Abstract
Selective progesterone receptor modulators are a class of drugs with progesterone antagonist activity that may confer therapeutic benefit for reproductive disorders in premenopausal women. Endometrial structure, which is dynamically controlled by circulating sex hormones, is likely to be perturbed by progesterone receptor modulators through their progesterone antagonist properties. We examined endometrial histology in 58 premenopausal women treated with the progesterone receptor modulator CDB-4124 (also known as Proellex™) for endometriosis or uterine leiomyomata in two clinical trials. Endometrial biopsies obtained after 3 or 6 months with doses of 12.5, 25, or 50 mg daily oral CDB-4124 were reviewed independently by three pathologists. Consensus diagnoses using the World Health Organization hyperplasia scoring system, comments on specific histologic features, and clinical annotation were collected and analyzed. The majority of the endometrial biopsies (103 of 174 biopsies) contained histologic changes that are not seen during normal menstrual cycles. The histology of CDB-4124-treated patients was generally inactive or atrophic, and less frequently, proliferative or secretory, superimposed upon which were novel changes including formation of cystically dilated glands, and secretory changes coexisting with mitoses and apoptotic bodies. With increasing treatment dose and duration, the cysts became predominant and their lining inactive or atrophic. Cystic glands in the CDB-4124-treated subjects correlated with increased endometrial thickness by ultrasound. None of the CDB-4124-treated patients developed endometrial carcinoma or hyperplasia while on therapy. CDB-4124 therapy for 3–6 months produces histologic changes that are sufficiently novel that they might easily be misinterpreted by pathologists, particularly as disordered proliferative or hyperplastic endometrium. Knowledge of the constellation of endometrial changes associated with this agent and other progesterone receptor modulators, including cystic architecture and mixed non-physiologic epithelial changes will prevent misdiagnosis.
Similar content being viewed by others
Main
Progesterone receptor modulators are a class of drugs that interact with the progesterone receptors to block or modify downstream effects.1 Those with potent progesterone antagonist activity, including asoprisnil,2, 3 mifepristone (RU486),4, 5 and CDB-4124 (17α-acetoxy-21-methoxy-11β-[4-N,N-dimethylaminophenyl]-19-norpregna-4,9-diene-3,20-dione) have great promise as medical therapeutic agents for those gynecologic diseases that are exacerbated by systemic progestins, such as uterine leiomyomata and endometriosis.6, 7 As these are primarily diseases of premenopausal women, patients who are candidates for progesterone receptor modulator medical therapy are likely to be young and have monthly sequential fluctuations of estrogen and progesterone that define their normal menstrual cycle. Clinical trials of progesterone receptor modulators in this population have shown induction of secondary amenorrhea in most subjects, accompanied by persistent or slightly lowered systemic levels of progesterone and estradiol. Assessing the endometrial effects of long-term progesterone antagonism by progesterone receptor modulators in women with persistent estradiol levels is a primary objective of ongoing clinical trials.
The endometrium is a highly dynamic tissue in which proliferation and histologic differentiation are exquisitely sensitive to the local and systemic hormonal environment. The histologic features of the normal menstrual cycle are well established, with mitogenic estrogen effects dominating the follicular phase and progesterone-driven secretory changes in the postovulatory luteal phase.8 Perturbations in the timetable and levels of estrogen and progesterone stimulation are common, and induce such distinctive endometrial changes that many can be recognized by microscopic examination of the endometrium itself.9 For example, disordered proliferation with cyst formation is often identified histologically in association with anovulation as a result of prolonged unopposed estrogen exposure. Delayed ovulation superimposes secretory epithelial differentiation changes upon a disordered gland pattern conferred by the protracted antecedent estrogen exposure. It is the combination of features, many of which otherwise appear individually in other conditions, that provides clues to the underlying hormonal state.
