Abstract
Mutation detection plays an important role in diagnostic pathology, not only in providing a tissue diagnosis, but also in predicting response to antitumourigenic agents. However, mutation detection strategies are often hampered by masking of mutant alleles by wild-type sequences. Coamplification at lower denaturation temperature PCR (COLD-PCR) reportedly increases the proportion of rare variant sequences in a wild-type background by using PCR cycles in which the denaturation temperature is reduced to favour product formation with lower melt temperatures and heteroduplexes arising from minor variants. Intramuscular myxoma is a rare benign soft tissue neoplasm that occurs sporadically and less commonly in association with fibrous dysplasia (Mazabraud's syndrome). Fibrous dysplasia results from activating GNAS1 mutations, and the same mutations have been identified in small numbers of intramuscular myxoma. The aim of the study was primarily to establish whether COLD-PCR is more sensitive than conventional PCR; this was achieved by testing for GNAS1 mutations in intramuscular myxomas using the two methodologies. Mutations were detected in 8 of 28 (29%) cases of intramuscular myxomas using conventional PCR followed by mutation-specific restriction enzyme digestion (PCR-MSRED) whereas 17 of 28 (61%) mutations were detected using COLD-PCR/MSRED. Mutations were detected in two cases where a diagnosis of low-grade myxofibrosarcoma had been favoured over intramuscular myxoma. No mutations were detected in an additional 9 low-grade and 19 high-grade myxofibrosarcomas, and another 40 control samples. This study shows the power of COLD-PCR compared with conventional PCR in mutation detection, and shows that GNAS1 mutation detection increases diagnostic accuracy when distinguishing between intramuscular myxoma and low-grade myxofibrosarcoma.
Similar content being viewed by others
Main
Mutation detection can be a powerful adjunct to diagnostic histopathology when combined with microscopic features. It can be helpful in distinguishing morphologically similar neoplasms, such as superficial fibromatosis and low-grade fibromyxoid sarcoma from desmoid-type fibromatosis, and reactive fibrous proliferation from fibrous dysplasia.1, 2 More recently, mutation detection has been found to be an important predictive factor in response to antitumourigenic agents. Specifically, it has been shown that the detection of a K-RAS mutation is a predictor of resistance to therapy directed against the receptor tyrosine kinase, EGFR, in large bowel adenocarcinoma and non-small cell lung carcinoma.3, 4 However, mutation detection can be hampered as a consequence of dilution by wild-type sequences, and for this reason, it is generally recommended that at least 50% of tissue analysed for mutations should be lesional; this may require tedious painstaking microdissection of the relevant tissue. Therefore, any method that increases mutation detection sensitivity would be a useful and valuable methodological development. COLD-PCR is potentially such a technique, as it reportedly increases the proportion of rare variant sequences in a wild-type background by using PCR cycles in which the denaturation temperature is reduced to favour amplification of products with lower melt temperatures and heteroduplexes formed between minor variants and wild-type sequences.5
Intramuscular myxoma is a rare benign myxoid spindle cell neoplasm that generally occurs as an isolated lesion, although it can be part of Mazabraud's syndrome, a combination of intramuscular myxoma with fibrous dysplasia.6 GNAS1 mutations were detected in fibrous dysplasia following the discovery that they occurred in sporadic endocrine neoplasms.7, 8 It was also recognised that these mutations occurred as somatic post-zygotic events, and resulted in a mosaic distribution of mutation-bearing cells.8 However, it was only in 2000, that the same GNAS1 mutations were detected in intramuscular myxoma, and to date, there have only been seven reported cases: two (one R201H and one R201C) of these occurred as non-syndromic cases and five (four R201H and one R201C) occurred as part of Mazabraud's syndrome.1, 9
Intramuscular myxomas are generally hypocellular and hypovascular neoplasms composed of spindle and stellate cells, exhibiting minimal nuclear atypia, embedded within a myxoid stroma.10 These tumours can be difficult to distinguish from low-grade myxofibrosarcoma, particularly the cellular variant, as neither have a genetic signature and both have a non-specific immunohistochemical profile and show variable expression of smooth muscle actin, and are typically negative for S100.11, 12
The aim of this study was to determine the incidence of GNAS1 mutations in intramuscular myxomas using COLD-PCR and conventional PCR.
