Abstract
We conducted a cytogenetic analysis of 642 children with de novo acute myeloid leukemia (AML) treated on the AML-Berlin-Frankfurt-Münster (BFM) 04 protocol to determine the prognostic value of specific chromosomal aberrations including monosomal (MK+), complex (CK+) and hypodiploid (HK+) karyotypes, individually and in combination. Multivariate regression analysis identified in particular MK+ (n=22) as a new independent risk factor for poor event-free survival (EFS 23±9% vs 53±2% for all other patients, P=0.0003), even after exclusion of four patients with monosomy 7 (EFS 28±11%, P=0.0081). CK+ patients without MK had a better prognosis (n=47, EFS 47±8%, P=0.46) than those with MK+ (n=12, EFS 25±13%, P=0.024). HK+ (n=37, EFS 44±8% for total cohort, P=0.3) influenced outcome only when t(8;21) patients were excluded (remaining n=16, EFS 9±8%, P<0.0001). An extremely poor outcome was observed for MK+/HK+ patients (n=10, EFS 10±10%, P<0.0001). Finally, isolated trisomy 8 was also associated with low EFS (n=16, EFS 25±11%, P=0.0091). In conclusion, monosomal karyotype is a strong and independent predictor for high-risk pediatric AML. In addition, isolated trisomy 8 and hypodiploidy without t(8;21) coincide with dismal outcome. These results have important implications for risk stratification and should be further validated in independent pediatric cohorts.
Similar content being viewed by others
Introduction
In recent years, analyses of molecular and cytogenetic aberrations have revealed the heterogeneity of pediatric acute myeloid leukemia (AML),1, 2 which is now partially incorporated within the World Health Organization classification and current risk stratification systems.3, 4, 5 To date, most study groups have agreed on favorable prognostic factors such as inv(16)(p13.1q22)/CBFB-MYH11, or t(16;16)(p13.1;q22), t(8;21)(q22;q22)/RUNX1-RUNX1T1, t(15;17)/PML-RARA, single NPM1 mutations or double mutated CEBPA.1, 2, 4, 5, 6 However, conflicting data on risk factors for poor outcomes represent the highly variable definitions of high-risk AML among international study groups and reflect the urgent need to analyze potentially high-risk aberrations in large pediatric cohorts.
Monosomy 7 is a well-described unfavorable prognostic factor in pediatric and adult patients with AML.2, 7 In adult AML, a defined group of patients harboring a monosomal karyotype (MK) has been found to experience exceedingly poor outcomes.8, 9, 10, 11, 12, 13 However, in children, the predictive relevance of a MK remains unclear.14 A recent study elucidated the impact of modal numbers in pediatric AML, assuming that a hypodiploid karyotype (HK) may be related to poor outcome.15 For complex karyotype (CK), however, varying definitions exist and patients are treated heterogeneously. Even with differences in karyotype definitions, current collaborative studies mostly recommend allogeneic stem cell transplantation (HSCT) during the first complete remission (1st CR) for treatment of genetically defined high-risk patients.16 Thus, it is crucial to carefully define high-risk factors.
In this study, we evaluated correlations between genotype and outcome for defined aberrant karyotypes in a large, uniquely treated group of children with AML in the AML-Berlin-Frankfurt-Münster (BFM) 04 study and considered the results within the context of the increasing complexity of genetic aberrations.
Patients and methods
Patients
Between March 2004 and March 2012, 764 patients 0–18 years of age with de novo AML in Germany, Austria, Switzerland, and the Czech Republic (patients with Down Syndrome excluded) were treated according to the AML-BFM 04 protocol (ClinicalTrials.gov Identifier: NCT00111345). Initial diagnosis was performed according to the French-American-British (FAB) classification.17, 18, 19 Bone marrow morphology, flow cytometry and cytogenetics were centrally reviewed. National ethics committees and institutional review boards approved this study, and patients or guardians provided written informed consent. The study was performed in accordance with the Declaration of Helsinki.
Methods
Cytogenetic data were available for 701 patients (92%) and were collected and centrally reviewed as previously described.2 The descriptions of karyotypes followed the International System of Human Cytogenetic Nomenclature.20 For the following analyses, we excluded patients with t(15;17)/PML-RARA-fusion gene (probability of event-free survival (EFS) 89±4%, n=59) due to their unique biology and treatment.