Pathologic evaluation of endometrial samples obtained from long-term progesterone receptor modulator-treated women has largely been confined to the clinical trial environment, as aside from short-term contraceptive use (RU486, mifepristone), these agents are not yet used chronically in the United States. Some consistent trends have emerged. Treatment with asoprisnil10 or mifepristone11 for 2–3 months produces a thickened endometrium with cystically dilated endometrial glands. The appearance of glandular epithelium changes with dose and exposure duration, from inactive to non-physiologic combinations of features usually seen separately in normal proliferative and secretory endometrium. Alterations are not limited to the glands themselves. Thick-walled vessels of the sort often seen in endometrial polyps, but more widely distributed throughout the endometrium, can be seen with asoprisnil therapy.10 Taken together, the histopathologic appearance of progesterone receptor modulator-exposed endometria do not readily fit into established diagnostic categories. This was the backdrop for a 2006 consensus meeting sponsored by the Center for Population Research at the National Institute of Child Health and Human Development where endometrial biopsies from women taking one of four different progesterone receptor modulators were examined by a panel of seven pathologists.7 They proposed the term progesterone receptor modulator-associated endometrial changes (‘PAEC’) to describe the combination of architectural (cysts), non-physiologic epithelial, and vascular findings in the material.12 A shortcoming, however, was that the pathologists were blinded to drug identity and exposure history during and after their review. This prevented comparison between individual agents, and examination of dose and time effects within each.
CDB-4124, a 21-substituted-19-nor-progestin, is a progesterone receptor modulator originally developed at the National Institutes of Health,13 currently under license to Repros Therapeutics Inc. (The Woodlands, TX, USA), which is now in phase II clinical trials for the treatment of endometriosis and uterine leiomyomata in premenopausal women. Preliminary data suggest a favorable clinical response of the underlying disease with 3–6 months of CDB-4124 therapy, and studies on the safety of this agent have included biopsies of the endometrium at various intervals to ensure that hyperplasia or carcinoma does not occur at increased frequency. Here, we present the histologic changes in the endometrium consequent to the use of this progesterone receptor modulator for 3–6 months, with the goal of helping pathologists to avoid misinterpretation of novel changes.
Materials and methods
Patient Groups
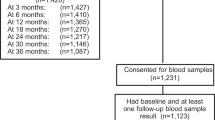
Premenopausal women with a diagnosis of endometriosis (Trial ZPE-002, 6 months of therapy, n=29) or uterine leiomyomas (Trial ZPU-003, 3 months of therapy, n=38) were administered oral CDB-4124 (also known as Proellex™; Progenta™; Repros Therapeutics Inc.) therapy at a daily dose of 12.5, 25, or 50 mg for a period of 77–175 days. Baseline pretreatment and on-treatment surveillance biopsies were performed and routine histologic sections were prepared for histologic review by a panel of three pathologists (OBI, RJZ, and GLM). Patients whose on-treatment biopsies did not contain sufficient endometrial tissue for interpretation (inadequate, n=3) or subjects who missed their on-treatment biopsies (missing, n=6) were excluded, leaving a total of 58 patients (27 with endometriosis and 31 with leiomyomas) for interpretation of endometrial histology while exposed to various doses of CDB-4124 (12.5 mg, n=23; 25 mg, n=26; and 50 mg, n=9). In total, 51 patients had technically adequate corresponding baseline, or pretreatment, biopsies.
All patients were specifically consented for inclusion in this phase II clinical trial, which was performed by Repros Therapeutics Inc. under investigational new drug application number IND-70 535 filed with the United States Food and Drug Administration.