Materials and methods
Clinical Information, Tumour and Control Material Selection
The study complied with the Central Office for Research Ethics Committee's standards. All cases were retrieved from the pathology archives of the Royal National Orthopaedic Hospital and the patients’ notes were reviewed for clinical outcome. A total of 24 cases of non-syndromic intramuscular myxoma (13 classical and 11 cellular variants), and 2 cases of intramuscular myxoma associated with fibrous dysplasia (Mazabraud's syndrome) were included in the study. The cellular variants of intramuscular myxoma were characterised by an increase in vascularity and cellularity comprising between 10 and 80% of the tumour.13 In all, 28 cases of myxofibrosarcoma (9 Grade 1, 19 Grades 2 or 3) classified according to the French Federation of Cancer Centres (FNCLCC) grading system14 were also studied. In addition, two cases were included where a definitive diagnosis had not been given, although a low-grade myxofibrosarcoma was favoured over intramuscular myxoma. All intramuscular myxoma and myxofibrosarcomas were immunohistochemically negative for S100 protein, smooth muscle actin and desmin expression. None of the patients had documented evidence of café-au-lait spots, which would indicate McCune Albright syndrome (combination of fibrous dysplasia, café-au-lait spots and endocrine tumours).8
Control material included 10 cases of osteofibrous dysplasia that has been previously reported as not harbouring GNAS1 mutations when screened by conventional PCR and mutation-specific restriction enzyme digestion (MSRED).1 In addition, DNA samples from 30 formalin-fixed paraffin-embedded lymphomas known to have relatively poor quality nucleic acid with variable degrees of DNA degradation and yield, which had been previously analysed in other studies, were analysed for the GNAS1 mutations by COLD-PCR. The purpose of this was to determine whether false-positive results would be generated from such material due to Taq polymerase errors that may occur in low quality or quantity template.5
All materials included were from resection specimens that had been fixed in 10% buffered formaldehyde for not more than 48 h, and were paraffin embedded. The haematoxylin and eosin-stained sections and immunohistochemistry of the tumours were reviewed by three Consultant Histopathologists (DD, RT and AMF), and the original diagnoses remained unchanged.
The intramuscular myxoma cases were screened for the two most common GNAS1 mutations associated with fibrous dysplasia (R201H, R201C) using conventional PCR and MSRED analysis as described previously.1 All cases were also studied by COLD-PCR.5 In addition, paired normal tissue (skeletal muscle) from 11 of the patients with intramuscular myxoma was studied.
Two 10-μm thick sections were cut from paraffin-embedded tissue, and DNA was extracted using proteinase K. For conventional PCR, the reaction mixture (50 μl) contained approximately 50 ng of genomic DNA, 12.5 pmol of each primer (Table 1), 200 μM each dNTP and 1 U of Thermal Activated Polymerase (TAP; CLP, Northampton, Northamptonshire, UK) in TAP reaction buffer. PCR consisted of an initial incubation period of 15 min at 95°C followed by 40 cycles of denaturation for 45 s at 93°C, annealing for 45 s at 60°C and strand elongation for 90 s at 72°C. PCR products (5 μl) were incubated at 37°C for 3 h with 1 × reaction buffer and 5 U of the appropriate enzyme according to the manufacturer's instructions (New England Biolabs, Hitchin, Hertfordshire, UK). Products were separated through an 8% polyacrylamide gel and visualised using the Bio-Rad Gel Doc 2000TM system (Bio-Rad, Hemel Hempstead, Hertfordshire, UK). Positive controls (proven by DNA sequencing, and MSRED) were included for the two R201 mutations.
