Abstract
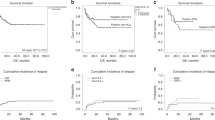
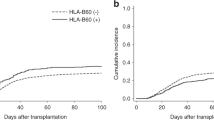
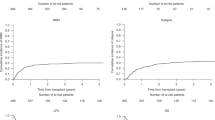
Prior data indicate similar outcomes after transplants from human leukocyte antigen (HLA)-haplotype-matched relatives, HLA-identical siblings and HLA-matched unrelated donors. We used our prospective data set to answer a clinically important question: who is the best donor for a person with acute leukaemia transplanted in first complete remission. Patients were randomly divided into training (n=611) and validation (n=588) sets. A total of 1199 consecutive subjects received a transplant from an HLA-haplotype-matched relative using granulocyte colony-stimulating factor and anti-thymocyte globulin (n=685) or an HLA-identical sibling (n=514); 3-year leukaemia-free survivals (LFSs) were 75 and 74% (P=0.95), respectively. The multivariate model identified three major risk factors for transplant-related mortality (TRM): older donor/recipient age, female-to-male transplants and donor–recipient ABO major-mismatch transplants. A risk score was developed based on these three features. TRMs were 8%, 15% and 31% for subjects with scores of 0–1, 2 and 3, respectively, (P<0.001). Three-year LFSs were 78%, 74% and 58%, respectively, (P=0.003). The risk score was validated in an independent cohort. In conclusion, our data confirm donor source is not significantly correlated with transplant outcomes. Selection of the best donor needs to consider donor–recipient age, matching for gender and ABO incompatibility among persons with acute leukaemia receiving related transplants under our transplant modality.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Raiola AM, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transplant 2013; 19: 117–122.
Kasamon YL, Luznik L, Leffell MS, Kowalski J, Tsai HL, Bolaños-Meade J et al. Nonmyeloablative HLA-haploidentical bone marrow transplantation with high-dose posttransplantation cyclophosphamide: effect of HLA disparity on outcome. Biol Blood Marrow Transplant 2010; 16: 482–489.
Wang Y, Chang YJ, Xu LP, Liu KY, Liu DH, Zhang XH et al. Who is the best donor for a related HLA haplotype-mismatched transplant? Blood 2014; 124: 843–850.
Kollman C, Howe CW, Anasetti C, Antin JH, Davies SM, Filipovich AH et al. Donor characteristics as risk factors in recipients after transplantation of bone marrow from unrelated donors: the effect of donor age. Blood 2001; 98: 2043–2051.
Loren AW, Bunin GR, Boudreau C, Champlin RE, Cnaan A, Horowitz MM et al. Impact of donor and recipient sex and parity on outcomes of HLA-identical sibling allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2006; 12: 758–769.
Bashey A, Zhang X, Sizemore CA, Manion K, Brown S, Holland HK et al. T-cell-replete HLA-haploidentical hematopoietic transplantation for hematologic malignancies using post-transplantation cyclophosphamide results in outcomes equivalent to those of contemporaneous HLA-matched related and unrelated donor transplantation. J Clin Oncol 2013; 31: 1310–1316.
Raiola AM, Dominietto A, di Grazia C, Lamparelli T, Gualandi F, Ibatici A et al. Unmanipulated haploidentical transplants compared with other alternative donors and matched sibling grafts. Biol Blood Marrow Transplant 2014; 20: 1573–1579.
Di Stasi A, Milton DR, Poon LM, Hamdi A, Rondon G, Chen J et al. Similar transplantation outcomes for acute myeloid leukemia and myelodysplastic syndrome patients with haploidentical versus 10/10 human leukocyte antigen-matched unrelated and related donors. Biol Blood Marrow Transplant 2014; 20: 1975–1981.
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood 2006; 107: 3065–3073.
Xiao-Jun Hl, Lan-Ping X, Kai-Yan L, Dai-Hong L, Yu W, Huan C et al. Partially matched related donor transplantation can achieve outcomes comparable to unrelated donor transplantation for patients with hematologic malignancies. Clin Cancer Res 2009; 15: 4777–4783.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X et al. Haploidentical versus matched-sibling transplant in adults with Philadelphia-negative high-risk acute lymphoblastic leukemia: a biologically phase 3 randomized study. Clin Cancer Res 2016; 22: 3467–3476.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X et al. Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood 2015; 125: 3956–3962.
