Abstract
Enterochromaffin (EC) cells in the gastrointestinal (GI) mucosa are the main source of serotonin (5-hydroxytryptamine (5-HT)) in the body. 5-HT is implicated in the pathophysiology of many GI disorders including functional and inflammatory bowel disorders. Herein we studied the role of interleukin 13 (IL-13) in EC cell biology by utilizing IL-13-deficient (IL-13−/−) mice and BON cells (a model for human EC cells). The numbers of EC cells and 5-HT amount were significantly lower in enteric parasite, Trichuris muris–infected IL-13−/− mice compared with the wild-type mice. This was accompanied with increased parasite burden in IL-13−/− mice. Treatment of naive and infected IL-13−/− mice with IL-13 increased EC cell numbers and 5-HT amount. BON cells expressed IL-13 receptor and in response to IL-13 produced more 5-HT. These results provide novel information on IL-13-mediated immunological control of 5-HT in the gut, which may ultimately lead to improved therapeutic opportunities in various GI disorders.
Similar content being viewed by others
Introduction
The gastrointestinal (GI) tract is the largest endocrine organ in the human body, producing a wide variety of biologically active products. Many of the enteric endocrine cells reside within the epithelial cells of intestinal mucosa where stimuli from the lumen or surrounding cells can influence their cellular biology.1 The best-characterized subset of enteric endocrine cells are enterochromaffin (EC) cells, which synthesize and release serotonin (5-hydroxytryptamine (5-HT)) and are the main source of 5-HT in the GI tract.2, 3 5-HT is an important enteric mucosal signaling molecule that can influence the maintenance of intestinal homeostasis, specifically motor and secretory functions.4, 5, 6 The release of 5-HT increases motility of the gut and is also an extremely important mediator of nausea and satiety.7, 8 Abnormal regulation of 5-HT in the human gut has been implicated with a diverse array of GI disorders such as inflammatory bowel disease,9, 10 irritable bowel syndrome (IBS),9, 11, 12 celiac disease,13 colorectal cancer,14, 15 diverticular disease,16 and enteric bacterial, viral, and parasitic infection.17, 18, 19, 20, 21, 22 Recently, we have demonstrated a critical role of 5-HT in the activation of immune response and generation of mucosal inflammation in experimental model of colitis.23, 24 Although 5-HT and EC cell biology have been implicated in a plethora of GI disorders, the precise mechanism regulating the observed changes in 5-HT content and EC cell numbers during GI disorder remains unclear.
Considering the location of EC cells in the epithelial layer of the gut mucosa, it is very likely that immune cells play an important role in EC cell biology in the context of various GI disorders. In patients with postinfectious IBS, observation of immune activation (increased number of CD3+ T cells) has been associated with increased EC cell numbers, which is suggestive of a link between these two systems.25, 26 This association between the immune system and endocrine system of the GI tract also holds true in animal models of postinfectious IBS.20, 27 The notion of an immune–endocrine axis in the GI tract is further supported by the findings that EC cells in mucosa of the ileum and colon of rhesus monkeys are in direct or close contact with lymphocytes.28 Two recent studies from our laboratory have uncovered a pivotal role for the immune system in EC cell biology.21, 22 Using the nematode Trichuris muris model of intestinal infection, we have observed upregulation in the number of EC cells and 5-HT amount following infection.21 This infection-induced increase in EC cells or in 5-HT was not evident in severe combined immunodeficient (SCID) mice. EC cell numbers and 5-HT amount significantly increased following reconstitution of SCID mice with CD4+ T cells from infected mice and this was accompanied by an upregulation of colonic CD3+ T cells and T helper type 2 (Th2) cytokines. In addition, laser capture microdissection-based molecular and immunofluorescence techniques revealed the presence of the interleukin-13 receptor α1 (IL-13Rα1) on EC cell.21 These findings demonstrate an important role for CD4+ T cells in EC cell function in enteric infection-induced gut inflammation. Recently, we have also demonstrated a difference in EC cell and 5-HT responses in Th1 and Th2 environments.22 Higher amount of 5-HT and EC cell numbers were observed in mice that are resistant to infection and expel worms by generating a Th2-type immune response as compared with susceptible mice that developed chronic infection with the generation of a Th1 response. Utilizing Stat4- and Stat6-deficient mice, which are impaired in Th1 and Th2 response respectively, we have also shown impairment in the development of infection-induced EC cell hyperplasia and in 5-HT production in Stat6-deficient mice after T. muris infection.22 These findings suggest the importance of the immunological profile of the inflammatory response in the regulation of EC cell biology in gut mucosa.
The involvement of immune response in the regulation of EC cell hyperplasia and 5-HT production in T. muris infection as well as the presence of IL-13Rα1 in colonic 5-HT-expressing EC cells exemplifies the role of IL-13 in EC cell biology. In this study we solidify the role of IL-13 in EC cell biology utilizing IL-13-deficient (IL-13−/−) mice in T. muris infection model and a cell culture model for EC cells (BON cells). Our results demonstrate compelling evidence in favor of a role of IL-13 in EC cell biology at the molecular level in both an in vivo mouse model and in culture human model of EC cells.
Results
IL-13 deficiency inhibits worm expulsion and development of infection-induced EC cell hyperplasia and 5-HT production in T. muris infection
BALB/c (wild-type) mice are resistant to T. muris infection and can expel almost all the worms within 21 days after infection, whereas IL-13−/− mice on BALB/c background failed to clear the parasitic infection (Figure 1a). The clearance of parasite from wild-type mice was associated with significantly higher levels of IL-13 (Figure 1b) and IL-4 (Figure 1c) in the colon, which is in agreement with previous observations of T. muris–infected BALB/c mice.21 IL-13 levels were elevated on both days 14 and 21 after infection in wild-type mice and, as expected, were not detectable in IL-13−/− mice. IL-4 levels were increased in the colonic tissues of both the wild-type and IL-13−/− mice in comparison with their noninfected controls. Notably, IL-4 levels were significantly higher in the IL-13−/− mice compared with their wild-type counterparts on days 14 and day 21 after infection.
