
At the consensus conference, 24% of participants interpreted the presence of tumor at the inked margin, in the absence of transected benign glands at the apical perpendicular margin section, as organ-confined tumor. A further 5% considered this to be extraprostatic extension, and 11% as intraprostatic incision. The remaining 40% would not offer an opinion as they noted that there were no formal criteria available for defining extraprostatic extension at this location. In addition, 69% of pathologists agreed that if tumor was present in skeletal muscle, when no benign glands were included at the apical perpendicular margin, this should be considered as organ-confined tumor. It was recommended that intraprostatic incision should be considered the cause of a positive apical margin only when benign glands were seen in conjunction with tumor reaching the inked surface and when the prostatic apex was sampled using the cone method. In the case of tumor extending to the inked margin at the apex, in the absence of transected benign glands, there was no consensus. Most participants recommended that the margin be reported as positive, but qualifying this with the comment that whether this is due to extraprostatic extension or intraprostatic incision cannot be determined, because of the vague boundaries of the prostate in this region (Figures 2e and f).
In the survey, the majority of pathologists noted that they did not routinely report if benign glands were present at the surgical margin, while 28% stated that they did report this with some elaboration as to the site and extent. During the conference, there was no consensus as to how pathologists should approach the presence of benign glands without carcinoma at the inked margin. Of those voting, 48% documented all instances of benign glands at inked margin, regardless of extent, in their pathology reports. A further 41% recorded cases when there were numerous benign glands at the inked margin as intraprostatic incision into benign glands. The remaining 11% of participants did not mention the presence of benign glands at the inked margin.
Terminology of proximal and distal margins of radical prostatectomy specimens
The terminology of proximal and distal margins in radical prostatectomy specimens is not uniform. The disadvantage of using the terms proximal and distal ‘urethral’ margins is that pathologists may inadvertently regard the urethra as the true margin, while in fact it is the prostatic tissue peripheral to the urethral orifice that is of clinical relevance. This may potentially lead to deliberate incision and sampling around the retracted urethral orifice, thus increasing the likelihood of reporting false-positive surgical margins at the prostatic apex and base. Furthermore, when pathologists use the terms ‘positive proximal urethral’ or ‘positive distal urethral’ margin, urologists may assume the pathologist to be in error as they normally transect the urethra some distance from the prostate and this then retracts back into the prostate.
Survey and Consensus Conference Results
In the survey, 62% of pathologists referred to the proximal margin of the prostate as the ‘bladder neck margin’, while 36% preferred the term ‘basal margin’, 12% the ‘proximal margin’ and 9% the ‘proximal urethral margin’. For the distal margin, 85% designated this the ‘apical margin’, with 12% referring to it as the ‘distal margin’ and 3% as the ‘distal urethral margin’.
The online survey responses indicated that there is mixed practice with respect to the terminology used to describe distal and proximal margins, and for consistency, it is clear that this should be reconciled.
At the conference, there was consensus achieved, with 71% of participants having a preference for the terms bladder neck and prostatic apical margins. Of some interest, there appeared to be a geographic variation in the responses, with bladder neck and prostatic apical margin being favored by 68% of North American pathologists and 45% of non-North American pathologists; while 55% of the latter preferred a variety of alternate designations.
Conclusions
The results of the survey and consensus meeting indicate that there is considerable agreement as to how pathologists interpret and report the status of surgical margins of radical prostatectomy specimens. Histological features that require further clarification include the significance of surgical margins that are extremely close to tumor, the reporting of the grade of tumor present at a positive surgical margin and the significance of reporting of benign glands at the surgical excision margin. Additionally, there were some issues raised as individual comments in the survey; specifically the submission of separate apical margins, the clinical significance of microscopic bladder neck margin positivity and the utility of adjuvant radiotherapy in the context of positive surgical margins and these may benefit from further study and discussion.
References
Watson RB, Civantos F, Soloway MS . Positive surgical margins with radical prostatectomy: detailed pathological analysis and prognosis. Urology 1996;48:80–90.
Cheng L, Darson MF, Bergstralh EJ, et al. Correlation of margin status and extraprostatic extension with progression of prostate carcinoma. Cancer 1999;86:1775–1782.
Epstein JI, Amin M, Boccon-Gibod L, et al. Prognostic factors and reporting of prostate carcinoma in radical prostatectomy and pelvic lymphadenectomy specimens. Scand J Urol Nephrol Suppl 2005;216:34–63.
Pettus JA, Weight CJ, Thompson CJ, et al. Biochemical failure in men following radical retropubic prostatectomy: impact of surgical margin status and location. J Urol 2004;172:129–132.
Saether T, Sorlien LT, Viset T, et al. Are positive surgical margins in radical prostatectomy specimens an independent prognostic marker? Scand J Urol Nephrol 2008;42:514–521.
Weldon VE, Tavel FR, Neuwirth H, et al. Patterns of positive specimen margins and detectable prostate specific antigen after radical perineal prostatectomy. J Urol 1995;153:1565–1569.