The cycling parameters for COLD-PCR were optimised using a gradient of annealing temperatures from 80 to 90°C, and by trial and error of other parameters using the published guidelines with both conventional and real-time PCR protocols.5 The COLD-PCR protocols giving the best enhancement of mutant detection were adopted as follows:
R201C (DdeI digestion): Reaction mixtures (50 μl) containing approximately 50 ng genomic DNA, 10 pmol of each primer (Table 1), 200 μM each dNTP, 1.5 mM MgCl2 and 1 U Amplitaq GOLD (Applied Biosystems, Foster City, CA, USA) in 1 × buffer II were subjected to 95°C for 7 min, then 10 cycles of 93°C for 45 s, 65°C for 45 s (decreasing by 1°C per cycle to 56°C) and 72°C for 1 min 30 s, then 40 cycles of 84.8°C for 3 s, 56°C for 45 s and 72°C for 1 min 30 s (with an extra 5 min at 72°C on the final cycle.) A Mastercycler conventional thermal cycler was used (Eppendorf, Cambridge, Cambridgeshire, UK). Amplification of specific products was confirmed by size analysis on an 8% polyacrylamide gel followed by DdeI digestion of 5 μl product for 3 h and 8% polyacrylamide gel analysis.
R201H (NcoI digestion): Reaction mixtures (25 μl) containing approximately 50 ng genomic DNA, 5 pmol each primer (Table 1) and 1 × iQ SYBR Green Supermix (Bio-Rad, Hemel Hempstead, Herts., UK) were subjected to 95°C for 3 min, then 10 cycles of 95°C for 15 s, 60°C for 30 s and 72°C for 30 s, then 40 cycles of 95°C for 15 s, 70°C for 8 min, 84.5°C for 3 s, 60°C for 30 s and 72°C for 30 s. An iCycler iQ real-time detection system was used (Bio-Rad). Amplification of specific products that melt at approximately 84°C was confirmed by melt-curve analysis followed by NcoI digestion of 3 μl product for 3 h, and 8% polyacrylamide gel analysis.
DNA samples that failed to yield specific products, comparable to positive controls in intensity by COLD-PCR were repeated and excluded from restriction digestion if subsequently negative. To estimate relative sensitivities of conventional versus COLD-PCR, one case positive for R201C and one positive for R201H, using both methods, were serially diluted with wild-type DNA (1:2; 1:4; 1:8, 1:16 and 1:32 and 1:64) and analysed using MSRED using conventional and COLD-PCR.
The imaging of the intramuscular myxoma was reviewed, and none of the lesions was shown on imaging to be related to a joint, thereby largely excluding the diagnosis of juxta-articular myxomas.15 If the appropriate imaging was available, there was no associated degenerative joint disease. A bone scan was not performed in any of the patients.
Results
Clinical Information and Histopathology
Review of the histopathology showed the classical features of intramuscular myxoma in 15 cases.10 These were paucicellular and hypovascular tumours, composed of a population of spindle and stellate cells with small amounts of fibrillary eosinophilic cytoplasm, in which all the nuclei had fine chromatin. The tumour cells were embedded in abundant myxoid stroma with pseudocystic areas, and microscopically the tumours were poorly delineated and entrapped skeletal muscle fibres (Figure 1). The 11 cases classified as cellular myxomas according to the criteria employed by Nielsen et al13 exhibited a significant degree of intratumoural vascularity, and although the nuclear features were largely similar to the classic variant of intramuscular myxoma, there was some nuclear enlargement and irregularity making it sometimes difficult to distinguish from low-grade myxofibrosarcoma (Figure 1). Some of the cellular intramuscular myxoma included a significant macrophage/muciphage population (Figure 1). The low-grade myxofibrosarcomas, and the two cases where this diagnosis was favoured over intramuscular myxoma, showed largely similar features except that the nuclei exhibited a greater degree of hyperchromasia (Figure 1). The 19 high-grade myxofibrosarcomas, with characteristic features, such as marked nuclear pleomorphism, mitotic activity and necrosis, focally exhibited low-grade areas (not shown).