Pathology Review
Three pathologists independently reviewed the baseline and on-treatment endometrial biopsies blinded to treatment group and time of exposure. A structured reporting form (Supplementary Table 1) was completed by each pathologist for each endometrial biopsy specimen, using endometrial hyperplasia and carcinoma diagnostic criteria of the World Health Organization.14 Diagnoses were assigned as follows. Each histologically adequate biopsy was assigned to the most severe observed diagnostic pattern of seven primary diagnostic categories, listed here in sequence of increasing severity: (1) benign, (2) simple non-atypical endometrial hyperplasia, (3) complex non-atypical endometrial hyperplasia, (4) simple atypical endometrial hyperplasia, (5) complex atypical endometrial hyperplasia, (6) endometrioid-type endometrial adenocarcinoma, or (7) other malignant neoplasm. In each case, the pathologists also noted whether an endometrial polyp was present or absent. Subclassification within the primary diagnostic categories, and supplemental histologic observations were recorded for each diagnostic pass (one review by one pathologist=‘diagnostic pass’). Some of the categories of supplemental observations were created based on descriptions of changes seen with other progesterone receptor modulators.12 Final primary diagnosis was determined by majority opinion of the three reviewing pathologists, or in cases where they all disagreed, by the single most severe diagnosis of the three. A polyp was determined to be present if two or more of the three pathologists made that determination.
After compilation of all data, the pathologists met to discuss their observations, including novel observations for which the diagnostic or observation categories were inadequate. The pathologists were unblinded following primary data collection and a preliminary descriptive analysis was performed to target specific features and case subsets for re-review. The purpose was to generate more precise descriptive details in support of the blinded interpretations previously rendered. Randomly selected examples of each CDB-4124 dose group, and groups of cases identified by particular blinded comments (such as ‘unusual vascular pattern’) were re-reviewed to assist in generating cohesive descriptions of findings.
Endometrial Thickness Measurement
Transvaginal ultrasound endometrial thickness measurements (endometrial stripe, consisting of a bilayer of anterior and posterior endometrium) were performed by ultrasound estimation of endometrial stripe width. All endometrial thickness measurements were taken within 1 day of accompanying endometrial biopsy.
Serum Hormone Levels
Peripheral blood was drawn at the time of endometrial biopsy, and analyzed for estradiol and progesterone concentrations.
Data Analysis
All data were exported to a spreadsheet, then analyzed, and plotted using Systat v.12.0 (Systat Software Inc., San Jose, CA, USA). Significance of CDB-4124 treatment changes compared with baseline (treatment effect=combined baseline vs combined treatment groups) was calculated using Fishers exact and t-tests, respectively, for categorical and numerical data. Significance of effect among different CDB-4124 doses (dose effect=CDB-4124 12.5 vs 25 vs 50 mg) was calculated using Pearson's χ2 and ANOVA tests, respectively, for categorical and numerical data.
All descriptive observations were tallied by case and treatment group, without application of a consensus algorithm. As three diagnostic passes were made for each case, the number of possible observations is three times the number of cases.
Results
Patient Characteristics
Demographics, endocrine status, and endometrial thickness measurements are shown in Table 1 by CDB-4124 dosage treatment group. The average age of the 58 patients was 36.9 years, and was not significantly different between treatment groups (ANOVA, P=0.064). Indications for CDB-4124 treatment, which included endometriosis (47%) and uterine leiomyomas (53%), were unevenly distributed across all CDB-4124 dosages, with the highest CDB-4124 dose group of 50 mg daily solely represented by endometriosis patients. The treatment interval was bimodal with peaks of about 80 and 170 days with a range from 77 to 175 days overall, with longest exposures in the 50 mg group. Significant associations of CDB-4124 dose groups with the duration of therapy (ANOVA, P=0.003) and underlying diagnosis (χ2 P=0.002) made it difficult to study those factors across all CDB-4124 doses administered.
CDB-4124 administration at all doses caused some degree of ovulation suppression, as documented by serum estradiol and progesterone level declines during CDB-4124 therapy compared with pretreatment baseline (t-test, P=0.004 and 0.002, respectively). Patients were generally amenorrheic on therapy (data not shown), but full clinical data regarding menstrual patterns and relief of symptoms referable to underlying disease will be reported elsewhere. Estradiol and progesterone levels were not significantly different among the three dose groups (ANOVA, P=0.645 and 0.722, respectively) at the small sample sizes from this study.
