Abstract
Treatment with azacitidine (AZA), a demethylating agent, prolonged overall survival (OS) vs conventional care in patients with higher-risk myelodysplastic syndromes (MDS). As median survival with monotherapy is <2 years, novel agents are needed to improve outcomes. This phase 1b/2b trial (n=113) was designed to determine the maximum tolerated dose (MTD) or recommended phase 2 dose (RP2D) of panobinostat (PAN)+AZA (phase 1b) and evaluate the early efficacy and safety of PAN+AZA vs AZA monotherapy (phase 2b) in patients with higher-risk MDS, chronic myelomonocytic leukemia or oligoblastic acute myeloid leukemia with <30% blasts. The MTD was not reached; the RP2D was PAN 30 mg plus AZA 75 mg/m2. More patients receiving PAN+AZA achieved a composite complete response ([CR)+morphologic CR with incomplete blood count+bone marrow CR (27.5% (95% CI, 14.6–43.9%)) vs AZA (14.3% (5.4–28.5%)). However, no significant difference was observed in the 1-year OS rate (PAN+AZA, 60% (50–80%); AZA, 70% (50–80%)) or time to progression (PAN+AZA, 70% (40–90%); AZA, 70% (40–80%)). More grade 3/4 adverse events (97.4 vs 81.0%) and on-treatment deaths (13.2 vs 4.8%) occurred with PAN+AZA. Further dose or schedule optimization may improve the risk/benefit profile of this regimen.
Similar content being viewed by others
Introduction
Myelodysplastic syndromes (MDS) represent a heterogeneous group of myeloid disorders characterized by severe cytopenias and dysplasias in one or more myeloid lineages. Subclassification of MDS according to several prognostic systems identifies patients at substantial risk for transformation to acute myeloid leukemia (AML), which is generally refractory to standard treatment.1 MDS remains incurable without stem cell transplant, but eligibility is restricted by the advanced age of patients.2 Azacitidine (AZA), the current standard frontline therapy for higher-risk MDS, significantly prolonged overall survival (OS) in these patients and has shown clinical benefit in those with AML.3, 4, 5 However, response rates with AZA therapy are generally <30%6, 7 and of limited durability, with all nontransplanted patients eventually progressing or dying, highlighting the significant need for novel agents that improve both response rates and duration of responses.
Panobinostat (PAN) is a potent oral pan-deacetylase inhibitor (DACi) approved in the United States, the European Union, Japan and Switzerland for patients with multiple myeloma.8 PAN modulates the acetylation of histone proteins and protein chaperones in malignant cells. The epigenetic regulation by PAN is primarily mediated through the inhibition of class I histone deacetylase (HDAC) enzymes, leading to increased histone acetylation, relaxation of chromatin and alteration of gene expression, including that of tumor suppressor genes.9 In a phase 1a/2 study of PAN in patients with advanced hematologic malignancies, a manageable safety profile was established, but only modest efficacy was demonstrated in patients with AML or MDS.10
In recent years, the involvement of epigenetic processes in the pathogenesis of MDS and the transformation to AML has been extensively studied. Several preclinical and clinical studies have demonstrated hypermethylation of CpG islands at the promoter regions of a number of genes.11 Additionally, epigenetic silencing of tumor suppressor genes in MDS, potentially mediated through dysregulated histone acetylation, has been associated with transformation to AML and poor prognosis.12 That both AZA and DACi modulate aberrant gene expression by different mechanisms suggests that they may act synergistically in MDS and AML. Preclinically, synergy of PAN and demethylating agents has been established in primary AML cells, with the combination of PAN and decitabine leading to a significant reduction in AML cell viability compared with either agent alone.13 A limited number of clinical trials investigating the combination of DACi and demethylating agents have been fully reported. Findings from early-phase clinical trials of AZA plus the DACi valproic acid with or without all-trans retinoic acid have shown promising response rates.14, 15 As PAN is among the most potent DACi in clinical development,16 we hypothesized that the addition of PAN could improve the clinical benefit of AZA monotherapy. On the basis of these data, the current phase 1b/2b study was designed to determine the maximum tolerated dose (MTD) or recommended phase 2 dose (RP2D), and the early efficacy and safety, of PAN in combination with AZA in patients with high-risk MDS, oligoblastic AML or chronic myelomonocytic leukemia (CMML).
Patients and methods
Patients
Adult patients (aged ⩾18 years) with International Prognostic Scoring System (IPSS) intermediate-2- or high-risk MDS, CMML or AML with multilineage dysplasia and ⩽30% bone marrow blasts who were not planning to undergo hematopoietic stem cell transplant were enrolled. Key inclusion criteria were an Eastern Cooperative Oncology Group performance status (ECOG PS) ⩽2 and adequate hepatic and renal function. Patients with therapy-related MDS or AML, relapsed/refractory AML, clinical symptoms of central nervous system leukemia, or impaired cardiac function were excluded. Additionally, patients who had received prior treatment with a DACi, AZA or decitabine, or who were currently receiving a drug known to prolong the QT interval that could not be terminated, were not eligible. The study protocol was reviewed by the independent ethics committee or institutional review board at each center, and written informed consent was obtained from each patient prior to screening.