Representative photomicrographs of haematoxylin and eosin-stained sections of a conventional, paucicellular, intramuscular myxoma with pseudocystic change (a), cellular intramuscular myxoma (b), low-grade fibromyxoid sarcoma (d), and high power views of an intramuscular myxoma (e) and a low-grade myxofibrosarcoma (f). Immunohistochemistry for CD68 highlights the macrophage population (c) occurring in the cellular intramuscular myxoma (b). Bar (a–d)=200 μm. Bar (e–f)=20 μm.
Of the 37 low-grade myxoid tumours (intramuscular myxoma and low-grade myxofibrosarcoma), 30 cases were excised marginally and the remaining 7 were widely excised. There were no intralesional excisions, and none were treated with radiotherapy. None of the intramuscular myxoma recurred (follow-up period 12–60 months; mean 25 months), whereas of the 9 low-grade myxofibrosarcoma 3 recurred (follow-up period 10–71 months; mean 30 months).
Mutation Detection
Using conventional PCR-MSRED, eight GNAS1 mutations, four R201H and four R201C were detected in five conventional and three cellular intramuscular myxomas diagnosed on the morphology. COLD-PCR–MSRED confirmed these results and revealed mutations in an additional nine cases, five R201H and four R201C (Table 2; Figure 2). These included 4 of the 11 cellular variants of intramuscular myxoma, both cases of Mazabraud's syndrome, and the 2 cases where a low-grade myxofibrosarcoma was favoured over an intramuscular myxoma (Tables 2 and 3). In toto, COLD-PCR revealed that 17 low-grade myxoid lesions harboured GNAS1 mutations, thereby more than doubling the mutation detection of these mutations in intramuscular myxomas. Analysis of DNA from the remaining low-grade myxoid tumours, high-grade myxofibrosarcoma, osteofibrous dysplasia, lymphoma, and normal (non-lesional) tissue from intramuscular myxoma patients revealed no mutations by COLD-PCR (Table 2). Of 30 negative control cases, which had low-quality DNA, 6 failed to yield a product with one or both targets and none showed mutations by COLD-PCR (Table 2).
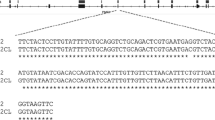
Polyacrylamide gel showing mutation-specific restriction enzyme digestion of GNAS1 R201C (DdeI digests). Upper panel with conventional PCR, lower panel with COLD-PCR. Lane M, molecular weight markers (100–400 bp); lane 1, wild-type control; lanes 2–6, positive control diluted with wild-type DNA as follows: lane 2, 1:2; lane 3, 1:4; lane 4, 1:16; lane 5, 1:32; lane 6, 1:64.
Dilution experiments showed that COLD-PCR increased the sensitivity of mutation detection by eightfold for R201C and fourfold for R201H.
Discussion
COLD-PCR enabled GNAS1 mutations to be detected in 61% of intramuscular myxoma compared with only 29% of cases using conventional PCR. This confirms that this recently published technology is a powerful tool5 and potentially a valuable adjunct in research and diagnostic pathology. The mutations in intramuscular myxoma were detected despite the relatively low number of lesional cells in the tumours, accounted for by the macrophage infiltrate, in addition to the paucicellular nature of intramuscular myxoma. This result shows that it is likely that the more sensitive nature of COLD-PCR can be employed more effectively than conventional PCR in other diagnostic settings and reduces the need for microdissection of lesional material.
Obtaining information concerning the mutation status of a tumour before treatment is becoming more important as new drugs are being designed, and the discovery that the presence and absence of mutations plays a role in determining response to treatment. There is always concern that failure to detect mutations may be accounted for by the lack of sensitivity of a test, and one of the reasons for this includes the presence of a low ratio of mutant to wild-type alleles in lesional tissue which could result in masking of mutant sequences. This problem can be partly overcome by microdissection of lesional tissue to enrich for the cells of interest. However, apart from this technique being very time-consuming and tedious, it is not always possible to select the lesional cells effectively because they are so intimately admixed with the contaminating population. Therefore, the use of COLD-PCR appears to be an attractive option for improved mutation detection.