Inhibition of worm expulsion in interleukin-13-deficient (IL-13−/−) mice as compared with the wild-type (WT) BALB/c mice. Both IL-13−/− and WT mice were infected orally with 300 eggs of Trichuris muris and killed on days 14 and 21 post infection (PI). (a) Worm burden in infected IL-13−/− and WT mice on days 14 and 21 PI. (b) Colon tissue IL-13 levels in WT mice infected with T. muris on days 14 and 21 PI. (c) Colon IL-4 levels in both noninfected and infected IL-13−/− and WT mice on days 14 and 21 PI. Each bar represents mean±s.e.m. of 3–7 mice. *P<0.05; **P<0.01; ***P<0.001.
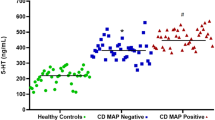
Significantly lower number of EC cells and 5-HT amount was detected in the colon of IL-13−/− mice in comparison with wild-type mice after infection. We found that noninfected wild-type controls had significantly higher number of 5-HT-expressing EC cells compared with IL-13−/− controls and, following infection, a progressive increase in 5-HT-expressing EC cells was observed in the wild-type group on both days 14 and 21 (Figure 2a). This increase in 5-HT-expressing EC cell numbers was statistically significant on day 21 when the wild-type infected group was compared with its noninfected counterpart. However, minimal changes in 5-HT-expressing EC cell numbers were observed in IL-13−/− mice irrespective of the duration of infection (Figure 2a). We have previously established parallels between the number of EC cells and the ability of the mouse to expel the parasite as measured by worm burden.21 This study also found a similar relationship between worm burden and EC cell numbers (Figure 1a vs. Figure 2a). Significantly fewer 5-HT-expressing EC cells were found in IL-13−/− mice along with increased worm burden. Restoration of IL-13, by treatment with recombinant mouse IL-13 (rmIL-13) for 5 days, in naive IL-13−/− mice significantly increased both EC cell numbers and 5-HT content in the colon of IL-13−/− mice (Figure 3a,b). In addition to that, replenishment of IL-13 in naive IL-13−/− mice resulted in upregulation of TPH1 (tryptophan hydroxylase 1) protein, the rate-limiting enzyme involved in the biosynthesis of 5-HT by EC cells (Figure 3c). Upregulation of EC cell number and 5-HT amount was observed in infected IL-13−/− mice treated with rmIL-13 (Figure 4a,b). Restoration of IL-13 levels improved the ability of IL-13−/− animals to expel the parasite, as indicated by worm burden (number of worms found was 176±43.2 and 100.5±27.1 in IL-13−/− mice that received vehicle and rmIL-13, respectively). Interestingly, although there was a significantly increased production of IL-4 in the IL-13−/− mice compared with wild-type mice after infection, the number of EC cells remained unchanged (Figure 1b vs. Figure 1a). These observations provide evidence in favor of a key role of IL-13 in the regulation of EC cell biology and 5-HT production in enteric infection caused by T. muris.
Interleukin-13-deficient (IL-13−/−) mice infected with Trichuris muris exhibited significantly less enterochromaffin (EC) cell numbers in comparison with the wild-type (WT) mice. Both IL-13−/− and WT mice were infected orally with 300 eggs of T. muris and killed on days 14 and day 21 post infection (PI). (a) Number of EC cells in the colon of noninfected and infected mice on days 14 and 21 PI. (b) Amount of colonic 5-hydroxytryptamine (5-HT) in noninfected and infected mice on day 14 PI. (c) Representative micrograph showing 5-HT-expressing EC cells in the colon of infected WT mice on day 14 PI. (d) Representative micrograph showing 5-HT-expressing EC cells in the colon of infected IL-13−/− mice on day 14 PI. Each bar represents mean±s.e.m. of 3–7 mice and micrographs at original magnification × 200. αNot statistically significant. *P<0.05; **P<0.01.
Treatment of naive interleukin-13-deficient (IL-13−/−) mice with recombinant mouse IL-13 (rmIL-13) upregulated the number of enterochromaffin (EC) cells and the amount of 5-hydroxytryptamine (5-HT) found in the colon as well as total tryptophan hydroxylase 1 (TPH1) protein. IL-13−/− mice were given 2 μg of rmIL-13 for 5 consecutive days, and the control group received the vehicle (phosphate-buffered saline (PBS)) by intraperitoneal (IP) injection. (a) Number of EC cells in the colon of IL-13−/− mice injected with vehicle or rmIL-13. (b) Amount of colonic 5-HT in the colon of IL-13 knockout mice injected with vehicle or rmIL-13. (c) Representative western blot and relative band density of TPH1 protein expression in the colon of IL-13−/− mice injected with vehicle or rmIL-13. (d) Representative micrograph showing 5-HT-expressing EC cells in the colon of IL-13−/− mice that received PBS by IP injection. (e) Representative micrograph showing 5-HT-expressing EC cells in the colon of IL-13−/− mice that received rmIL-13. Each bar represents mean±s.e.m. of 4 mice and micrographs at original magnification × 200. *P<0.05; **P<0.01.
Treatment of Trichuris muris–infected interleukin-13-deficient (IL-13−/−) mice with recombinant mouse IL-13 (rmIL-13) increases enterochromaffin (EC) cell number and the amount of 5-hydroxytryptamine (5-HT) found in the colon on day 14 post infection (PI). IL-13−/− mice were given 2 μg of rmIL-13 for 15 days, and the control group received phosphate-buffered saline (PBS) as vehicle via intraperitoneal (IP) injection. (a) Number of EC cells in the colon of infected IL-13−/− mice injected with vehicle or rmIL-13. (b) Amount of colonic 5-HT in the colon of IL-13 knockout mice injected with vehicle or rmIL-13. (c) Representative micrograph showing 5-HT-expressing EC cells in the colon of infected IL-13−/− mice that received PBS by IP injection. (d) Representative micrograph showing 5-HT-expressing EC cells in the colon of infected IL-13−/− mice that received rmIL-13. Each bar represents mean±s.e.m. of 3–5 mice and micrographs at original magnification × 200. *P<0.05; **P<0.01.