Study design
This was an open-label, multicenter, international, phase 1b/2b study. In phase 1b, the primary objective was determination of the MTD or RP2D of PAN in combination with AZA (Figure 1). Other objectives included early analyses of the regimen’s safety and efficacy. Patients were enrolled in escalating dose cohorts consisting of ⩾3 patients each. The starting dose of PAN was 20 mg administered orally on days 3, 5, 8, 10, 12 and 15 in combination with AZA 75 mg/m2 administered on days 1 to 7 in 4-week cycles. Successive cohorts received escalating doses of PAN until determination of MTD or RP2D. AZA was administered according to its label. Dose reductions or interruptions of PAN and AZA were permitted, but the PAN dose was not to decrease below 10 mg, and no cycle could be extended longer than 42 days. Patients were evaluated for dose-limiting toxicities (DLTs), and dose escalation was guided by an adaptive Bayesian logistic regression model (BLRM). The MTD could not be declared until ⩾9 patients were evaluated at that dose level.
Study design. In phase 1b, patients received escalating doses of PAN in combination with AZA. In phase 2b, patients were randomized to receive treatment with either the RP2D of PAN+AZA or single-agent AZA. AML, acute myeloid leukemia; AZA, azacitidine; CMML, chronic myelomonocytic leukemia; ECOG PS, Eastern Cooperative Oncology Group performance status; IPSS Int-2, International Prognostic Scoring System intermediate 2; MDS, myelodysplastic syndrome; MTD, maximum tolerated dose; PAN, panobinostat; RP2D, recommended phase 2 dose.
Upon determination of the MTD or RP2D defined in phase 1b, an additional 80 patients were to be enrolled in the phase 2b portion and randomly assigned in the ratio 1:1 following Interactive Response Technology procedures to receive either the MTD/RP2D of PAN plus AZA (PAN+AZA) or single-agent AZA on a treatment schedule identical to that from phase 1b. Because the study population consisted of patients with three different indications (MDS, CMML and AML) with varying response assessment criteria, a composite end point that could be used across all three indications to obtain an overall response assessment was devised. This composite end point was named 'composite complete response' (composite CR) and pooled together 'complete response/complete remission' (CR; applicable to both AML and MDS/CMML), 'morphologic CR with incomplete blood count' (CRi; applicable to AML) and 'bone marrow CR' (BM-CR; applicable to MDS/CMML). The primary objective of phase 2b was to assess the early efficacy of PAN at the MTD/RP2D in combination with AZA vs AZA alone through the assessment of composite CR. Secondary objectives included efficacy assessment of clinical responses other than composite CR, 1-year survival, time to progression and assessment of safety in comparison with single-agent AZA.17, 18 Patients in both phases were allowed to continue study treatment until disease progression, unacceptable toxicity or withdrawal of consent.
Safety and efficacy assessments
Patients were monitored for safety throughout the trial and up to 28 days after the last dose of study treatment. Adverse events (AEs) were assessed according to the Common Terminology Criteria for Adverse Events version 3.0. Safety evaluations included monitoring of hematology, blood chemistry and urine, and regular assessment of vital signs, physical condition, body weight, ECOG PS and cardiac monitoring.
Assessment of response was made per the investigator, based on standardized criteria proposed by the international working groups for AML17 and MDS/CMML.18 Response during study treatment was evaluated via blood and bone marrow assessment. Bone marrow aspiration and/or core biopsy was obtained within 5 days of the planned end of even-numbered cycles, at the end of treatment visit and at the discretion of the investigator. Peripheral blood assessments were performed within 5 days of bone marrow aspiration/biopsy, unless not clinically feasible.
Bone marrow aspirate samples were collected at screening from patients in phase 2b and sent for next-generation sequencing analysis (NGS; Genoptix, Carlsbad, CA, USA). Genomic DNA was isolated from the samples, and the coding regions of 24 genes (Supplementary Table 1) were amplified by polymerase chain reaction and sequenced using NGS technology (MiSeq system; Illumina, Inc, San Diego, CA, USA). Somatic mutations consistent with AML, MDS or myeloproliferative neoplasms were identified. This study is registered at http://clinicaltrials.gov as NCT00946647.
Statistical analysis
An adaptive BLRM and dose-escalation criteria similar to that proposed by Babb, Rogatko and Zacks, including the escalation with overdose control principle,19 was used to guide dose escalation in phase 1b. The study was not designed for hypothesis testing of comparisons between the treatment arms. Point estimates and 95% exact binomial CIs20 were computed to provide descriptive summaries of response rates. The 1-year survival probabilities were estimated from the Kaplan−Meier curve. All analyses were done using SAS software (version 9.3) and R software (version 2.13).