Jagasia M, Arora M, Flowers ME, Chao NJ, McCarthy PL, Cutler CS et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood 2012; 119: 296–307.
Huang XJ, Zhu HH, Chang YJ, Xu LP, Liu DH, Zhang XH et al. The superiority of haploidentical related stem cell transplantation to chemotherapy alone as postremission treatment for patients with intermediate- or high-risk acute myeloid leukemia in first complete remission. Blood 2012; 119: 5584–5590.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on acute GVHD grading. Bone Marrow Transplant 1995; 15: 825–828.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE et al. Chronic graft-versus-host syndrome in man: a long-term clinicopathologic study of 20 Seattle patients. Am J Med 1980; 69: 204–217.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant 2005; 11: 945–956.
Eisner MD, August CS . Impact of donor and recipient characteristics on the development of acute and chronic graft‐versus‐host disease following pediatric bone marrow transplantation. Bone Marrow Transplant 1995; 15: 663–668.
Weisdorf D, Hakke R, Blazar B, Miller W, McGlave P, Ramsay N et al. Risk factors for acute graft‐versus‐host disease in histocompatible donor bone marrow transplantation. Transplantation 1991; 51: 1197–1203.
Miller RA . The aging immune system: primer and prospectus. Science 1996; 273: 70–74.
Lipschitz DA, Udupa KB, Indelicato SR, Das M . Effect of age on second messenger generation in neutrophils. Blood 1991; 78: 1347–1354.
Chang YJ, Xu LP, Liu DH, Liu KY, Han W, Chen YH et al. Platelet recovery in patients with hematologic malignancies following unmanipulated haploidentical blood and marrow transplantation: effects of CD34+ cell dose and disease status. Biol Blood Marrow Transplant 2009; 15: 632–638.
Wang YT, Zhao XY, Zhao XS, Xu LP, Zhang XH, Wang Y et al. The impact of donor characteristics on the immune cell composition of mixture allografts of granulocyte-colony-stimulating factor-mobilized marrow harvests and peripheral blood harvests. Transfusion 2015; 55: 2874–2881.
Kröger N, Zabelina T, de Wreede L, Berger J, Alchalby H, van Biezen A et al. Allogeneic stem cell transplantation for older advanced MDS patients: improved survival with young unrelated donor in comparison with HLA-identical siblings. Leukemia 2013; 27: 604–609.
Alousi AM, Le‐Rademacher J, Saliba RM, Appelbaum FR, Artz A, Benjamin JD et al. Who is the better donor for older hematopoietic transplant recipients: an older‐aged sibling or a young, matched unrelated volunteer? Blood 2013; 121: 2567–2573.
Randolph SSB, Gooley TA, Warren EH, Appelbaum FR, Riddell SR . Female donors contribute to a selective graft-versus-leukemia effect in male recipients of HLA matched, related hematopoietic stem cell transplants. Blood 2004; 103: 347–352.
Carlens S, Rihgden O, Remberger M, Lönnqvist B, Hägglund H, Klaesson S et al. Risk factors for chronic graft-versus-host disease after bone marrow transplantation: a retrospective single-center analysis. Bone Marrow Transplant 1998; 22: 755–761.
Miklos DB, Kim HT, Miller KH, Guo L, Zorn E, Lee SJ et al. Antibody responses to H-Y minor histocompatibility antigens correlate with chronic graft-versus-host disease and disease remission. Blood 2005; 105: 2973–2978.
Nakasone H, Remberger M, Tian L, Brodin P, Sahaf B, Wu F et al. Risks and benefits of sex-mismatched hematopoietic cell transplantation differ by conditioning strategies. Haematologica 2015; 100: 1477–1485.
Nakasone H, Tian L, Sahaf B, Kawase T, Schoenrock K, Perloff S et al. Allogeneic HY antibodies detected 3 months after female-to-male HCT predict chronic GVHD and nonrelapse mortality in humans. Blood 2015; 125: 3193–3201.
Ciurea SO, Champlin RE . Donor selection in T cell-replete haploidentical hematopoietic stem cell transplantation: knowns, unknowns, and controversies. Biol Blood Marrow Transplant 2013; 19: 180–184.