IL-13 upregulates 5-HT concentration in both the cell and media of BON cells
Previously, we have shown that 5-HT-expressing EC cells in the mouse colon express IL-13Rα1.22 In this study we observed that IL-13 plays an important role in promoting EC hyperplasia and 5-HT production. In examining the molecular mechanisms associated with IL-13 and EC cell function, we began by describing the expression of IL-13Rα1 in BON cells (Figure 5). BON cells are a human carcinoid cell line derived from a metastasis of a pancreatic carcinoid tumor of EC cell origin.29 IL-13Rα1 mRNA is expressed in BON cells (Figure 5a); in addition, IL-13Rα1 protein was also identified in BON cells using immunocytofluorescence. Treatment of BON cells with recombinant human IL-13 (rhIL-13) resulted in significantly increased intracellular and extracellular 5-HT after 24 h (Figure 6). However, IL-13 does not induce the immediate release (after 1 h) of 5-HT from BON cells (Figure 7), in comparison with phorbol-12-myristate-13-acetate, a secretagogue known to induce the secretion of hormones from BON cells.30
BON cells (a model for human enterochromaffin (EC) cells) express interleukin-13 receptor α1 (IL-13Rα1). (a) Agarose gel electrophoresis of the PCR product from reverse transcriptase-PCR of IL-13Rα1 mRNA. Samples were from a negative control (H2O), lymphocyte cell population (positive control), and BON cell population. (b–g) Immunocytofluorescence of BON cells using both anti-IL-13Rα1 and mouse isotype control. (b) Overlay of BON cells stained with 4′,6-diamidino-2-phenylindole (DAPI) and (c) IL-13Rα1 (1°: mouse anti-IL-13Rα1 dilution 1:100; 2°: Alexa Fluor 568 F(ab′)2 fragment goat anti-mouse IgG dilution 1:500). (e) Overlay of BON cells stained with DAPI and (f) mouse IgG isotype control (1°: mouse IgG dilution 1:100; 2°: Alexa Fluor 568 F(ab′)2 fragment goat anti-mouse IgG dilution 1:500). White bars represent 10 μm.
Treatment of BON cells with 10 ng ml−1 recombinant human interleukin-13 (rhIL-13) increases the concentration of 5-hydroxytryptamine (5-HT) in both the cell and media after 24 h. (a) Concentration of 5-HT in serum-free media with or without 10 ng ml−1 of rhIL-13 after 24 h. (b) Concentration of 5-HT in 2.5 × 105 cells treated with or without 10 ng ml−1 of rhIL-13 after 24 h. Each bar represents mean±s.e.m. of four biological replicates (wells). *P<0.05.
Phorbol ester (phorbol-12-myristate-13-acetate (PMA)) induces the release of 5-hydroxytryptamine (5-HT) from BON cells after 1 h in a dose-dependent manner, but recombinant human interleukin-13 (rhIL-13) at three different concentrations does not. BON cells were treated with serum-free media (Control) containing either PMA or rhIL-13 for 1 h at 37 °C. Media were collected and 5-HT concentration was determined by enzyme-linked immunosorbent assay (ELISA). Each bar represents mean±s.e.m. of six biological replicates (wells). a, b and c represent statistical significance. a is significantly different from b and c, b is significantly different than a and c, and all the conditions with c are not significantly different from each other.
IL-13 induces an increase in TPH1 mRNA expression and amount of TPH1 protein
Recent studies have identified two isoforms of the TPH enzyme: TPH1, which is present in mainly peripheral organs such as the EC cells in gut, and TPH2, which is associated with the nervous system and is present predominantly in the brain stem.31, 32 In this study we have detected TPH1 in BON cells and examined its expression over 24 h. TPH1 expression in BON cells has been previously described.33 TPH1 expression in BON cells increases significantly, almost two fold, after 4 h of treatment with rhIL-13, but returns to levels similar to the control at 24 h (Figure 8a). However, TPH1 protein levels, as determined by western blot, were increased after 24 h (Figure 8b).
Time course expression analysis of tryptophan hydroxylase 1 (TPH1) in BON cells treated with and without 10 ng ml−1 recombinant human interleukin-13 (rhIL-13) at 1, 4, 6, and 24 h. (a) Quantitative real-time PCR analysis of TPH1 mRNA expression in BON cells. (b) Representative western blot and relative band density of TPH1 protein expression in BON cells. Each bar represents mean±s.e.m. of four biological replicates (wells). *P<0.05.
IL-13 induces BON cell hyperplasia
The number of BON cells was quantified using two different methods, both of which were found to be significantly elevated in IL-13-treated samples (Figure 9). Trypan blue was used to select for live cells; typically, 97–99% of the cells were found to be viable. Cells were counted manually using a hemocytometer (Figure 9a). Treatment of BON cells with rhIL-13 (10 ng ml−1) for 24 h resulted in significantly increased fluorescence, as determined by the cell viability reagent alamarBlue, which is a function of increased cell number (Figure 9b). The ability of IL-13 to induce BON cell hyperplasia was further confirmed utilizing 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide (MTT) assay, a cell proliferation assay (Figure 9c).