Results
Patients and disposition
A total of 113 patients were enrolled in the study and received treatment starting 4 December 2009; data cutoff for this analysis was 30 April 2014, corresponding to the time point at which the last patient enrolled in the phase 2 part of the study should have completed 12 cycles of treatment. In phase 1b, 31 patients (median age, 69 years; Table 1) received PAN in dosing cohorts of 20 mg (n=6), 30 mg (n=18) and 40 mg (n=7). At the time of data cutoff, four patients remained on treatment (30 mg (n=3); 40 mg (n=1)). Patients in phase 1b had diagnoses of MDS (n=16), CMML (n=4) and AML (n=11). The majority of patients with MDS were previously untreated (81.3%), categorized as IPSS intermediate-2 (87.5%) or high risk (12.5%) at study entry, and had favorable cytogenetics per IPSS (62.5%); 12.5% had unfavorable cytogenetics. Among the patients with CMML, 75% were previously untreated. All patients with AML were previously untreated for AML; 72.7% had prior MDS that transformed to AML, and 1 of these patients received prior treatment with lenalidomide for MDS. The majority of patients with AML (54.5%) had unfavorable cytogenetics; the remaining 45.5% had intermediate cytogenetic risk. The median time from initial diagnosis to study entry for patients with MDS, CMML and AML was 1.3 months (range, 0.5–37.9 months), 1.8 months (range, 0.8–3.2 months) and 0.7 months (range, 0.2–2.5 months), respectively. Most patients had an initial ECOG PS of either 0 (41.9%) or 1 (48.4%). Demographics and baseline characteristics for patients in phase 1b are presented in Table 1.
Eighty-two patients (median age, 71 years) were enrolled in phase 2b and randomized to receive treatment with PAN+AZA (n=40) or AZA (n=42). At the time of data cutoff, 13 patients remained on treatment (PAN+AZA (n=7); AZA (n=6)). Of the 82 phase 2b patients, 47 (57.3%), 13 (15.9%) and 22 (26.8%) had a diagnosis of MDS, CMML and AML, respectively. The majority of patients with MDS were previously untreated (89.4%), and 44.7% had unfavorable cytogenetics (patients with favorable and intermediate cytogenetics accounted for 27.7% each). Patients with CMML were primarily untreated (84.6%), and nearly all patients with AML (95.5%) were previously untreated for AML. Most patients with AML had multilineage dysplasia with 21–30% bone marrow blasts (95.5%), with 77.3% of these patients having prior MDS that transformed to AML and 81.8% having intermediate- or high-risk cytogenetics. ECOG PS at baseline was primarily 0 (41.5%) or 1 (52.4%). A comparison of demographics and baseline characteristics between treatment arms is presented in Table 2.
Determination of MTD or RP2D
Of the 31 patients enrolled in phase 1b, 26 were evaluable for MTD determination (20 mg, n=5; 30 mg, n=14; 40 mg, n=7). Six DLTs were observed. In the 20-mg cohort, one patient experienced a DLT of septic shock. Three patients in the 30-mg cohort experienced DLTs, which included atrial fibrillation and syncope, dehydration and fatigue, and colitis. In the 40-mg cohort, two patients experienced DLTs of grade 3 nausea and vomiting and grade 3 hyperbilirubinemia. The MTD for PAN was not reached. Although DLTs were rare, two patients (29%) required at least one PAN dose reduction and one patient (14%) required at least one AZA dose reduction. Based on the BLRM and safety findings, the 30- mg dose was selected as the RP2D.
Safety
During phase 1b dose escalation, nearly all patients (96.8%) reported ⩾1 grade 3/4 AE, regardless of study drug relationship. The most common grade 3/4 AEs (in ⩾20% of patients) were primarily hematologic, including thrombocytopenia (54.8%), neutropenia (41.9%), anemia (32.3%) and febrile neutropenia (29.0%; Table 3). Three patients (9.7%) died while on treatment (or ⩽28 days after the end of treatment) from underlying malignancy (n=2) and renal insufficiency not attributed to study treatment (n=1).
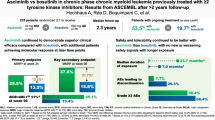
In phase 2b, a total of 80 randomized patients (38, PAN+AZA; 42, AZA) received at least one dose of study treatment and were included in the safety set. The median duration of treatment with PAN was 20.5 weeks (5.1 cycles; range, 0.03–23.3 cycles), and the median duration of treatment with AZA was 23.4 weeks (5.9 cycles; range, 0.1–23.4 cycles) in the PAN+AZA arm vs 16.9 weeks (4.2 cycles; range, 0.03–23.6 cycles) in the AZA arm. A summary of frequent AEs by treatment group in phase 2b is presented in Table 4. A greater proportion of patients in the PAN+AZA arm experienced ⩾1 grade 3/4 AE compared with the AZA arm (97.4 vs 81.0%). The most common grade 3/4 AEs with higher incidence in the PAN+AZA arm than the AZA arm were thrombocytopenia (55.3 vs 19.0%), febrile neutropenia (31.6 vs 19.0%) and anemia (21.1 vs 11.9%). A slightly higher proportion of patients in the PAN+AZA arm vs the control arm experienced ⩾1 serious AE (71.1 vs 64.3%), with febrile neutropenia (26.3 vs 14.3%), pneumonia (18.4 vs 9.5%), sepsis (7.9 vs 7.1%), thrombocytopenia (7.9 vs 7.1%), sepsis during neutropenia (0 vs 7.1%), pyrexia (5.3 vs 0%) and septic shock (5.3 vs 0%) being the most common serious AEs reported in >5% of patients in either arm. In the PAN+AZA arm, a relative dose intensity of ⩾90% was achieved with PAN in only 47.4% of patients and with AZA in 71.1%. In the AZA arm, 73.8% of patients had a relative dose intensity ⩾90%. A greater proportion of patients in the PAN+AZA arm discontinued treatment due to AEs (36.8 vs 23.8%). There were seven on-treatment deaths (PAN+AZA, n=5 (13.2%); AZA, n=2 (4.8%)), all of which occurred between cycles 1 and 3. None of the patients were known to be in response. In the PAN+AZA arm, one patient died due to MDS and two patients died due to causes that the investigator suspected to be treatment-related (septic shock during grade 4 febrile neutropenia and pulmonary hemorrhage during grade 4 thrombocytopenia). Neither of the deaths in the AZA arm was suspected to be treatment-related.