Endometrial thickness, which averaged 9.8 mm at intake, increased significantly (t-test, P=0.007) to a mean of 14.9 mm during CDB-4124 therapy. The extent of endometrial thickening was not significantly different by dose group (ANOVA P=0.913).
Blinded Observations
All baseline and all CDB-4124-treated endometrial biopsies had benign (non-hyperplastic and non-malignant) histologic findings by majority diagnosis of the three reviewing pathologists. There was no significant relationship (P=0.346) between endometrial polyps and CDB-4124 therapy, with no polyps present at baseline, and only one during therapy.
More detailed information regarding the histologic appearance of CDB-4124-treated endometrium was collected during pathologic review as observations of specific features indicated by a checklist. All secondary diagnoses and supplemental observations by all pathologists were carried forward into Tables 2 and 3, where they are shown as number of observations per pathologist diagnostic ‘pass’. As three pathologists reviewed each case, one case appears as three diagnostic passes. As it was permitted to make more than one supplemental observation (Table 3), these add up to more than 100%.
Substratification of benign endometria by secondary diagnosis showed significant changes with CDB-4124 administration (secondary diagnosis; Table 2). Pretreatment biopsies were primarily secretory (76%), but this shifted to inactive (55%) or disordered proliferative (18%) upon CDB-4124 administration. Diagnoses indicating mitotic activity in the glands (proliferative and disordered proliferative) were common at 12.5 and 25 mg daily CDB-4124, but absent entirely in the 50-mg dose group, suggesting an antimitotic effect at higher doses. Abnormal types of secretory endometrium, either regionally dyssynchronous or with admixed mitoses, were rare and seen in equivalent frequencies in both baseline and CDB-4124-treated endometria (Table 3). When present, secretory differentiation included development of stratified and non-stratified cytoplasmic vacuoles of variable size and location.
Cystically dilated glands were seen in 59% of CDB-4124-treated biopsies, and this correlated with increased endometrial thickness as measured by ultrasound (Figure 1). The 12.5-mg CDB-4124 treatment group was the largest studied, and because it included patients biopsied at either 3 or 6 months, was suited to examination of a possible treatment duration effect. Figure 2 shows that endometrial thickening and generation of cysts was found to be a time-dependent phenomenon at the fixed CDB-4124 daily dose of 12.5 mg. Increased endometrial volume seen by ultrasound was most likely due to expansion of gland lumen diameters.
Presence of histologic endometrial cysts correlates with endometrial thickness by ultrasound. When the majority (two or more of three) of pathologists identified cysts, the endometrial thickness was significantly greater than when none or only one saw cysts (P<0.001; Wilcoxon rank sum). Each round symbol plots endometrial thickness (y axis, mm) for a specimen in which the majority of pathologists did (x axis=yes) or did not (x axis=no) make a supplemental observation of cysts. CDB-4124 exposed endometria only, pretreatment biopsies were excluded. Summary notched box plot with superimposed dot density plot of individual (round symbols) cases. Box contains inner quartiles, notched at the median and tapered to the upper and lower confidence intervals. Whiskers show the data range, excluding outliers.
Duration of 12.5 mg daily CDB-4124 exposure is associated with endometrial thickness and cyst formation. Women taking 12.5 mg daily CDB-4124 showed a trend toward increasing endometrial thickness with duration of therapy (a), and those endometria judged by a majority of pathologists to contain cysts had a significantly longer exposure (b, pretreatment biopsies excluded; P<0.001; Wilcoxon rank sum).
Unusual vascular patterns were more common in CDB-4124-treated endometria (4%) than baseline (1%), but this difference was not significant (0.081).