Cytogenetics, fluorescence in situ hybridization (FISH) and reverse transcription polymerase chain reaction (RT-PCR) analyses were performed using standard protocols with initial bone marrow or peripheral blood samples. After short-term culture for 12–72 h, metaphases of bone marrow and/or peripheral blood were prepared according to standard procedures. Fluorescence R-banding was performed as described by Göhring et al.21 In patients with MLL-rearrangement (mixed-lineage leukemia, also called KMT2A), t(15;17)(q22;q21), t(8;21)(q22;q22) or inv(16)(p13q22)/t(16;16)(p13;q22) the molecular genetic aberrations were analyzed to confirm the cytogenetic data by FISH on interphase nuclei and by RT-PCR.21, 22 In few patients the confirmation of specific aberrations in cytogenetics was performed only by FISH or RT-PCR, and patients were added to the corresponding cytogenetic subgroup. In detail 16% of patients with MLL-rearrangement, t(15;17) or t(8;21) were confirmed by FISH only, without additional confirmation by RT-PCR. Seven percent of patients with MLL-rearrangement have been confirmed by RT-PCR only.
Analysis of the FLT3 gene (FMS-Related Tyrosine Kinase 3; OMIM No: 136351; localization: 13q12) was performed in 475 patients using PCR with 5′ end D4 WellRED dye-labeled reverse primers (Beckman Coulter, Krefeld, Germany). Samples were diluted in SLS (CEQt SLS, Beckman Coulter) containing a CEQ 600 size standard mixture (CEQt DNA Size Standard Kit, Beckman Coulter). The sizes of the resulting fragments were measured by capillary fragment analysis on a CEQ8000 genetic analysis system (Beckman Coulter). Wild-type and mutated alleles were assessed as proposed by Thiede et al.23 PCR products were subsequently sequenced using the GenomeLab Dye Terminator Cycle Sequencing with Quick Start Kit (Beckman Coulter).23, 24, 25, 26, 27, 28, 29, 30 Detailed protocols and primer sequences are available on request.
Risk classification
Risk stratification was performed as described.31 Patients with FAB M1/M2 with Auer rods or FAB M4eo or favorable cytogenetics [t(8;21)/RUNX1-RUNX1T1 or inv(16) or t(16;16) and/or CBFB/MYH11)] were assigned to the standard risk group. All other patients as well as standard risk patients with FLT3-ITD mutations or bone marrow blasts ⩾5% on day 15 were assigned to the high-risk group.
Treatment
Between March 2004 and April 2010, patients were treated according to the schedule of study AML-BFM 04, as summarized previously.31 Allogeneic HSCT from matched sibling donors was limited to high-risk patients in 1st CR, and after a 2006 amendment, allogeneic HSCT was restricted to only high-risk patients with persistent disease after second induction (bone marrow blasts >5%).32, 33 Thereafter, patients were treated according to the AML-BFM 04 protocol but not further randomized. All patients received the liposomal formulation of daunorubicin during induction therapy, and all high-risk patients received 2-chloro-2-deoxyadenosine as intensification therapy during the cytarabine/idarubicin consolidation. Furthermore only high-risk patients received high-dose cytarabine and mitoxantrone (HAM) as second induction. Randomized cranial irradiation was stopped in May 2009.33
Definitions
The remission criteria were defined according to the Cancer and Leukemia Group B criteria at the end of intensification.34 EFS was calculated as the time from diagnosis to the first event (relapse, death of any cause, failure to achieve remission or secondary malignancy) or last follow-up. Failure to achieve remission was considered an event on day 0. Overall survival (OS) was defined as the time from the date of diagnosis to the date of death from any cause or last follow-up. Death within 42 days was considered early death.
Cytogenetic definitions
MK was defined as either loss of at least two autosomes or one autosome and at least one structural abnormality excluding marker and ring chromosomes. Favorable cytogenetics were excluded. This definition was previously described by Breems et al.8 and excluded patients with only one autosomal monosomy combined with a marker chromosome but no additional aberration. For further analysis, we defined a subgroup of patients who fulfilled the MK+ criteria but had no involvement of monosomy 7 (referred to as MK+ no −7). HK was defined as <46 chromosomes. Patients with HK (HK+) were subdivided as those who fulfilled the criteria for both MK and HK (HK+/MK+) or HK+/MK−. CK was defined as previously described by von Neuhoff et al.2 by three or more aberrations, including at least one structural aberration, without favorable genetics and without MLL-rearrangement. Unbalanced translocations were counted as one abnormality. Patients with CK (CK+) were similarly separated into subgroups according to whether they also fulfilled the criteria for MK: CK+/MK+ and CK+/MK−. For further analysis, patients were analyzed regarding the number of aberrations as described by Grimwade et al.35 Therefore, we referred to the definition of Grimwade and counted an unbalanced translocation as two abnormalities, but again excluded patients with MLL-rearrangement or favorable genetics.35
In addition, we analyzed patients with MK, excluding any presence of a marker or ring chromosome and patients with marker chromosomes only, but no MK.