Early efficacy
Phase 1b. The clinical response rates were 33.0%, 33.0% and 42.9% in the 20-, 30- and 40-mg cohorts, respectively.
Among patients with MDS/CMML across all dose cohorts, a clinical response (CR, BM-CR, partial response (PR) or hematologic improvement (HI)) was observed in six patients (30.0%; 95% CI, 11.9–54.3%), with 2 CRs (10.0%), 2 BM-CRs (10.0%), 1 PR (5.0%) and 1 HI (5.0%). Erythroid and platelet responses were observed in 3 patients (15.0%) each, and no patients had a neutrophil response. Two patients relapsed following HI.
Five patients (45.5%; 95% CI, 16.7–76.6%) with AML showed a clinical response (CR, CRi, PR), including 2 CRs (18.2%) and 3 CRi's (27.3%). Treatment failure was observed in 3 patients (27.3%), and best overall response was unknown in 3 patients (27.3%). One patient with AML relapsed following CRi.
Phase 2b. A higher proportion of patients achieved a composite CR in the PAN+AZA arm (27.5%; 95% CI, 14.6–43.9%) vs the AZA arm (14.3%; 95% CI, 5.4–28.5%), including a slightly higher proportion of patients achieving a CR (15.0 vs 9.5%) or achieving a CRi or BM-CR (12.5 vs 4.8% (Table 5)). However, the overall response rate (composite CR+PR+HI) was similar across the two arms (PAN+AZA, 37.5%; AZA, 38.1%).
For patients with MDS/CMML, the composite CR rate was higher in the PAN+AZA arm vs the control arm (29.0 vs 10.3%; Supplementary Table 2). However, the clinical response (41.9 vs 41.4%), erythroid response (25.8 vs 31.0%), platelet response (35.5 vs 24.1%) and neutrophil response (19.4 vs 13.8%) rates were similar across treatment arms. Relapse was reported in 22.6% of all patients in the PAN+AZA arm vs 17.2% in the AZA arm. Among patients with AML, the clinical response rate was 22.2% (95% CI, 2.8–60.0%) in the PAN+AZA arm and 30.8% (95% CI, 9.1–61.4%) in the control arm (Supplementary Table 3).
In the overall phase 2b population, the probability of being progression free at 12 months, based on Kaplan−Meier analysis, was similar for both treatment arms (PAN+AZA, 70% (95% CI, 40–90%); AZA, 70% (95% CI, 40–80%)). The 1-year survival rate, as computed from the Kaplan−Meier analysis of OS, was 60% (95% CI, 50–80%) in the PAN+AZA arm vs 70% (95% CI, 50–80%) in the control arm (Figure 2).
Bone marrow aspirate samples from 37 patients (45.1%) were collected for NGS, 20 from the PAN+AZA arm (7 achieved CR) and 17 from the AZA arm (0 achieved CR). The genes most often mutated in the available samples include TP53 (51.4%), a tumor suppressor gene; TET2 (29.7%), which promotes DNA methylation; and RUNX1 (24.3%), a regulator of hematopoiesis (Figure 3). However, there was no clear evidence of a relationship between mutations and disease status or response.
Next-generation sequencing analysis. Patients with next-generation sequencing (NGS) data are from phase 2b. A gene is considered to be mutant (MT) if one or more alterations, regardless of functional significance, are detected. AML, acute myeloid leukemia; AZA, azacitidine; BM-CR, bone marrow complete response; CMML, chronic myelomonocytic leukemia; CR, complete response; CRi, morphologic CR with incomplete blood count; MDS, myelodysplastic syndrome; PAN, panobinostat; WT, wild type.