Unblinded Review of Histologic Changes in CDB-4124 Treatment Groups
After unblinding, a selection of CDB-4124-treated endometria was reviewed to better characterize the histologic changes that were not adequately captured by the review forms, to select representative cases for photography, and to generate complete descriptions of the resultant pathology. There was a spectrum of changes within the material, which included many patterns and combinations of features that are rarely, if ever, seen under normal circumstances. The pattern of a disordered arrangement of irregularly distributed cystically dilated glands with mitotically active secretory epithelium transformed at higher doses into a more uniform population of atrophic cysts separated by only sparse amounts of stroma. Figure 3 shows typical changes in the 12.5-mg treatment group, including cystically dilated glands with moderately abundant intervening compact stroma and vacuole-bearing secretory endometrium with admixed mitotic figures. Longer exposure with a higher CDB-4124 dose of 25 mg daily (Figure 4) yielded more prominent cysts that occupied a large proportion of the endometrial volume at the expense of intervening stroma. Mitoses were less common.
Progesterone receptor modulator-associated endometrial changes (‘PAEC’) after 92 days of 12.5 mg daily CDB-4124. Dyssynchronous growth of glands compared with stroma results in scattered cyst formation throughout the endometrial compartment (a). Non-physiologic epithelial changes are characterized by admixture of secretory vacuoles with mitoses (b), or mitoses with apoptotic bodies (c). A similar constellation of effects has been described for other progesterone receptor modulators.
Progesterone receptor modulator-associated endometrial changes (‘PAEC’) after 154 days of 25 mg daily CDB-4124. At higher CDB-4124 doses, or longer periods of exposure, cyst formation becomes extensive with depletion of intervening stroma to form thin cyst walls (a). In this example, non-physiologic combinations of epithelial secretory vacuoles (b) and apoptotic change (c) are seen.
Apoptotic cell death, as indicated by apoptotic bodies within endometrial glands, was not assessed formally during the blinded phase of review, but were noted in free text comments made by the pathologists. As part of the unblinded review, we looked for apoptotic bodies across the different treatment groups, in conjunction with other features previously noted. Cases with readily identifiable apoptotic bodies were those with a mitotically active epithelium.
The character of vascular change was elaborated upon by re-review of those five patients in whom one or more pathologists noted this finding. Three of these had dilated ectatic vessels devoid of thrombosis, which were located within otherwise intact tissue fragments (Figure 5a). Two cases had isolated occlusive venous thrombi within tissue fragments that demonstrated sheet-like necrosis (Figure 5b). Arteriolar thrombosis with aggregative stromal breakdown was not seen.
Ectatic and thrombosed vessels in CDB-4124-treated patients. The most common vascular change in CDB-4124-treated patients is ectasia (a), in which dilated thin-walled blood vessels have a prominent endothelial lining and open lumen. Less frequent is vascular thrombosis (b) associated with sheet-like necrosis of large areas of endometrial tissue, a pattern seen when venous structures are occluded.
Discussion
CDB-4124 administration induces a constellation of histopathologic features encompassed within the spectrum of PAEC previously described for mifepristone, CDB-2914 (HRA Pharma, France); JNJ-17072341 (Johnson and Johnson Pharmaceutical Research and Development, LLC, Raritan, NJ, USA) and asoprisnil.12 PAEC changes of cysts and combinations of glandular epithelial alterations that are usually ascribed to the mutually exclusive effects of estrogens (mitotic activity) and progestins (secretory change) were commonly noted in CDB-4124-treated endometria. Even when glandular secretory differentiation was present, the stroma rarely demonstrated predecidual changes. This epithelial–stromal dyssynchrony has also been recognized as a feature of PAEC. Admixed secretory changes and mitoses are not unique to CDB-4124-exposed patients, being transiently present in the normal menstrual cycle soon after ovulation (cycle days 16 and 17, corresponding to postovulatory days 2–3). Unlike the normal state, dyssynchronous changes in CDB-4124-treated women are more variable across the endometrial field, can persist for months, and are usually superimposed upon an abnormal architecture characterized by cysts. It is the combination of features that are peculiar to progesterone receptor modulator-exposed patients, rather than particular uniqueness of any specific element. These non-physiologic epithelial effects were not seen in all patients receiving CDB-4124, with over half having inactive endometrial glands devoid of either mitoses or secretory vacuoles. Thus, it is possible in only a fraction of treated women to claim that endometrial changes of CDB-4124 are sufficiently pathognomic to offset them from other elements in the differential diagnosis such as cystic atrophy, or delayed ovulation.