The introduction of all new methodologies must be tested rigorously before being introduced in the diagnostic setting. In this particular case, the benefit of increased sensitivity must be balanced against the theoretical risk of amplification of Taq polymerase errors. However, this has been largely excluded in the current study as repeated testing of control material including nucleic acid from lymphoma, paired normal matched material, osteofibrous dysplasia and myxofibrosarcomas, including samples with poor DNA quality and low template levels, failed to produce false-positive signals.
The COLD-PCR protocols adopted were selected on the basis of optimum performance determined by trial and error using end-point and SYBR Green real-time PCR techniques. This resulted in selection of one end-point and one real-time PCR protocol. This is inconvenient in practise, and we intend to further optimise to produce a single, simplified approach for all mutations.
COLD-PCR was carried out using different Taq polymerase enzymes (Amplitaq GOLD in end-point PCR and iTaq DNA polymerase in real-time PCR) to the original experiments (TAP DNA polymerase). This is unlikely to have significantly influenced the results as we have shown comparable COLD-PCR data with different Taq DNA polymerase enzymes using positive controls.
In contrast to detecting GNAS1 mutations in only 61% of intramuscular myxoma by COLD-PCR, our previous screen for GNAS1 mutations in fibrous dysplasia using conventional PCR revealed mutations in 93% of 28 cases.1 Why it should be easier to detect GNAS1 mutations in fibrous dysplasia compared with intramuscular myxoma is unclear and may not be fully accounted for by the low cellularity and low tumour proportion of intramuscular myxoma as 7 of the 11 mutation-negative intramuscular myxoma cases were of the cellular variant. An alternative explanation is that as GNAS1 is under tissue specific imprinting control, so that the gene may be differentially expressed in bone and skeletal tissue.16
The study shows for the first time that the majority, 58% (15/26)), of apparent non-syndromic intramuscular myxoma, diagnosed on the basis of microscopy, harbour one of the GNAS1 mutations (R201C and R201H). This raises the possibility that the pathogenesis of this disease is the consequence of a post-zygotic mutation and is largely similar to the development of fibrous dysplasia and some endocrine neoplasms, which harbour the same mutations, and which may co-exist in a mosaic distribution of disease. The existence of silent fibrous dysplasia lesion/s in these patients with the intramuscular myxoma cannot be excluded, as it is not current practice to screen for a skeletal lesion when a diagnosis of intramuscular myxoma is made. Furthermore, it is known that fibrous dysplasia can be asymptomatic because the disease on occasions presents as a pathological fracture, and can be diagnosed as late as 60 years of age when it is detected as a coincidental finding when imaging for some other reason.1 Therefore, as Hannon et al17 found that a significant proportion of children who presented with fibrous dysplasia had subclinical endocrine abnormalities, it is worth considering that patients with intramuscular myxoma may also have other manifestations of this mosaic disorder, including fibrous dysplasia, endocrine abnormalities and café-au-lait spots.