Discussion
In this study, the combination of PAN+AZA did not demonstrate a substantial efficacy benefit compared with AZA alone in patients with higher-risk MDS, CMML, and AML. Additionally, patients in the PAN+AZA arm experienced a higher rate of grade 3/4 AEs. Similar results were found in phase 2 studies of vorinostat+AZA for higher-risk MDS and CMML,21 entinostat+AZA for MDS and AML,22 pracinostat+AZA for previously untreated MDS,23 and valproic acid+decitabine for MDS and AML.24, 25, 26
However, these results were not anticipated for PAN+AZA based on strong preclinical evidence supporting combined treatment with PAN and demethylating agents13 and compelling preliminary data from an uncontrolled phase 1b/2 trial examining PAN+AZA in patients with higher-risk MDS and AML.27 Results from that study by Tan et al. demonstrated an overall response rate of 31% (9/29) in patients with AML and 50% (5/10) in patients with high-risk MDS at the MTD of PAN 30 mg plus AZA 75 mg/m2. Both the previous and present studies demonstrated better clinical response in patients with MDS/CMML compared with AML. In patients with AML, PAN did not enhance the clinical benefit of AZA. In patients with MDS/CMML, the composite CR rate was nearly 3 times higher in the PAN+AZA arm (29.0% vs 10.3%). The observed safety profile in the previous study was similar to that seen in the present study, with high rates of grade 3/4 hematologic AEs including neutropenia (96.2%), thrombocytopenia (91.7%) and anemia (88.9%).
Despite improvements in composite CR rates, particularly in patients with MDS/CMML, there were no significant improvements in OS or time to progression with the addition of PAN to AZA treatment in the present study. Although a number of factors could have contributed to this outcome, the addition of PAN to AZA is unlikely to positively impact therapy for patients with AML/MDS with the treatment schedule and in a clinical setting as examined in this study. For example, patients may not have stayed on treatment long enough to improve their OS; composite CR may be a poor correlate to OS; the overall response rate, which was similar between the two arms, may have a greater influence on OS than composite CR; and the study may have been underpowered for OS. It should be noted that the proportion of patients with MDS/CMML achieving a PR or better response (17.2%) in the AZA arm of the present study appeared lower than that in the AZA arm (29%: 17% CR, 12% PR) of the pivotal phase 3 study of AZA vs conventional care in patients with MDS/CMML (AZA-001),6 potentially due to the rate of treatment discontinuation prior to the first efficacy assessment at the end of cycle 2. Similarly, a population-based analysis found shorter OS among patients receiving AZA in clinical practice compared with those receiving AZA-001.28 Another potential reason for the lack of survival benefit in the overall population could be the inherent difficulty in selecting MDS/AML patient populations likely to derive benefit. Additionally, one limitation of the study is that there was no central review or adjudication of responses.
Currently, there is no good universally accepted clinical biomarker for response to epigenetic therapy in MDS/AML. The study by Tan et al.27 demonstrated that an elevation of histone H3 and H4 levels of >50% from baseline following PAN treatment strongly correlated with clinical response. However, a number of other studies examining the correlation between acetylation levels and response have failed to show an association, potentially due to the use of less sensitive methodology.14, 29, 30 An additional limitation of exploring histone acetylation levels as a potential biomarker of response is that, while such markers are useful universal pharmacodynamic markers of class I HDAC inhibition, they do not measure the consequence of increased acetylation on tumor cells (for example, at the gene expression or cell signaling levels), and therefore cannot necessarily be expected to correlate with response. There was no clear evidence of a relationship between mutations and disease status or response. However, the lack of data for patients in the AZA arm who achieved a CR and the small sample size make it difficult to draw conclusions.
Consideration should also be given to the potential role of the sequence in which DACi and hypomethylating agents are administered. Although this was reflected in scheduling the two agents, with PAN started on day 3 of each cycle, both agents were given concurrently for a substantial part of the first week of each cycle. Results from a phase 1 study showed that concurrent administration of vorinostat and decitabine yielded better responses compared with sequential administration;31 however, PAN has been shown to induce cell cycle arrest,9 which may lead to antagonistic effects when used in combination with AZA in the present schedule. This concept is currently being evaluated in a trial of concurrent vs sequential administration of entinostat and AZA (NCT01305499). Thus, other doses and schedules of this or other HDAC inhibitors in combination with AZA should be explored.