Cystic dilation of endometrial glands is a histologic correlate of ultrasound-documented endometrial thickening in CDB-4124-treated women. It is a dynamic process that occurs increasingly with higher doses and longer exposures. In its most extreme form, cyst lumen volume exceeds that of the cellular components of endometrial tissue, which persists predominantly as delicate cyst walls lined by atrophic epithelium. Superficially, these resemble senile-type endometrial polyps, but are widely diffuse rather than localized. Gradual overgrowth of non-shedding endometrium may also contribute to increased thickness.
Endometrial thickness in progesterone receptor modulator-treated women may provide a surrogate marker for development of endometrial cysts, but it is difficult at this time to state whether it is a useful screen for development of hyperplasia or carcinoma in this premenopausal population.15 This is because many women with endometrial hyperplasias have an endometrial thickness within the normal range of premenopausal endometrium, which averages from 9 to 12 mm.
Epithelial mitotic activity, which was seen predominantly at 12.5 and 25 mg CDB-4124 doses disappeared almost entirely at 50 mg. A similar dose effect has been seen with other progesterone receptor modulators, but it is unknown whether it is mediated through the progesterone receptor itself or invocation of another pathway.16, 17, 18, 19 Most mitotically active CDB-4124-treated endometria also had an increase in epithelial apoptotic bodies. The proliferative effect is thus, in part, counterbalanced by an increase in cell death. More sophisticated quantitative studies will be required to determine whether the net effect of these opposing factors is one of tissue growth or involution.
A low frequency (4%) of vascular alterations, primarily thin-walled vascular ectasia, was seen in CDB-4124-treated endometria (marginally significant, P=0.071). This is nonspecific, having also occurred in one baseline endometrium, and women treated with non-progesterone receptor modulator exogenous progestin-containing treatment regimens.20, 21, 22 Notably lacking were occlusive microarterial thrombi of the type encountered with unopposed estrogens, high-density ‘chicken-wire’ microvessels seen with mifepristone,23 and widespread vascular wall thickening reported previously for asoprisnil.10 Two cases with endometrial vascular thrombosis involved only venules in isolated fragments that had sheet-like necrosis. It is unclear whether this was an effect of an underlying fibroid or other localized disease, or CDB-4124 therapy.
The hormonal context upon which premenopausal administration of progesterone receptor modulators is superimposed is likely to be a codeterminant of endometrial histology. We do not know at this time how generalizable our current findings in premenopausal women might be to the postmenopausal patient. In general, both estradiol and progesterone levels declined with CDB-4124 administration, indicating some level of ovarian suppression. The endocrine profile of women treated in the current study will be the subject of a separate report.
Demonstration of endometrial safety is an essential prerequisite for public use of any new pharmacological compound with sex steroid hormone activity.2, 24 The endometrium is of particular interest from the perspective of agents designed to block progesterone effects, because of the known anticarcinogenic effects of progestins in an estrogen-rich environment.25 The short term of this study did not permit direct observation of long-term outcomes, and it is not yet clear how these results may, or may not, be generalizable to other administration doses and schedules. A particular difficulty is that the biologic effects of synthetic compounds such as CDB-4124 cannot be modeled as a pure effect (antagonist) upon a single target (progesterone receptor). Indeed, the antiproliferative endometrial effects of increasing progesterone receptor modulator dosage, as has now been described for several progesterone receptor modulators,19 cannot be explained by such simple mechanisms.