Treatment of BON cells with recombinant human interleukin-13 (rhIL-13) results in increased cell numbers as determined by different methods for quantifying cell numbers. (a) BON cells were treated with and without (Control) 10 ng ml−1 of rhIL-13 in serum-free media for 24 h. Cells were lifted from the plate using trypsin and quantified by hemocytometer. Each bar represents mean±s.e.m. of three biological replicates (wells). (b) BON cells were treated with and without 10 ng ml−1 of rhIL-13 in serum-free media for 24 h. Media were then replaced with 1 × alamarBlue (Invitrogen) in phosphate-buffered saline (PBS) and incubated with the cells for 1 h at 37 °C. Fluorescence was measured using an excitation wavelength of 570 nM and emission wavelength of 585 nm. Each bar represents mean±s.e.m. of six biological replicates (wells). (c) BON cells were treated with and without 10 ng ml−1 of rhIL-13 in serum-free media for 24 h and control is media but no cells. The 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyl tetrazolium bromide (MTT)-based cell growth determination kit (Sigma) was utilized and optical density (OD) was measured at 540 nm. Each bar represents mean±s.e.m. of eight biological triplicates (wells). *P<0.05; **P<0.01; ***P<0.001.
Discussion
5-HT is a well-known neurotransmitter of the central nervous system, and traditionally it is known to influence a range of behavioral, physiological, and cognitive functions. However, the vast majority of 5-HT in the body (∼98%) is found outside of the central nervous system and is generated mainly by the EC cells situated within the epithelial layer of the gut mucosa, which are the best-characterized endocrine cell population in the GI tract.1, 2 Despite the association of alteration in 5-HT response and a variety of GI disorders such as IBS, inflammatory bowel disease, celiac disease, and colorectal cancer, it is not clear how the changes in 5-HT take place, what role 5-HT has in intestinal pathophysiology, and whether by modulating 5-HT production and signaling is it possible to elicit a therapeutic effect. In this study, by employing in vivo mouse model of enteric infection and in vitro model of human EC cells, we have demonstrated a critical role of IL-13 in the development of EC cell hyperplasia and in the upregulation of 5-HT production.
Interactions among immune system, nervous system, and endocrine system have been suggested by a number of studies, and a key player in these neuroimmunoendocrine networks of both human and rodents is 5-HT. The reduced numbers of EC cells in the colon of mice with targeted disruption of IL-2 (ref. 34) and T cell receptor-α,35 and the presence of EC cells in contact with, or very close proximity to, CD3+ lymphocytes28 strongly suggest the existence of the immunological control on EC cells. It is also shown that interferon-γ has an inhibitory effect on proliferation of BON cells.36 Recently, the link between EC cells and the immune system during enteric infection has been examined in several studies.20, 21, 22, 37 Infection with a nematode parasite produces mucosal inflammation and induces changes in intestinal physiology, and thus these models have considerable importance in exploring the pathophysiology of many GI disorders. It has been shown that infection with T. spiralis results in the upregulation of EC cells, and this effect is attenuated in infected T cell receptor knockout mice.20 Utilizing T. muris mouse model of enteric infection, we have previously shown an important connection between immune and endocrine systems in the gut, where secretory products from CD4+ T cells interact with EC cells or their precursors to enhance 5-HT production in the gut via Th2-based mechanisms.21 We have also observed that EC cell and 5-HT responses induced by the same enteric infectious agent are influenced by Th1 or Th2 cytokine predominance, suggesting the importance of the immunological profile of the inflammatory response in the regulation of EC cell biology.22 In addition, it is reported that infection-induced reduction of EC cells numbers in Citrobacter rodenitium is not evident in SCID mice, further indicating an important role of the immune system in mediating EC cell hyperplasia in the gut.36 In this study we observed that EC cell numbers were significantly increased in T. muris–infected wild-type mice as compared with the control. However, in IL-13−/− mice there was no significant increase in EC cell numbers after the infection as compared with the noninfected controls and this impairment in the development of EC cell hyperplasia is accompanied with delayed worm expulsion from the intestine. Treatment of naive IL-13−/− mice with recombinant IL-13 for 5 days significantly increased both EC cell numbers and 5-HT amount in the colon. Administration of rmIL-13, over a 15-day period, in T. muris–infected IL-13−/− mice was also accompanied by upregulation of EC cell numbers and 5-HT content, as well as facilitation of worm expulsion. These observations suggest that IL-13 plays a prominent role in mediating the upregulation of 5-HT-expressing EC cell numbers and in the production of 5-HT in infection-induced inflammatory condition and this may contribute to host defense in this infection.
We have previously reported the expression of IL-13αR but not IL-4 receptor in mouse EC cells in the colon.22 The findings from in vivo investigations that recombinant IL-13 can influence the EC cell numbers in the colon and 5-HT content has led us to hypothesize that IL-13 can regulate 5-HT production by acting directly on EC cells and influencing TPH1 (rate-limiting enzyme of 5-HT synthesis) expression and function of EC cells. In this study we have identified and characterized the expression of IL-13αR in BON cells, a cell culture model of human EC cells. Incubation of BON cells with IL-13 for 24 h results in both increased extracellular and intracellular 5-HT content. TPH1 was originally thought to be regulated at the transcriptional level as slightly elevated nocturnal 5-HT content and TPH1 mRNA levels were found in the rat pineal gland.38, 39 Recent studies have suggested that posttranslational regulation of TPH1 may be more important than transcription activation.39 In BON cells, activation of the phasphatidylinositol-3-kinase/protein kinase B (Akt) signaling pathway results in the loss of TPH1 protein, potentially by posttranslational degradation, with concomitant decrease in 5-HT synthesis.40 TPH1 is a target of cAMP-dependent protein kinase, resulting in phosphorylation of serine 58 in vitro, and an increase in the catalytic activity of TPH1.41, 42 Our study found that TPH1 mRNA expression increased after 4 h of IL-13 treatment and this was associated with upregulation of protein levels of TPH1 at 24 h. These observations provide evidence that IL-13 regulates 5-HT production from EC cells by enhancing TPH1 activity.