Furthermore, tolerability of PAN+AZA may have limited the therapeutic efficacy of this combination by preventing delivery of sufficient doses of PAN in particular. Only 47.4% of patients in the combination arm received ⩾90% of the scheduled dose due to dose reductions and interruptions, which were generally AE related. This is one explanation provided for the lack of benefit of AZA plus vorinostat over AZA in the North American Intergroup Study SWOG S1117.21 Hematologic toxicity is common to both DACi and hypomethylating agents, so the potential for aggravating thrombocytopenia and neutropenia by combining these two classes of drugs was anticipated when designing the study. Even though we did not observe extremely prolonged cytopenia attributable to study drugs, hematologic toxicity was the principal reason for decreasing drug dose and interrupting or discontinuing treatment. In contrast, gastrointestinal and constitutional AEs were generally well managed and did not constitute a major management problem during the DLT-defining period, so that the number of DLTs in all dose cohorts in phase 1b was below the threshold for declaration of MTD. The overall long-term safety profile of the regimen in this study posed a challenge, with nearly all patients in the PAN+AZA arm of phase 2b (97.3%) reporting ⩾1 grade 3/4 AE vs 81.0% in the AZA arm. Common AEs (⩾50% in PAN+AZA arm) were nausea, thrombocytopenia, diarrhea, and pyrexia, consistent with the established safety profile of both drugs as single agents in patients with hematologic malignancies.6, 10, 32 Grade 3/4 AEs were primarily managed through dose reduction/interruption, leading to only moderate drug-related discontinuations. However, the observed safety profile was similar to AZA in combination with other, less potent, DACi’s.14, 29, 33, 34, 35, 36 Additionally, in phase 2b, there was a higher rate of on-treatment mortality in the PAN+AZA arm compared with the AZA arm, and the death of 2 of 5 patients in the PAN+AZA arm was suspected by the investigator to be treatment related. These results suggest that further dose and schedule optimization is warranted to improve the tolerability of the combination in this patient population. Studies have shown that higher doses of AZA are associated with increased risk of infection; thus, lower doses of AZA should be considered.37, 38
The results of this study demonstrate that the regimen of PAN 30 mg plus AZA 75 mg/m2 has an unfavorable risk/benefit profile in patients with MDS, CMML or AML, but also suggest that PAN+AZA could provide clinical benefit in select subsets of patients (for example, patients with high-risk MDS). The development of a consistent biomarker for patients with MDS/AML likely to respond to DACi could help shift the risk/benefit relationship. However, in the current therapeutic landscape, further dose and schedule optimization is warranted to improve the tolerability of the combination in this patient population. It is worth noting that at the time of data cutoff (30 April 2014), 3 patients from phase 1b and 13 patients from phase 2b (PAN+AZA (n=7); AZA (n=6)) remained on treatment, with most patients having achieved CR.
References
Garcia-Manero G . Myelodysplastic syndromes: 2015 update on diagnosis, risk-stratification and management. Am J Hematol 2015; 90: 831–841.
Nimer SD . Myelodysplastic syndromes. Blood 2008; 111: 4841–4851.
Fenaux P, Mufti GJ, Hellström-Lindberg E, Santini V, Gattermann N, Germing U et al. Azacitidine prolongs overall survival compared with conventional care regimens in elderly patients with low bone marrow blast count acute myeloid leukemia. J Clin Oncol 2010; 28: 562–569.
Dombret H, Seymour JF, Butrym A, Wierzbowska A, Selleslag D, Jang JH et al. International phase 3 study of azacitidine vs conventional care regimens in older patients with newly diagnosed AML with >30% blasts. Blood 2015; 126: 291–299.
Pleyer L, Burgstaller S, Girschikofsky M, Linkesch W, Stauder R, Pfeilstocker M et al. Azacitidine in 302 patients with WHO-defined acute myeloid leukemia: results from the Austrian azacitidine registry of the AGMT-study group. Ann Hematol 2014; 93: 1825–1838.
Fenaux P, Mufti GJ, Hellstrom-Lindberg E, Santini V, Finelli C, Giagounidis A et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher-risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol 2009; 10: 223–232.
Maurillo L, Venditti A, Spagnoli A, Gaidano G, Ferrero D, Oliva E et al. Azacitidine for the treatment of patients with acute myeloid leukemia: report of 82 patients enrolled in an Italian Compassionate Program. Cancer 2012; 118: 1014–1022.
Laubach JP, Moreau P, San-Miguel JF, Richardson PG . Panobinostat for the treatment of multiple myeloma. Clin Cancer Res 2015; 21: 4767–4773.
Atadja P . Development of the pan-DAC inhibitor panobinostat (LBH589): successes and challenges. Cancer Lett 2009; 280: 233–241.
DeAngelo DJ, Spencer A, Bhalla KN, Prince HM, Fischer T, Kindler T et al. Phase Ia/II, two-arm, open-label, dose-escalation study of oral panobinostat administered via two dosing schedules in patients with advanced hematologic malignancies. Leukemia 2013; 27: 1628–1636.
Khan H, Vale C, Bhagat T, Verma A . Role of DNA methylation in the pathogenesis and treatment of myelodysplastic syndromes. Semin Hematol 2013; 50: 16–37.
Issa JP . Epigenetic changes in the myelodysplastic syndrome. Hematol Oncol Clin North Am 2010; 24: 317–330.
Fiskus W, Buckley K, Rao R, Mandawat A, Yang Y, Joshi R et al. Panobinostat treatment depletes EZH2 and DNMT1 levels and enhances decitabine mediated de-repression of JunB and loss of survival of human acute leukemia cells. Cancer Biol Ther 2009; 8: 939–950.
Soriano AO, Yang H, Faderl S, Estrov Z, Giles F, Ravandi F et al. Safety and clinical activity of the combination of 5-azacytidine, valproic acid, and all-trans retinoic acid in acute myeloid leukemia and myelodysplastic syndrome. Blood 2007; 110: 2302–2308.
Garcia-Manero G, Kantarjian HM, Sanchez-Gonzalez B, Yang H, Rosner G, Verstovsek S et al. Phase 1/2 study of the combination of 5-aza-2'-deoxycytidine with valproic acid in patients with leukemia. Blood 2006; 108: 3271–3279.