In conclusion, short-term CDB-4124 treatment of premenopausal women creates a disorganized endometrial gland architecture of admixed cystic and tubular glands with non-physiologic combinations of secretory and proliferative features. With increasing dose and time of exposure, the epithelium becomes increasingly atrophic and cysts more regularly prominent. No endometrial cancers or hyperplastic lesions were seen in this study, and at this time there is no specific indication of a heightened endometrial cancer risk. Progesterone receptor modulator-treated endometria do, however, present several unique challenges. When practicing pathologists encounter unfamiliar histopathologic findings that do not readily fit into an existing diagnostic lexicon they may be tempted to render best fit diagnoses without meeting all requisite diagnostic criteria. Crowded cysts might be interpreted as ‘hyperplasia,’ abnormal vessels as ‘polyps,’ and non-physiologic epithelium as a ‘dyssynchronous cycle.’ This can be remedied by developing new diagnostic criteria and terminology. The problem is not simply one of semantics and criteria, however, as the behavior over time of any newly defined entity must be empirically determined. This has not yet been done for CDB-4124. One question is whether the endometrial changes are reversible upon withdrawal of the compound, and if so whether that might justify an interrupted rather than continuous regimen.
References
Attardi BJ, Burgenson J, Hild SA, et al. In vitro antiprogestational/antiglucocorticoid activity and progestin and glucocorticoid receptor binding of the putative metabolites and synthetic derivatives of CDB-2914, CDB-4124, and mifepristone. J Steroid Biochem Mol Biol 2004;88:277–288.
Chwalisz K, Larsen L, Mattia-Goldberg C, et al. A randomized, controlled trial of asoprisnil, a novel selective progesterone receptor modulator, in women with uterine leiomyomata. Fertil Steril 2007;87:1399–1412.
Demanno D, Elger W, Garg R, et al. Asoprisnil (J867): a selective progesterone receptor modulator for gynecological therapy. Steroids 2003;68:1019–1032.
Fiscella K, Eisinger SH, Meldrum S, et al. Effect of mifepristone for symptomatic leiomyomata on quality of life and uterine size: a randomized controlled trial. Obstet Gynecol 2006;108:1381–1387.
Steinauer J, Pritts EA, Jackson R, et al. Systematic review of mifepristone for the treatment of uterine leiomyomata. Obstet Gynecol 2004;103:1331–1336.
Chabbert-Buffet N, Meduri G, Bouchard P, et al. Selective progesterone receptor modulators and progesterone antagonists: mechanisms of action and clinical applications. Hum Reprod Update 2005;11:293–307.
Horne FM, Blithe D . Progesterone receptor modulators and the endometrium: changes and consequences. Hum Reprod Update 2007;13:567–580.
Noyes RW, Hertig AT, Rock J . Dating the endometrial biopsy. Am J Obstet Gynecol 1975;122:262–263.
Mutter GL, Zaino RJ, Baak JPA, et al. The benign endometrial hyperplasia sequence and endometrial intraepithelial neoplasia. Int J Gynecol Pathol 2007;26:103–114.
Williams AR, Critchley HO, Osei J, et al. The effects of the selective progesterone receptor modulator asoprisnil on the morphology of uterine tissues after 3 months treatment in patients with symptomatic uterine leiomyomata. Hum Reprod 2007;22:1696–1704.
Baird DT, Brown A, Critchley HO, et al. Effect of long-term treatment with low-dose mifepristone on the endometrium. Hum Reprod 2003;18:61–68.
Mutter GL, Bergeron C, Deligdisch L, et al. The spectrum of endometrial pathology induced by progesterone receptor modulators. Mod Path 2008;21:591–598.
Attardi BJ, Burgenson J, Hild SA, et al. CDB-4124 and its putative monodemethylated metabolite, CDB-4453, are potent antiprogestins with reduced antiglucocorticoid activity: in vitro comparison to mifepristone and CDB-2914. Mol Cell Endocrinol 2002;188:111–123.