Wieder JA, Soloway MS . Incidence, etiology, location, prevention and treatment of positive surgical margins after radical prostatectomy for prostate cancer. J Urol 1998;160:299–315.
Montironi R, Cheng L, Mazzucchelli R, et al. Pathological definition and difficulties in assessing positive margins in radical prostatectomy specimens. BJU Int 2009;103:286–288.
Epstein JI, Partin AW, Sauvageot J, et al. Prediction of progression following radical prostatectomy. A multivariate analysis of 721 men with long-term follow-up. Am J Surg Pathol 1996;20:286–292.
Ohori M, Wheeler TM, Kattan MW, et al. Prognostic significance of positive surgical margins in radical prostatectomy specimens. J Urol 1995;154:1818–1824.
Cheng L, Slezak J, Bergstralh EJ, et al. Preoperative prediction of surgical margin status in patients with prostate cancer treated by radical prostatectomy. J Clin Oncol 2000;18:2862–2868.
Egevad L, Srigley JR, Delahunt B . International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens: rationale and organization. Mod Pathol 2010 (in press).
Samaratunga H, Montironi R, True L, et al. International Society of Urological Pathologists (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. Working group 1: specimen handling. Mod Pathol 2010 (in press).
van der Kwast T, Amin MB, Billis A, et al. International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. Working group 2: T2 substaging and prostate cancer volume. Mod Pathol 2010 (in press).
Magi-Galluzzi C, Evans A, Delahunt B, et al. International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. Working group 3: extraprostatic extension, lymphovascular invasion and locally advanced disease. Mod Pathol 2010 (in press).
Berney D, Wheeler T, Grignon D, et al. International Society of Urological Pathology (ISUP) consensus conference on handling and staging of radical prostatectomy specimens. Working group 4: seminal vesicles and lymph nodes. Mod Pathol 2010 (in press).
Srigley JR, Humphrey PA, Amin MB, et al. Protocol for the examination of specimens from patients with carcinoma of the prostate gland. Arch Pathol Lab Med 2009;133:1568–1576.
Kench J, Clouston D, Delahunt B, et al. Royal College of Pathologists of Australasia Prostate Cancer (Radical Prostatectomy) Structured Reporting Protocol. 2010, 54 pp. http://www.rcpa.edu.au/Publications/StructuredReporting/CancerProtocols.htm.
Epstein JI . Evaluation of radical prostatectomy capsular margins of resection. The significance of margins designated as negative, closely approaching, and positive. Am J Surg Pathol 1990;14:626–632.
Emerson RE, Koch MO, Daggy JK, et al. Closest distance between tumor and resection margin in radical prostatectomy specimens: lack of prognostic significance. Am J Surg Pathol 2005;29:225–229.
Epstein JI, Sauvageot J . Do close but negative margins in radical prostatectomy specimens increase the risk of postoperative progression? J Urol 1997;157:241–243.
Salomon L, Anastasiadis AG, Levrel O, et al. Location of positive surgical margins after retropubic, perineal, and laparoscopic radical prostatectomy for organ-confined prostate cancer. Urology 2003;61:386–390.
Smith Jr JA, Chan RC, Chang SS, et al. A comparison of the incidence and location of positive surgical margins in robotic assisted laparoscopic radical prostatectomy and open retropubic radical prostatectomy. J Urol 2007;178:2385–2389.
Obek C, Sadek S, Lai S, et al. Positive surgical margins with radical retropubic prostatectomy: anatomic site-specific pathologic analysis and impact on prognosis. Urology 1999;54:682–688.
Eastham JA, Kuroiwa K, Ohori M, et al. Prognostic significance of location of positive margins in radical prostatectomy specimens. Urology 2007;70:965–969.
Sofer M, Hamilton-Nelson KL, Civantos F, et al. Positive surgical margins after radical retropubic prostatectomy: the influence of site and number on progression. J Urol 2002;167:2453–2456.
Poulos CK, Koch MO, Eble JN, et al. Bladder neck invasion is an independent predictor of prostate-specific antigen recurrence. Cancer 2004;101:1563–1568.
Aydin H, Tsuzuki T, Hernandez D, et al. Positive proximal (bladder neck) margin at radical prostatectomy confers greater risk of biochemical progression. Urology 2004;64:551–555.
Zhou M, Reuther AM, Levin HS, et al. Microscopic bladder neck involvement by prostate carcinoma in radical prostatectomy specimens is not a significant independent prognostic factor. Mod Pathol 2009;22:385–392.
Buschemeyer III WC, Hamilton RJ, Aronson WJ, et al. Is a positive bladder neck margin truly a T4 lesion in the prostate specific antigen era? Results from the SEARCH Database. J Urol 2008;179:124–129.
Babaian RJ, Troncoso P, Bhadkamkar VA, et al. Analysis of clinicopathologic factors predicting outcome after radical prostatectomy. Cancer 2001;91:1414–1422.