Aberrations in chromosome 12p were counted as abnormality independent of the breakpoint or other aberrations. For this analysis, a subgroup of patients was retrospectively defined as having a very high risk of relapse depending on the following cytogenetic criteria: inv(3)(q21q26.2)/t(3;3)(q21;q26.2), t(6;9)(p23;q34), t(7;12)(q36;p13), t(5;11)(q35.3;p15), t(9;22)(q34;q11), monosomy 7, aberrations in chromosome 12p, and MLL-rearrangement due to t(4;11)(q21;q23), t(6;11)(q27;q23) or t(10;11)(p12;q23).
Statistical analyses
Statistical analyses were performed with SAS version 9.03 (SAS Institute, Cary, NC, USA). The median follow-up was 5.6 years. The Kaplan–Meier method was applied to estimate probabilities of survival. EFS and OS were compared with the log rank test. Construction of the cumulative incidence of relapse (CIR), the cumulative incidence of nonresponse and death in continuous complete remission (CCR) was based on the Kalbfleisch and Prentice method.36 Gray’s method was used to compare cumulative incidences. The Cox proportional hazards model was used for multivariate analysis of outcomes or nonresponse and relapse. The following parameters were used for multivariate analysis: cytogenetic standard risk group, MK, monosomy 7, isolated trisomy 8, FLT3 mutation, other genetically defined high-risk factors, bone marrow day 15 and HSCT. Proportions were compared between groups using the Chi-square or Fisher’s exact test. If not further specified, we refer to the remaining patients (others than patients of the analyzed subgroup) as comparator group. For further analysis and discussion, published data from study AML-BFM 98 were included.2 The database lock for this analysis was set at first of July 2016.
Results
Prognoses among cytogenetic subgroups in the AML-BFM 04 study
The 5-year EFS of all study patients with cytogenetic data (n=701) was 55±2% compared to 49±2% in our previous study (n=457, AML-BFM 98).2 For detailed information regarding incidences, outcomes and initial data of cytogenetic aberrations see Supplementary Tables 1 and 2. If not otherwise specified, the following outcome data always refer to the remaining patients excluding patients with t(15;17) (others than patients of the analyzed subgroup) as comparator group.
Patients with favorable cytogenetic aberrations showed an excellent response to induction therapy with CR rates of 95% (t(8;21)(q22;q22)/RUNX1-RUNX1T1) and 97% (inv(16)(p13.1q22)/CBFB-MYH11) and significantly better survival rates (EFS 65±6%, P=0.028 and EFS 77±6%, P<0.0001) compared to the remaining patients of the study (Supplementary Table 2). However, the EFS of patients with t(8;21) was significantly lower compared to that of AML-BFM 98 (65±6% vs 84±5%, P=0.021) due to a temporary change in the reinduction therapy without high-dose cytarabine and mitoxantrone (HAM) in study AML-BFM 04 as described by Creutzig et al. (Supplementary Table 2).37 In contrast to our previous study, the prognosis in patients with an MLL-rearrangement was not significantly inferior to that of the remaining cohort (EFS 54±4%, P=0.91) and was significantly better than that in the AML-BFM 98 cohort (EFS 54±4% vs 34±5%, P=0.0063; Supplementary Tables 2 and 5). Patients with aberrations of chromosome 7q had a worse prognosis (EFS 21±13%, P=0.0073) than those in the AML-BFM 98 study, but only in terms of EFS (Supplementary Table 2).
This study confirmed the poor prognosis in terms of EFS and CIR associated with aberrations in 12p (EFS 24±9%, P=0.0011; CIR 53±11%, P=0.01; Supplementary Table 2).
In addition, patients with trisomy 8 had a significantly poorer outcome compared to the other patients of the study, but only if this aberration was exclusive (EFS 25±11%, P=0.0091 and OS 42±13, P=0.011). Four patients were nonresponders (25%), and seven patients relapsed (44%) (Supplementary Tables 1 and 2). On multivariate analysis, isolated trisomy 8 showed a hazard ratio (HR) of 1.98 for EFS (95% confidence interval (CI) 0.99–3.97, P=0.053; Table 3).
Patients with the retrospectively analyzed high-risk factors according to genotype (see cytogenetic definition) (13%) had a significantly lower survival (EFS 33±4%, P<0.0001 and OS 57±6%, P=0.0003) compared to other patients (Supplementary Table 2). CR was achieved by 75% of these patients. The predicted poor outcomes were confirmed retrospectively in the AML-BFM 98 data (EFS 22±7%).
For the following analyses, outcome results of all patients with cytogenetic data were used to evaluate the novel high-risk criteria in detail. If not otherwise specified, the following sections always refer to the remaining patients (others than patients of the analyzed subgroup, excluding patients with t(15;17) as comparator group.