Silverberg SG, Mutter GL, Kurman RJ, et al. Tumors of the uterine corpus: epithelial tumors and related lesions In: Tavassoli FA, Stratton MR (eds). WHO Classification of Tumors: Pathology and Genetics of Tumors of the Breast and Female Genital Organs 1st edn IARC Press: Lyon, France, 2003, pp 221–232.
Dueholm M, Lundorf E, Olesen F . Imaging techniques for evaluation of the uterine cavity and endometrium in premenopausal patients before minimally invasive surgery. Obstet Gynecol Surv 2002;57:388–403.
Brenner RM, Slayden OD, Nayak NR, et al. A role for the androgen receptor in the endometrial antiproliferative effects of progesterone antagonists. Steroids 2003;68:1033–1039.
Narvekar N, Cameron S, Critchley HO, et al. Low-dose mifepristone inhibits endometrial proliferation and up-regulates androgen receptor. J Clin Endocrinol Metab 2004;89:2491–2497.
Slayden OD, Nayak NR, Burton KA, et al. Progesterone antagonists increase androgen receptor expression in the rhesus macaque and human endometrium. J Clin Endocrinol Metab 2001;86:2668–2679.
Chwalisz K, Brenner RM, Fuhrmann UU, et al. Antiproliferative effects of progesterone antagonists and progesterone receptor modulators on the endometrium. Steroids 2000;65:741–751.
Hickey M, Krikun G, Kodaman P, et al. Long-term progestin-only contraceptives result in reduced endometrial blood flow and oxidative stress. J Clin Endocrinol Metab 2006;91:3633–3638.
McGavigan CJ, Dockery P, Metaxa-Mariatou V, et al. Hormonally mediated disturbance of angiogenesis in the human endometrium after exposure to intrauterine levonorgestrel. Hum Reprod 2003;18:77–84.
Simbar M, Manconi F, Markham R, et al. A three-dimensional study of endometrial microvessels in women using the contraceptive subdermal levonorgestrel implant system, norplant. Micron 2004;35:589–595.
Narvekar N, Critchley HO, Cheng L, et al. Mifepristone-induced amenorrhoea is associated with an increase in microvessel density and glucocorticoid receptor and a decrease in stromal vascular endothelial growth factor. Hum Reprod 2006;21:2312–2318.
Eisinger SH, Bonfiglio T, Fiscella K, et al. Twelve-month safety and efficacy of low-dose mifepristone for uterine myomas. J Minim Invasive Gynecol 2005;12:227–233.
Writing Group for the PEPI Trial. Effects of hormone replacement therapy on endometrial histology in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. JAMA 1996;275:370–375.
Acknowledgements
We thank Dr Andre VanAs and Dr Ronald Wiehle of Repros Therapeutics Inc. for making the clinical trial data available for analysis.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
The authors received compensation from Repros Therapeutics Inc. for planning the pathology evaluation and blinded review of histological materials, but were not paid for the production of this paper and had full and independent control over all analysis and interpretation of the data. The study was funded by Repros Therapeutics Inc.
Supplementary Information accompanies the paper on Modern Pathology website (http://www.nature.com/modpathol)
Supplementary information
Rights and permissions
About this article
Cite this article
Ioffe, O., Zaino, R. & Mutter, G. Endometrial changes from short-term therapy with CDB-4124, a selective progesterone receptor modulator. Mod Pathol 22, 450–459 (2009). https://doi.org/10.1038/modpathol.2008.204
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2008.204
Keywords
This article is cited by
-
Hepatotoxizität selektiver Progesteronrezeptormodulatoren
Gynäkologische Endokrinologie (2021)
-
Leiomyoma: genetics, assisted reproduction, pregnancy and therapeutic advances
Journal of Assisted Reproduction and Genetics (2012)