It is also possible that at least some of the GNAS1 mutation-negative intramuscular myxoma harbour a Q227 mutation, which occurs in a small proportion of cases of fibrous dysplasia.1 However, as the prime aim of this study was to compare the sensitivity of conventional with COLD-PCR, the rare GNAS1 mutations previously described in fibrous dysplasia, McCune Albright syndrome and isolated endocrine neoplasms (R201G, R201S, R201P, R201L, Q227L, Q227R, Q227K and Q227H) have not been analysed as it was considered beyond the scope of this study.1, 18
The major differential diagnoses when considering intramuscular myxoma are other low-grade myxoid neoplasms, including low-grade fibromyxoid sarcoma, myxoid liposarcoma, extraskeletal myxoid chondrosarcoma, myxoid variants of nerve sheath tumour and smooth muscle tumour. Fortunately, in the majority of cases, a diagnosis can be reached by interpreting the haematoxylin and eosin-stained sections in the light of immunohistochemistry and/or molecular genetic studies.19, 20, 21, 22 In contrast, a low-grade myxofibrosarcoma can be difficult to distinguish from a cellular intramuscular myxoma because of the absence of an immunohistochemical phenotype and a well-established molecular signature. The benefit of this study is that the detection of a GNAS1 mutation can be helpful in such cases, and in this series, it allowed provision of a confident diagnosis of intramuscular myxoma where previously a low-grade myxofibrosarcoma was favoured. Nevertheless, the failure to detect a GNAS1 mutation in approximately 40% of the cases, which we considered were morphologically typical for intramuscular myxoma, also shows that as a diagnostic test, it has its limitations. The presence of a complex cytogenetic abnormality would favour a diagnosis of a myxofibrosarcoma over an intramuscular myxoma as there is only one report of a cytogenetic abnormality, a small clone of trisomy 18, in the latter.23 In contrast, myxofibrosarcomas have been shown to have both normal and abnormal karyotypes with the cytogenetic aberrations becoming more complex with recurrences and the progression to a higher grade tumour.24 Unfortunately, frozen tissue was not available from the mutation-negative lesions that were diagnosed as cellular intramuscular myxoma, and therefore, we were unable to undertake further investigation of these tumours. Finally, intramuscular myxoma can be indistinguishable from juxta-articular myxoma, but this diagnosis can be largely excluded by imaging.
In conclusion, the study highlights the importance of knowing the sensitivity and specificity of any test before employing it in the clinic, and the value of being aware of new technology that might improve the sensitivity of any diagnostic evaluation.
References
Idowu BD, Al-Adnani M, O’Donnell P, et al. A sensitive mutation-specific screening technique for GNAS1 mutations in cases of fibrous dysplasia: the first report of a codon 227 mutation in bone. Histopathology 2007;50:691–704.
Amary MF, Pauwels P, Meulemans E, et al. Detection of beta-catenin mutations in paraffin-embedded sporadic desmoid-type fibromatosis by mutation-specific restriction enzyme digestion (MSRED): an ancillary diagnostic tool. Am J Surg Pathol 2007;31:1299–1309.
Pao W, Wang TY, Riely GJ, et al. KRAS mutations and primary resistance of lung adenocarcinoma to Gefitinib or Erlotinib. PLoS Med 2005;2:e17.
Lievre A, Bachet JB, Le Corre D, et al. KRAS mutation status is predictive of response to Cetuximab therapy in colon cancer. Cancer Res 2006;66:3992–3995.
Li J, Wang L, Mamon H, et al. Replacing PCR with COLD-PCR enriches variant DNA sequences and redefines the sensitivity of genetic testing. Nat Med 2008;15:579–584.
Mazabraud A, Semat P, Roze R . A propos de l’association de fibromyxomes des tissus mous a la dysplasie fibreuse des os. Presse Med 1967;75:2223–2228.
Landis CA, Masters SB, Spada A, et al. GTPase inhibiting mutations activate the alpha chain of Gs and stimulate adenylate cyclase in human pituitary tumours. Nature 1989;340:692–696.
Albright F, Butler AM, Hampton AO, et al. Syndrome characterised by osteitis fibrosa disseminate, areas of pigmentation and endocrine dysfunction, with precocious puberty in females: report of five cases. N Engl J Med 1937;216:727–746.
Okamoto S, Hisaoka M, Ushijima M, et al. Activating Gsalpha mutation in intramuscular myxomas with and without activating fibrous dysplasia of bone. Virchows Arch 2000;437:133–137.
Enzinger FM . Intramuscular myxoma. A review and follow up study of 34 cases. Am J Clin Pathol 1965;43:104–113.
Miettinen M, Hockerstedt K, Reitamo J, et al. Intramuscular Myxoma—A clinicopathological study of twenty-three cases. Am J Clin Pathol 1985;84:265–272.
Lombardi T, Lock C, Samson J, et al. S100, alpha-smooth muscle and cytokeratin 19 immunohistochemistry in ondontogenic and soft tissue myxomas. J Clin Pathol 1995;48:759–762.