Richardson PG, Laubach JP, Lonial S, Moreau P, Yoon SS, Hungria VT et al. Panobinostat: a novel pan-deacetylase inhibitor for the treatment of relapsed or relapsed and refractory multiple myeloma. Expert Rev Anticancer Ther 2015; 15: 737–748.
Cheson BD, Bennett JM, Kopecky KJ, Büchner T, Willman CL, Estey EH et al. Revised recommendations of the international working group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol 2003; 21: 4642–4649.
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood 2006; 108: 419–425.
Babb J, Rogatko A, Zacks S . Cancer phase I clinical trials: efficient dose escalation with overdose control. Stat Med 1998; 17: 1103–1120.
Clopper CJ, Pearson ES . The use of confidence or fiducial limits illustrated in the case of the binomial. Biometrika 1934; 26: 404–413.
Sekeres MA, Othus M, List AF, Odenike O, Stone RM, Gore SD et al. Randomized phase II study of azacitidine alone or in combination with lenalidomide or with vorinostat in higher-risk myelodysplastic syndromes and chronic myelomonocytic leukemia: North American Intergroup Study SWOG S1117. J Clin Oncol 2017; e-pub ahead of print 9 May 2017 doi:10.1200/JCO.2015.66.2510.
Prebet T, Sun Z, Figueroa ME, Ketterling R, Melnick A, Greenberg PL et al. Prolonged administration of azacitidine with or without entinostat for myelodysplastic syndrome and acute myeloid leukemia with myelodysplasia-related changes: results of the US Leukemia Intergroup trial E1905. J Clin Oncol 2014; 32: 1242–1248.
Garcia-Manero G, Berdeja JG, Komrokji RS, Essell J, Lyons RM, Maris M et al. A randomized, placebo-controlled, phase II study of pracinostat in combination with azacitidine (AZA) in patients with previously untreated myelodysplastic syndrome (MDS). Blood 2015; 126: Abstract 911.
Issa JP, Garcia-Manero G, Huang X, Cortes J, Ravandi F, Jabbour E et al. Results of phase 2 randomized study of low-dose decitabine with or without valproic acid in patients with myelodysplastic syndrome and acute myelogenous leukemia. Cancer 2015; 121: 556–561.
Lubbert M, Kuendgen A . Combining DNA methyltransferase and histone deacetylase inhibition to treat acute myeloid leukemia/myelodysplastic syndrome: achievements and challenges. Cancer 2015; 121: 498–501.
Blum W, Klisovic RB, Hackanson B, Liu Z, Liu S, Devine H et al. Phase I study of decitabine alone or in combination with valproic acid in acute myeloid leukemia. J Clin Oncol 2007; 25: 3884–3891.
Tan P, Wei A, Mithraprabhu S, Cummings N, Liu HB, Perugini M et al. Dual epigenetic targeting with panobinostat and azacitidine in acute myeloid leukemia and high-risk myelodysplastic syndrome. Blood Cancer J 2014; 4: e170.
Zeidan AM, Davidoff AJ, Long JB, Hu X, Wang R, Ma X et al. Comparative clinical effectiveness of azacitidine versus decitabine in older patients with myelodysplastic syndromes. Br J Haematol 2016; 175: 829–840.
Fandy TE, Herman JG, Kerns P, Jiemjit A, Sugar EA, Choi SH et al. Early epigenetic changes and DNA damage do not predict clinical response in an overlapping schedule of 5-azacytidine and entinostat in patients with myeloid malignancies. Blood 2009; 114: 2764–2773.
Garcia-Manero G, Yang H, Bueso-Ramos C, Ferrajoli A, Cortes J, Wierda WG et al. Phase 1 study of the histone deacetylase inhibitor vorinostat (suberoylanilide hydroxamic acid (SAHA)) in patients with advanced leukemias and myelodysplastic syndromes. Blood 2008; 111: 1060–1066.
Kirschbaum M, Gojo I, Goldberg SL, Bredeson C, Kujawski LA, Yang A et al. A phase 1 clinical trial of vorinostat in combination with decitabine in patients with acute myeloid leukaemia or myelodysplastic syndrome. Br J Haematol 2014; 167: 185–193.
Lee YG, Kim I, Yoon SS, Park S, Cheong JW, Min YH et al. Comparative analysis between azacitidine and decitabine for the treatment of myelodysplastic syndromes. Br J Haematol 2013; 161: 339–347.
Maslak P, Chanel S, Camacho LH, Soignet S, Pandolfi PP, Guernah I et al. Pilot study of combination transcriptional modulation therapy with sodium phenylbutyrate and 5-azacytidine in patients with acute myeloid leukemia or myelodysplastic syndrome. Leukemia 2006; 20: 212–217.
Gore SD, Baylin S, Sugar E, Carraway H, Miller CB, Carducci M et al. Combined DNA methyltransferase and histone deacetylase inhibition in the treatment of myeloid neoplasms. Cancer Res 2006; 66: 6361–6369.