Gajewski J, Johnson VV, Sandler SG, Sayegh A, Klumpp TR . A review of transfusion practice before, during and after hematopoietic progenitor cell transplantation. Blood 2008; 112: 3036–3047.
Guttridge MG, Sidders C, Booth-Davey E, Pamphilon D, Watt SM . Factors affecting volume reduction and red blood cell depletion of bone marrow on the COBE Spectra cell separator before hematopoietic stem cell transplantation. Bone Marrow Transplant 2006; 38: 175–181.
Ramírez P, Brunstein CG, Miller B, Defor T, Weisdorf D . Delayed platelet recovery after allogeneic transplantation: a predictor of increased treatment-related mortality and poorer survival. Bone Marrow Transplant 2011; 46: 981–986.
Tomonari A, Takahashi S, Ooi J, Tsukada N, Konuma T, Kobayashi T et al. Impact of ABO incompatibility on engraftment and transfusion requirement after unrelated cord blood transplantation: a single institute experience in Japan. Bone Marrow Transplant 2007; 40: 523–528.
Eiz‐Vesper B, Seltsam A, Blasczyk R . ABO glycosyltransferases as potential source of minor histocompatibility antigens in allogeneic peripheral blood progenitor cell transplantation. Transfusion 2005; 45: 960–968.
Seebach JD, Stussi G, Passweg JR, Loberiza FR Jr, Gajewski JL, Keating A et al. ABO blood group barrier in allogeneic bone marrow transplantation revisited. Biol Blood Marrow Transplant 2005; 11: 1006–1013.
Kollman C, Klein JP, Spellman SR, Hassebroek A, Confer D, Fernandez-Vina M et al. The effect of donor characteristics on graft vs. host disease (GVHD) and survival after unrelated donor transplantation for hematologic malignancy. Biol Blood Marrow Transplant 2013; 19: S146–S147.
Sorror M, Storer B, Sandmaier BM, Maloney DG, Chauncey TR, Langston A et al. Hematopoietic cell transplantation-comorbidity index and Karnofsky performance status are independent predictors of morbidity and mortality after allogeneic nonmyeloablative hematopoietic cell transplantation. Cancer 2008; 112: 1992–2001.
Armand PI, Gibson CJ, Cutler C, Ho VT, Koreth J, Alyea EP et al. A disease risk index for patients undergoing allogeneic stem cell transplantation. Blood 2012; 120: 905–913.
Gratwohl A . The EBMT risk score. Bone Marrow Transplant 2012; 47: 749–756.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 2005; 106: 2912–2919.
Acknowledgements
This work was partly supported by grants from National Natural Science Foundation of China (grant nos. 81400143, 81530046 and 81621001); Collaborative Innovation Center of Hematology, China; the Science and Technology Project of Guangdong Province of China (grant no. 2016B030230003); and the Beijing Municipal Science and Technology Program (grant no. Z141100000214011).
Author contributions
X-JH designed the research; YW and X-JH analysed the data and wrote the manuscript; and all authors provided patient data and gave final approval for the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wang, Y., Wu, DP., Liu, QF. et al. Donor and recipient age, gender and ABO incompatibility regardless of donor source: validated criteria for donor selection for haematopoietic transplants. Leukemia 32, 492–498 (2018). https://doi.org/10.1038/leu.2017.199
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2017.199
This article is cited by
-
Comparison of outcomes for patients with acute myeloid leukemia undergoing haploidentical stem cell transplantation in first and second complete remission
Annals of Hematology (2023)
-
Efficacy and safety of CD19 CAR-T cell therapy for acute lymphoblastic leukemia patients relapsed after allogeneic hematopoietic stem cell transplantation
International Journal of Hematology (2022)
-
Comparison of non-first-degree related donors and first-degree related donors in haploidentical HSCT: a multi-centre retrospective analysis
Bone Marrow Transplantation (2021)
-
Allogeneic hematopoietic stem cell transplantation for intermediate-risk acute myeloid leukemia in the first remission: outcomes using haploidentical donors are similar to those using matched siblings
Annals of Hematology (2021)
-
Epstein–Barr virus and cytomegalovirus reactivation after allogeneic hematopoietic cell transplantation in patients with non–Hodgkin lymphoma: the prevalence and impacts on outcomes
Annals of Hematology (2021)