A study by Ishizuka et al.43 showed that 5-HT itself can act as a mitogen on BON cells; however, significant differences were only observed after 4 days. In our study we observed that IL-13 treatment increases the number of BON cells in culture after 24 h, which is associated with an increase in 5-HT content within the media. Potentially, 5-HT and IL-13 may act synergistically to increase the number of BON cells in culture as well as a similar mechanism may be responsible for EC cell hyperplasia during a Th2-mediated response to enteric infection.
In conclusion, we have shown that IL-13 plays an important role in the development of EC cell hyperplasia in enteric infection-induced model of gut inflammation. IL-13 secreted from Th2 cells or natural killer T cells44 may control EC cell biology acting via IL-13 receptor on EC cell. In addition, this study also suggests that 5-HT production and worm expulsion share a common immunologic basis and may be causally linked. Using BON cells, a model for human EC cells, we have shown that IL-13 can influence 5-HT synthesis through modulation of TPH1 activity at both the level of mRNA and protein expression. These observations clearly demonstrate a vital role of IL-13 in EC cell biology and 5-HT production and provide important information on immunoendocrine axis in the gut. Furthermore, by manipulating the host immune response, we are able to modulate the accompanying EC cell response and 5-HT production, and this may have clinical relevance. Alterations in EC cell numbers and 5-HT production occur in a variety of clinical settings associated with inflammation and immune activation such as IBS and inflammatory bowel disease. An understanding of the underlying immunological mechanisms of altered EC cell biology, coupled with the ability to modulate EC cell function by immune mediator as depicted in this study, may ultimately yield new therapeutic strategies in these conditions.
Methods
Animals. IL-13−/− mice on a BALB/c background (kindly provided by A. McKenzie, MRC Lab, Cambridge, UK45) were bred at McMaster University. Male IL-13−/− mice and their age-matched (average age 8–11 weeks) wild-type counterparts were used for the purposes of these experiments. The guidelines implemented by the McMaster University Animal Care Committee, Canadian Council on the Use of Laboratory Animals, and the Home Office Scientific Procedures Act (1986) were strictly followed. All mice were kept in sterilized, filter-topped cages, and fed autoclaved food in the animal facilities.
BON cell culture. BON cells (obtained from Dr L. Mayer, Mount Sinai School of Medicine, New York, NY) were maintained in Dulbecco's modified Eagle's medium/F-12 media, containing 10% non-heat-treated fetal calf serum at 37 °C in 5% CO2. Media were changed every 72 h, and all experiments were performed on BON cells from passages 6–14 in this study.
Experimental design for T. muris infection. The techniques used for T. muris maintenance and infection were described previously.46, 47 Mice were infected with ∼300 eggs by oral gavage on day 0 and were killed on days 14 and 21, and at these time points tissue samples were collected. In a separate experiment, IL-13−/− mice were treated with either rmIL-13 (2 μg day−1) or vehicle (phosphate-buffered saline (PBS)) for 15 days, starting 1 day before infection with T. muris. The duration of infection in the latter experiments was 14 days, and thereafter the animals were killed and tissue samples were collected. Additionally, in another experiment, naive IL-13−/− mice were treated with aforementioned rmIL-13 dose or PBS and killed on day 5.
Determination of colonic and intracellular BON cell 5-HT content. Segments of colon or ∼2.5 × 106 BON cells were homogenized in 0.5 ml of 0.2 m perchloric acid, and then centrifuged at 10,000 g for 5 min. The supernatants were neutralized with an equal volume of 1 m borate buffer (pH 9.25) and centrifuged again at 10,000 g for 1 min. The 5-HT content in the supernatant was analyzed using a commercially available kit (Beckman Coulter, Bera, CA). The 5-HT content of BON cells was expressed in weight (ng) per 2.5 × 106 cells, and colonic 5-HT content was expressed as a function of the colon segment's wet weight.
Measurement of 5-HT concentration in BON cell culture media. BON cell conditioned media were removed from cells and centrifuged at 110 g for 5 min to remove cell debris. Media were placed in fresh tubes and frozen at −70 °C until analysis. The 5-HT content in the media was analyzed using a commercially available kit (Beckman Coulter).
Measurement of cytokines in colonic tissues. Frozen colonic tissues were homogenized in lysis buffer (50 mm Tris-HCl (pH 8); 150 mm NaCl; 1% Triton X-100) containing protease inhibitor cocktail (Sigma, St Louis, MO). The homogenate was centrifuged at 10,000 g for 5 min and the supernatants were collected and stored at −80 °C until analysis.
Colon samples were analyzed using a mouse IL-13 and IL-4 ELISA kit (R&D Systems, Minneapolis, MN) according to the manufacturer's instructions. Total protein concentration was measured by DC Protein Assay kit (Bio-Rad Laboratories, Hercules, CA). Cytokine values were expressed as a function of total protein content in each sample.
RNA isolation and reverse transcriptase reaction. RNA from ∼1 × 106 BON cells that were treated with or without 10 ng ml−1 rhIL-13 was isolated using Total RNA Purification kit from Norgen Biotek (Thorold, Ontario, Canada). Purified RNA was quantified and the integrity of RNA was determined using the Experion bio analyzer with a standard sensitivity RNA chip (Bio-Rad Laboratories). All RNA samples were found to be of sufficient integrity with minimal RNA degradation (RNA quality indicator (RQI) >8.5). An aliquot of 3 μg of RNA was used for reverse transcription using 0.5 μg of oligo (dT)12−18 with the M-MLV Research Transcriptase (Invitrogen, Grand Island, NY) kit. The complementary DNA (cDNA) samples were diluted 1:10, and cDNA pooled samples were diluted in a 10-fold serial dilution to create a standard curve with autoclaved ddH2O.
Quantitative Real-time PCR. All real-time PCR reactions were performed using the Bio-Rad CFX 96 PCR system (Bio-Rad Laboratories) and amplification reactions (10 μl) were done using 5 μl of EvaGreen PCR Master Mix (Bio-Rad Laboratories), 1 μl of both the 10 μM reverse and forward primers, 2 μl of autoclaved ddH2O, and 1 μl of diluted cDNA.