Raffoux E, Cras A, Recher C, Boëlle PY, de Labarthe A, Turlure P et al. Phase 2 clinical trial of 5-azacitidine, valproic acid, and all-trans retinoic acid in patients with high-risk acute myeloid leukemia or myelodysplastic syndrome. Oncotarget 2010; 1: 34–42.
Garcia-Manero G, Estey EH, Jabbour E, Borthakur G, Kadia T, Naqvi K et al. Final report of a phase II study of 5-azacitidine and vorinostat in patients (pts) with newly diagnosed myelodysplastic syndrome (MDS) or acute myelogenous leukemia (AML) not eligible for clinical trials because poor performance and presence of other comorbidities. Blood 2011; 118: Abstract 608.
Merkel D, Filanovsky K, Gafter-Gvili A, Vidal L, Aviv A, Gatt ME et al. Predicting infections in high-risk patients with myelodysplastic syndrome/acute myeloid leukemia treated with azacitidine: a retrospective multicenter study. Am J Hematol 2013; 88: 130–134.
Ofran Y, Filanovsky K, Gafter-Gvili A, Vidal L, Aviv A, Gatt ME et al. Higher infection rate after 7- compared with 5-day cycle of azacitidine in patients with higher-risk myelodysplastic syndrome. Clin Lymphoma Myeloma Leuk 2015; 15: e95–e99.
Acknowledgements
This trial (NCT00946647) was sponsored by Novartis Pharmaceuticals Corporation. The authors thank Julie Shilane, PhD, and Michael Demars, PhD, of ArticulateScience LLC, for editorial writing support, which was funded by Novartis. The authors thank Antje Wegener and Florence Binlich, formerly employees of Novartis, for assistance with an earlier draft of the manuscript and Marina Mantori and Socrates Opio for operational support.
Author contributions
GG-M, DJD and OGO contributed to study design and conception, provision of study materials and patients, data collection, data analysis and interpretation, and drafting, review and final approval of the manuscript. MAS, SA, AM and LG contributed to provision of study materials and patients, data collection, data analysis and interpretation, and drafting, review and final approval of the manuscript. ME, MB, CG, JDC, HS, AI, PF, NZ, KY and J-HL contributed to provision of study materials and patients, data collection, and drafting, review and final approval of the manuscript. RS and DV contributed to provision of study materials and patients, data analysis and interpretation, and drafting, review and final approval of the manuscript. ZB contributed to provision of study materials and patients, and drafting, review and final approval of the manuscript. SI and MM contributed to data analysis and interpretation, and drafting, review and final approval of the manuscript. SA contributed to study design and conception, data collection, data analysis and interpretation, and drafting, review and final approval of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
GG-M, ME, JDC, HS, PF, NZ, J-HL, AM and ZB declare no conflict of interest; MAS has served on the board of directors/advisory committees for Celgene; MB has received honoraria from Novartis, BMS, Pfizer and Ariad; CG has received honoraria from and has served on the board of directors/advisory committees for Celgene, Novartis and Amgen; AI has served on the board of directors/advisory committees for Roche, Takeda and Janssen; DJD has held consulting and advisory roles with Ariad, BMS, Novartis, Pfizer, Incyte and Amgen; RS has received research funding and honoraria from Novartis, Celgene and Teva, has received honoraria from Hospira, and has served on the board of directors/advisory committees for Celgene; KY has served on the board of directors/advisory committees for Novartis and Celgene and has received research funding from Novartis, Celgene and Astex, and honoraria from Novartis; DV has received honoraria from and has served on the speaker's bureaus and board of directors/advisory committees for Celgene, Novartis, Amgen, Takeda and Pfizer, has held a consulting role with Celgene, has received honoraria from and served on the board of directors/advisory committees for Boehringer Ingelheim, and has received honoraria from and served on the speaker's bureau for Astellas; LG and SA are employees of Novartis; SI and MM are employees of and have equity ownership of Novartis; OGO has held a consulting role, has received research funding and honoraria from, and has served on the board of directors/advisory committees for Novartis.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Garcia-Manero, G., Sekeres, M., Egyed, M. et al. A phase 1b/2b multicenter study of oral panobinostat plus azacitidine in adults with MDS, CMML or AML with ⩽30% blasts. Leukemia 31, 2799–2806 (2017). https://doi.org/10.1038/leu.2017.159
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2017.159
This article is cited by
-
Phase 1 study of belinostat and adavosertib in patients with relapsed or refractory myeloid malignancies
Cancer Chemotherapy and Pharmacology (2023)
-
G-CSF plus azacitidine versus azacitidine alone for patients with high-risk myelodysplastic syndrome: academic, open label, randomized trial
Blood Cancer Journal (2022)
-
Recent developments in epigenetic cancer therapeutics: clinical advancement and emerging trends
Journal of Biomedical Science (2021)
-
Towards precision medicine for AML
Nature Reviews Clinical Oncology (2021)
-
Mutations in chronic myelomonocytic leukemia and their prognostic relevance
Clinical and Translational Oncology (2021)