Chuang AY, Nielsen ME, Hernandez DJ, et al. The significance of positive surgical margin in areas of capsular incision in otherwise organ confined disease at radical prostatectomy. J Urol 2007;178:1306–1310.
Marks RA, Koch MO, Lopez-Beltran A, et al. The relationship between the extent of surgical margin positivity and prostate specific antigen recurrence in radical prostatectomy specimens. Hum Pathol 2007;38:1207–1211.
Shuford MD, Cookson MS, Chang SS, et al. Adverse prognostic significance of capsular incision with radical retropubic prostatectomy. J Urol 2004;172:119–123.
Chuang AY, Epstein JI . Positive surgical margins in areas of capsular incision in otherwise organ-confined disease at radical prostatectomy: histologic features and pitfalls. Am J Surg Pathol 2008;32:1201–1206.
Kernek KM, Koch MO, Daggy JK, et al. The presence of benign prostatic glandular tissue at surgical margins does not predict PSA recurrence. J Clin Pathol 2005;58:725–728.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
The members of the ISUP Prostate Cancer Group are the following:
Adebowale Adeniran, Hikmat Al-Ahmadie, Ferran Algaba, Robert Allan, Mahul Amin, Marc Barry, Sheldon Bastacky, Dilek Baydar, Louis Bégin, Dan Berney, Athanase Billis, Liliane Boccon-Gibod, David Bostwick, Maria Brito, Tucker Burks, Christer Busch, Philippe Camparo, Liang Cheng, Cynthia Cohen, Milton Datta, Laurence de Leval, Brett Delahunt, Warick Delprado, Lars Egevad, Jonathan Epstein, Andrew Evans, Sara Falzarano, Samson Fine, Eddie Fridman, Bungo Furusato, Masoud Ganji, Lisa Glantz, Anuradha Gopalan, David Grignon, Rainer Grobholz, Charles Guo, Rekha Gupta, Bora Gurel, Seife Hailemariam, Ardeshir Hakam, Omar Hameed, Donna Hansel, R-Peter Henke, Mehsati Herawi, Michelle Hirsch, Jiaoti Huang, Wei Huang, Christina Hulsbergen van de Kaa, Peter Humphrey, Kenneth Iczkowski, Edward Jones, Michael Jones, Laura Jufe, James Kench, Hyun-Jung Kim, Peter Kragel, Glen Kristiansen, Katia Ramos Moreira Leite, Claudio Daniel Lewin, Josep Lloreta, Antonio Lopez- Beltran, Scott Lucia, Daniel Luthringer, Cristina Magi-Galluzzi, Peter McCue, Teresa McHale, Jesse McKenney, Maria Merino, Rodolfo Montironi, Gabriella Nesi, George Netto, Esther Oliva, Pedro Oliveira, Adeboye Osunkoya, Gladell Paner, Anil Parwani, Maria Picken, Galina Pizov, Andrew Renshaw, Jae Ro, Stephen Rohan, Ruben Ronchetti, Mark Rubin, Hemamali Samaratunga, Anna Sankila, Alan Schned, Isabell Sesterhenn, Ahmed Shabaik, Rajal Shah, Jonathan Shanks, Steven Shen, Jungweon Shim, Taizo Shiraishi, VO Speights, Jr, John Srigley, Ming-Tse Sung, Sueli Suzigan, Hiroyuki Takahashi, Puay Hoon Tan, Bernard Tetu, Satish Tickoo, John Tomaszewski, Patricia Troncoso, Kiril Trpkov, Lawrence True, Toyonori Tsuzuki, Jennifer Turner, Theo van der Kwast, Mark Weiss, Thomas Wheeler, Kirk Wojno, Keith Volmar, Chin-Lee Wu, Jorge Yao, Asli Yilmaz, Jim Zhai.
Rights and permissions
About this article
Cite this article
Tan, P., Cheng, L., Srigley, J. et al. International Society of Urological Pathology (ISUP) Consensus Conference on Handling and Staging of Radical Prostatectomy Specimens. Working group 5: surgical margins. Mod Pathol 24, 48–57 (2011). https://doi.org/10.1038/modpathol.2010.155
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2010.155
Keywords
This article is cited by
-
Radiologic-pathologic correlation of prostatic cancer extracapsular extension (ECE)
Insights into Imaging (2023)
-
MRI index lesion radiomics and machine learning for detection of extraprostatic extension of disease: a multicenter study
European Radiology (2021)
-
The impact of surgical margin status on prostate cancer-specific mortality after radical prostatectomy: a systematic review and meta-analysis
Clinical and Translational Oncology (2020)
-
Extent of positive surgical margins following radical prostatectomy: impact on biochemical recurrence with long-term follow-up
BMC Urology (2019)
-
Preoperative staging using magnetic resonance imaging and risk of positive surgical margins after prostate-cancer surgery
Prostate Cancer and Prostatic Diseases (2019)