The optimal annealing temperature of 58 °C was determined for the TPH1 primers (forward: 5′-TGCCCTTGCTAAGGTCAGCAGGA-3′, reverse: 5′-AGCAAGAGATGGCCCAGACCTCC-3′). The thermal cycling conditions were as follows: initial denaturation of 30 s at 95 °C followed by amplification for 40 cycles of 5 s at 95 °C and 5 s at 58 °C. Using multiple classical internal control genes we assessed the variability of each gene using a random subset of the cDNA samples and assessed the stability of the reference gene using geNorm (http://medgen.ugent.be/~jvdesomp/genorm/) and as described by Vandesompele et al.48 The reference gene primers that we utilized were as follows: glyceraldehyde-3-phosphate dehydrogenase (GAPDH), forward: 5′-CCCTCCAAAATCAAGTGGGGCG-3′ and reverse: 5′-ATGACGAACATGGGGGCATCAGC-3′; β-Actin, forward: 5′-ATGTGGCCGAGGACTTTGATT-3′ and reverse: 5′-AGTGGGGTGGCTTTTAGGATG-3′; Ubiquitin C (UBC), forward: 5′-ATTTGGGTCGCGGTTCTTG-3′ and reverse: 5′-TGCCTTGACATTCTCGATGGT-3′; 18S rRNA, forward: 5′-TCCACAGGAGGCCTACACGCC-3′ and reverse: 5′-TTTCCGCCGCCCATCGATGTT-3′.
We found the 18S rRNA gene to be most stable according to geNorm (average expression stability (M)=0.401) and the other reference genes to be less stable (M=0.548 to 0.526), and therefore the 18S rRNA gene was selected for subsequent relative quantification of TPH1 at each time point.
TPH1 western blotting. Colonic tissue samples of IL-13−/− mice treated with or without rmIL-13 (2 μg day−1 for 5 days) were homogenized in the same manner as samples prepared for determination of tissue cytokine levels. Once again, concentration of the total protein in the solution of homogenized tissue was determined using a DC Protein Assay kit (Bio-Rad).
BON cell lysate was prepared in 6 cm dishes and pre-treated with or without rhIL-13 (10 ng ml−1) for different time periods (1, 4, 6, and 24 h). After treatment, the cells were washed with ice-cold PBS, and 300 μl of lysis buffer (50 mm Tris-HCl (pH 8); 150 mm NaCl; 1% Triton X-100) containing protease and phosphatase inhibitors (0.5 mmol l−1 Na3VO4, 10 mmol l−1 NaF, 1 μmol l−1 leupeptin, 1 μmol l−1 pepstatin, 1 μmol l−1 okadaic acid, and 0.2 mmol l−1 phenylmethylsulfonyl fluoride) was added. An aliquot of the cell lysate was used to determine the protein concentration in each sample.
Before loading onto sodium dodecyl sulfate (SDS)–polyacrylamide gel electrophoresis gels, the samples, both tissue and cell, were diluted 1:1 (vol/vol) with 2 × Laemmli sample buffer (62.5 mmol l−1 Tris-HCl (pH 6.8), 2% (wt/vol) SDS, 50 mmol l−1 dithiothreitol, and 0.01% (wt/vol) bromophenol blue). Aliquots of cell lysates and tissue homogenate (equal amount from each group) containing 20 and 30 μg of protein, respectively, were then subjected to SDS–polyacrylamide gel electrophoresis and then transferred to polyvinylidene difluoride membranes. The total TPH1 protein level was detected using a specific antibody (1:1,000; Abgent, San Diego, CA), and primary antibody detection was performed using horseradish peroxidase–conjugated appropriate secondary antibody. Signal was visualized using enhanced chemiluminescence, and quantified using the ImageJ program (National Institutes of Health, Bethesda, MD).
Immunohistochemistry. Immunohistochemical studies of 5-HT-expressing EC cells were performed on formalin-fixed, paraffin-wax-embedded samples as described previously.22 Briefly, tissue sections were deparaffinized in CitriSolv (Fisher Scientific, Mississauga, Ontario, Canada), and rehydrated in increasingly less ethanol in PBS. Endogenous peroxide activity was blocked for 30 min (DakoCytomation, Burlington, Ontario, Canada). Antigen retrieval was accomplished using hot 10 mM Citrate Buffer (pH 6.0). Nonspecific binding was reduced using 1% bovine serum albumin in PBS; sections were then incubated with 5-HT rabbit antibody (Immunostar, Hudson, WI; 1:5,000; 1 h at room temperature). Secondary antibody was then applied for 30 min (Envision, DakoCytomation; horseradish peroxidise–coupled anti-rabbit secondary reagent; DakoCytomation). Sections were developed with 3,3′-diaminobenzidine and counterstained with Meyer's hematoxylin. Quantification of 5-HT-positive EC cells was conducted by a blinded observer and expressed as number of positive cells per 10 glands.
Immunocytofluorescence. BON cells were grown in a 12-well dish in the presence of a glass circular cover slip. Media were removed and cell washed with PBS. Fixation with 2% paraformaldehyde in PBS was performed first at room temperature for 10 min. Cells were permeabilized with 0.1% Triton X-100 and 0.1% Saponin in PBS at room temperature for 15 min. A second fixation step was then performed with 4% paraformaldehyde in PBS. Cells were blocked with 3% bovine serum albumin in PBS for 1 h at room temperature. Primary antibody at indicated dilution was applied to the cells in PBS containing 3% bovine serum albumin, 0.1% Triton X-100, and 0.1% saponin overnight, shaking at 4 °C. The cells were washed 3 times with PBS containing 0.1% Triton X-100, and 0.1% saponin. Secondary antibody was applied at indicated dilution to cells in PBS containing 3% bovine serum albumin, 0.1% Triton X-100, and 0.1% saponin, shaking at room temperature for 1 h. Cells were then washed 3 times with PBS containing 0.1% Triton X-100, and 0.1% saponin. Cover slips were mounted on to slides using ProLong Gold with 4′,6-diamidino-2-phenylindole (Invitrogen).