Nielsen GP, O’Connell JX, Rosenberg AE . Intramuscular myxoma. A clinicopathological study of 51 cases with emphasis on hypercellular and hypervascular variants. Am J Surg Pathol 1998;22:1222–1227.
Trojani M, Contesso G, Coindre JM, et al. Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system. Int J Cancer 1984;33:37–42.
Meis JM, Enzinger FM . Juxta-articular myxoma: a clinical and pathologic study of 65 cases. Hum Pathol 1992;23:639–646.
Mantovani G, Ballare E, Giammona E, et al. The Gsalpha gene: predominant maternal origin of transcription in human thyroid gland and gonads. J Clin Endocrin Metab 2002;87:4736–4740.
Hannon TS, Noonan K, Steinmetz R, et al. Is McCune-Albright syndrome overlooked in subjects with fibrous dysplasia of bone? J Pediatr 2003;142:532–538.
Candeliere GA, Roughley PJ, Glorieux FH . Polymerase chain reaction based technique for the selective enrichment and analysis of mosaic arg201 mutations in Gsalpha from patients with fibrous dysplasia of bone. Bone 1997;21:201–206.
Turc-Carel C, Limon J, Dal Cin P, et al. Cytogenetic studies of adipose tissue tumours. II. Recurrent reciprocal translocations t(12;16)(q13;p11) in myxoid liposarcomas. Cancer Genet Cytogenet 1986;23:291–299.
Hirabayashi Y, Ishida T, Yoshida MA, et al. Translocation (9;22)(q22;q12). A recurrent chromosome abnormality in extraskeletal myxoid chondrosarcoma. Cancer Genet Cytogenet 1995;81:33–37.
Mezzelani A, Sozzi G, Nessling M, et al. Low grade fibromyxoid sarcoma. A further low-grade soft tissue malignancy characterised by a ring chromosome. Cancer Genet Cytogenet 2000;122:144–148.
Graadt von Roggen JF, Hogendoorn PC, Fletcher CD . Myxoid tumours of soft tissue. Histopathology 1999;35:291–312.
Meis-Kindblom JM, Sjorgren H, Kindblom LG, et al. Cytogenetic and molecular analyses of liposarcoma and its soft tissue stimulators: recognition of new variants and differential diagnosis. Virchows Arch 2001;439:141–151.
Willems SM, Debiec-Rychter M, Szuhai K, et al. Local recurrence of myxofibrosarcoma is associated with increase in tumour grade and cytogenetic aberrations, suggesting a multistep tumour progression model. Mod Pathol 2006;19:407–416.
Acknowledgements
We are grateful to all of the patients for donating their tissue for research and to all of the clinicians and support staff in the London Bone and Soft Tissue Sarcoma Unit who were involved in caring for these patients. The research was generously funded by Skeletal Cancer Action Trust (SCAT), UK: this study was also supported by UCLH/UCL Comprehensive Biomedical Research Centre. BI is funded by the RNOH NHS Trust. UCL is a partner of the EuroBoNeT consortium, a European Commission granted Network of Excellence for studying the pathology and genetics of bone tumours.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Delaney, D., Diss, T., Presneau, N. et al. GNAS1 mutations occur more commonly than previously thought in intramuscular myxoma. Mod Pathol 22, 718–724 (2009). https://doi.org/10.1038/modpathol.2009.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2009.32
Keywords
This article is cited by
-
Osteofibrous dysplasia: a narrative review
Journal of Orthopaedic Surgery and Research (2024)
-
Identification of novel GNAS mutations in intramuscular myxoma using next-generation sequencing with single-molecule tagged molecular inversion probes
Diagnostic Pathology (2019)
-
Mutational analysis of high-grade spindle cell sarcoma of the femur in Mazabraud’s syndrome
Skeletal Radiology (2019)
-
Detection of GNAS mutations in intramuscular / cellular myxomas as diagnostic tool in the classification of myxoid soft tissue tumors
Diagnostic Pathology (2018)
-
The curious case of Gαs gain-of-function in neoplasia
BMC Cancer (2018)