BON cell proliferation assay. Commercially available MTT based cell growth determination kit (Sigma) was utilized to measure BON cell proliferation. Approximately 1 × 104 cells in 200 μl of aforementioned medium were seeded in triplicates into 96-well culture plates and incubated for 48 h to allow cell adhesion. Thereafter, 200 μl of serum-free medium either with or without 10 ng ml−1 of rhIL-13 was added to the wells containing cells and incubated at 37 °C, 5% CO2 for 24 h. At the end of incubation, 20 μl of MTT was added to all wells and incubated for an hour and a half, following which the medium was removed and the plate was dried at 37 °C for 1 h. After 1 h, 200 μl of 0.04 M HCl in isopropanol was added to each well and mixed thoroughly. Optical density was measured at 540 nm using a luminometer (EL 808; Bio-Tek Instruments, Winooski, VT).
Statistical analysis. Comparison of the two groups was accomplished using Student's t-test. Comparison of three or more groups was accomplished first using a one-way analysis of variance followed by the Newman-Keuls multiple comparison test unless otherwise indicated. The P-values are designated as follows: *0.05, **0.01, ***0.001, and ****0.0001. All statistical analyses were performed using GraphPad Prism 5 (La Jolla, CA).
References
Khan, W.I. & Ghia, J.E. Gut hormones: emerging role in immune activation and inflammation. Clin. Exp. Immunol. 161, 19–27 (2010).
Erspamer, V. Historical introduction: the Italian contribution to the discovery of 5-hydroxytryptamine (enteramine, serotonin). J. Hypertens. 4 (Suppl), S3–S5 (1986).
Cetin, Y. et al. Enterochromaffin cells of the digestive system: cellular source of guanylin, a guanylate cyclase-activating peptide. Proc. Natl. Acad. Sci. USA 91, 2935–2939 (1994).
Braun, T. et al. Enterochromaffin cells of the human gut: sensors for spices and odorants. Gastroenterology 132, 1890–1901 (2007).
Camilleri, M. Serotonin in the gastrointestinal tract. Curr. Opin. Endocrinol. Diabetes. Obes. 16, 53–59 (2009).
Gershon, M.D. Serotonin: its role and receptors in enteric neurotransmission. Adv. Exp. Med. Biol. 294, 221–230 (1991).
Costedio, M.M., Hyman, N. & Mawe, G.M. Serotonin and its role in colonic function and in gastrointestinal disorders. Dis. Colon Rectum 50, 376–388 (2007).
Spiller, R. Recent advances in understanding the role of serotonin in gastrointestinal motility in functional bowel disorders: alterations in 5-HT signalling and metabolism in human disease. Neurogastroenterol. Motil. 19 (Suppl 2), 25–31 (2007).
Coates, M.D. et al. Molecular defects in mucosal serotonin content and decreased serotonin reuptake transporter in ulcerative colitis and irritable bowel syndrome. Gastroenterology 126, 1657–1664 (2004).
Magro, F. et al. Impaired synthesis or cellular storage of norepinephrine, dopamine, and 5-hydroxytryptamine in human inflammatory bowel disease. Dig. Dis. Sci. 47, 216–224 (2002).
Miwa, J. et al. Patients with constipation-predominant irritable bowel syndrome (IBS) may have elevated serotonin concentrations in colonic mucosa as compared with diarrhea-predominant patients and subjects with normal bowel habits. Digestion 63, 188–194 (2001).
Faure, C. et al. Serotonin signaling is altered in irritable bowel syndrome with diarrhea but not in functional dyspepsia in pediatric age patients. Gastroenterology 139, 249–258 (2010).
Coleman, N.S. et al. Abnormalities of serotonin metabolism and their relation to symptoms in untreated celiac disease. Clin. Gastroenterol. Hepatol. 4, 874–881 (2006).
Ataee, R. et al. Anti-mitogenic and apoptotic effects of 5-HT1B receptor antagonist on HT29 colorectal cancer cell line. J. Cancer. Res. Clin. Oncol. 136, 1461–1469 (2010).
Coogan, P.F., Strom, B.L. & Rosenberg, L. Antidepressant use and colorectal cancer risk. Pharmacoepidemiol. Drug Saf. 18, 1111–1114 (2009).
Costedio, M.M. et al. Serotonin signaling in diverticular disease. J. Gastrointest. Surg. 12, 1439–1445 (2008).
Moore, B.A., Sharkey, K.A. & Mantle, M. Role of 5-HT in cholera toxin-induced mucin secretion in the rat small intestine. Am. J. Physiol. 270, G1001–G1009 (1996).
Grondahl, M.L. et al. Secretory pathways in Salmonella Typhimurium-induced fluid accumulation in the porcine small intestine. J. Med. Microbiol. 47, 151–157 (1998).
Kordasti, S. et al. Serotonin and vasoactive intestinal peptide antagonists attenuate rotavirus diarrhoea. Gut 53, 952–957 (2004).
Wheatcroft, J. et al. Enterochromaffin cell hyperplasia and decreased serotonin transporter in a mouse model of postinfectious bowel dysfunction. Neurogastroenterol. Motil. 17, 863–870 (2005).
Wang, H. et al. CD4+ T cell-mediated immunological control of enterochromaffin cell hyperplasia and 5-hydroxytryptamine production in enteric infection. Gut 56, 949–957 (2007).
Motomura, Y. et al. Enterochromaffin cell and 5-hydroxytryptamine responses to the same infectious agent differ in Th1 and Th2 dominant environments. Gut 57, 475–481 (2008).
Ghia, J.E. et al. Serotonin has a key role in pathogenesis of experimental colitis. Gastroenterology 137, 649–1660 (2009).
Li, N. et al. Serotonin activates dendritic cell function in the context of gut inflammation. Am. J. Pathol. 178, 662–671 (2011).
Chadwick, V.S. et al. Activation of the mucosal immune system in irritable bowel syndrome. Gastroenterology 122, 1778–1783 (2002).
Collins, S.M., Piche, T. & Rampal, P. The putative role of inflammation in the irritable bowel syndrome. Gut 49, 743–745 (2001).
Spiller, R. & Garsed, K. Postinfectious irritable bowel syndrome. Gastroenterology 136, 1979–1988 (2009).
Yang, G.B. & Lackner, A.A. Proximity between 5-HT secreting enteroendocrine cells and lymphocytes in the gut mucosa of rhesus macaques (Macaca mulatta) is suggestive of a role for enterochromaffin cell 5-HT in mucosal immunity. J. Neuroimmunol. 146, 46–49 (2004).
Evers, B.M. et al. The human carcinoid cell line, BON. A model system for the study of carcinoid tumors. Ann. NY Acad. Sci. 733, 393–406 (1994).
Li, J. et al. Phorbol ester-mediated neurotensin secretion is dependent on the PKC-alpha and -delta isoforms. Am. J. Physiol. Gastrointest. Liver Physiol. 283, G1197–G1206 (2002).
Walther, D.J. et al. Synthesis of serotonin by a second tryptophan hydroxylase isoform. Science 299, 76 (2003).
Walther, D.J. & Bader, M. A unique central tryptophan hydroxylase isoform. Biochem. Pharmacol. 66, 1673–1680 (2003).
Vikman, S. et al. Gene expression in midgut carcinoid tumors: potential targets for immunotherapy. Acta. Oncol. 44, 32–40 (2005).
Qian, B.F., El-Salhy, M., Melgar, S., Hammarstrom, M.L. & Danielsson, A. Neuroendocrine changes in colon of mice with a disrupted IL-2 gene. Clin. Exp. Immunol. 120, 424–433 (2000).
Rubin, D.C. et al. Altered enteroendocrine cell expression in T cell receptor alpha chain knock-out mice. Microsc. Res. Tech. 51, 112–120 (2000).
O'Hara, J.R. et al. Consequences of Citrobacter rodentium infection on enteroendocrine cells and the enteric nervous system in the mouse colon. Cell. Microbiol. 8, 646–660 (2006).
Sun, X. et al. Circadian 5-HT production regulated by adrenergic signaling. Proc. Natl. Acad. Sci. USA 99, 4686–4691 (2002).
Sugden, D. Comparison of circadian expression of tryptophan hydroxylase isoform mRNAs in the rat pineal gland using real-time PCR. J. Neurochem. 86, 1308–1311 (2003).
Huang, Z. et al. Posttranslational regulation of TPH1 is responsible for the nightly surge of 5-HT output in the rat pineal gland. J. Pineal Res. 45, 506–514 (2008).
Silva, S.R. et al. The effect of PTEN on serotonin synthesis and secretion from the carcinoid cell line BON. Anticancer Res. 31, 1153–1160 (2011).
Kuhn, D.M., Arthur, R. Jr & States, J.C. Phosphorylation and activation of brain tryptophan hydroxylase: identification of serine-58 as a substrate site for protein kinase A. J. Neurochem. 68, 2220–2223 (1997).
Kumer, S.C. et al. Amino-terminal analysis of tryptophan hydroxylase: protein kinase phosphorylation occurs at serine-58. J. Neurochem. 69, 1738–1745 (1997).
Ishizuka, J. et al. Receptor-mediated autocrine growth-stimulatory effect of 5-hydroxytryptamine on cultured human pancreatic carcinoid cells. J. Cell. Physiol. 150, 1–7 (1992).
Godfrey, D.I., MacDonald, H.R., Kronenberg, M., Smyth, M.J. & Van Kaer, L. NKT cells: what's in a name? Nat. Rev. Immunol. 4, 231–237 (2004).
McKenzie, G.J. et al. A distinct role for interleukin-13 in Th2-cell-mediated immune responses. Curr. Biol. 8, 339–342 (1998).
Wakelin, D. Studies on the immunity of albino mice to Trichuris muris. The stimulation of immunity by chemically abbreviated infections. Parasitology 59, 549–555 (1969).
Else, K.J. et al. The influence of genes mapping within the major histocompatibility complex on resistance to Trichuris muris infections in mice. Parasitology 101, 61–67 (1990).
Vandesompele, J. et al. Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genome Biol. 3, RESEARCH0034 (2002).
Smith, J.W. & Castro, G.A. Relation of peroxidase activity in gut mucosa to inflammation. Am. J. Physiol. 234, R72–R79 (1978).
Acknowledgements
This work is supported by the grants from the Canadian Institutes of Health Research (CIHR) and Crohn's and Colitis Foundation of Canada (CCFC) to Dr Khan. Dr Khan is a recipient of CIHR New Investigator Award. The authors thank Dr SM Atiqur Rahman for his valuable input.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declared no conflict of interest.
Rights and permissions
About this article
Cite this article
Manocha, M., Shajib, M., Rahman, M. et al. IL-13-mediated immunological control of enterochromaffin cell hyperplasia and serotonin production in the gut. Mucosal Immunol 6, 146–155 (2013). https://doi.org/10.1038/mi.2012.58
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/mi.2012.58
This article is cited by
-
Dual infective burden of Helicobacter pylori and intestinal parasites: Good or bad news for the host?
Indian Journal of Gastroenterology (2020)
-
Selective inhibition of intestinal 5-HT improves neurobehavioral abnormalities caused by high-fat diet mice
Metabolic Brain Disease (2019)
-
Mast Cells and Serotonin Synthesis Modulate Chagas Disease in the Colon: Clinical and Experimental Evidence
Digestive Diseases and Sciences (2018)