Prognosis with novel cytogenetic high-risk criteria in the study AML-BFM 04
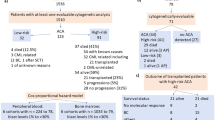
A high level of complexity based on overlapping subgroups (MK+, CK+ and HK+) was detected in our cohort (see Figure 1a; initial data in Table 1). Several patients met the definitions of more than one subgroup, and three patients fulfilled the criteria for all three definitions. Of these three patients, two experienced relapse, and one is in CCR.
Prognosis with monosomal karyotype
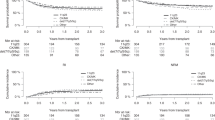
Twenty-two patients (3%) met the criteria for MK+ as defined by Breems et al. (for details on the distribution of monosomies in patients with MK, see Figure 2a and Supplementary Table 6). MK+ patients were younger (median age, 3.9 years) than the comparator group and showed significantly reduced EFS and OS compared to other patients (23±9%, P=0.0003 and 35±10%, P<0.0001, respectively; Tables 1 and 2, Figures 2b and c). Seventy-seven percent of MK+ patients achieved CR after induction therapy, but the CIR was high (46±11%, P=0.08). Multivariate analysis identified MK+ as an independent high-risk factor (EFS: HR 2.44, 95% CI 1.27–4.69, P=0.007 and nonresponse or relapse: HR 2.56, 95% CI 1.28–5.09, P=0.007; Table 3). Fourteen MK+ patients were analyzed for FLT3 mutations, and no such mutation was detected.
(a) Distribution of monosomies in patients with monosomal karyotype. n=number of monosomies; MK, monosomal karyotype. (b) EFS for patients with MK compared to patients with standard risk (SR), intermediate (MR) and other high-risk factors. (c) OS for patients with MK compared to patients with SR, intermediate risk and other high-risk factors. Definition of intermediate risk according to the AML-BFM 2012 protocol, defined as no favorable or high-risk criteria.
Monosomal karyotype and monosomy 7
Four MK+ patients also were missing chromosome 7 (Table 1). After excluding these patients, the remaining patients (labeled MK+ no −7) still experienced a poor outcome (EFS 28±11%, P=0.0081; Table 2). Although 89% of them achieved CR, their risk of relapse was high (CIR 50±13%, P=0.03; Table 2). Only two patients had an isolated monosomy 7. Both patients died after nonresponse. Overall, the seven patients with monosomy 7 showed the expected adverse outcome (EFS 14±13%, P=0.0018), with a poor response to therapy (CR 29%, P<0.001) compared to all other patients (Supplementary Table 2).
Multivariate analysis of EFS, established to distinguish MK+ no −7 patients and those with monosomy 7, identified monosomy 7 as independent prognostic factors for poor survival (monosomy 7: HR 4.53; 95% CI 1.43–14.35; P=0.01 and MK+ no −7: HR 2.08, 95% CI 0.96–4.48, P=0.062; Supplementary Table 3). This was further confirmed by Cox regression analysis of the incidence of nonresponse and relapse (Supplementary Table 3).
Monosomal and complex karyotype
Twelve patients met the criteria for MK+/CK+ and had a very poor prognosis (EFS 25±13%, P=0.024 and OS 25±13%, P=0.0001) compared to that of other patients (Table 2). The remaining MK+ patients without a CK (MK+/CK−) had a similarly unfavorable prognosis (EFS 20±13%, P=0.0029; Figure 1b and Table 2). The presence of CK did not change outcome of MK patients significantly (EFS MK+/CK− vs MK+/CK+, P=0.58). Also, the poor outcome of patients with MK was not dependent on the presence of complex aberrations according to Grimwade et al. (Supplementary Table 4).
Monosomal and hypodiploid karyotype
Ten patients who fulfilled the criteria for both MK and HK showed very poor EFS (10±10%, P<0.0001; Figure 1c) and a significantly increased CIR (70±17%, P<0.0001; Table 2) compared to other patients. The event-free survival of MK+/HK− vs MK+/HK+ was not significantly different (P=0.19). HK+ independent of MK+ did not significantly affect patients’ outcome (EFS 44±8%, P=0.30; Table 2).
Monosomal and marker chromosomes
Ten out of 22 patients with MK showed the presence of a marker chromosome, including one ring chromosome (45%). Patient with MK without any involvement of a marker chromosome still showed a very poor survival (EFS 25±13%, P=0.007 and OS 40±15, P=0.011; Table 2). The event-free survival of patients with presence of a marker chromosome but no MK was not significantly different compared to the remaining patients of the comparator group (EFS 45±10%, P=0.30 and OS 62±10%, P=0.44; Table 2).
Prognosis with complex karyotype
Fifty-nine patients (9%) were CK+ (see Table 1 for initial data), and only 3 of the 32 analyzed CK+ patients had an additional FLT3 mutation. Of note, no patient with CK+ showed a monosomy 7. Survival in CK+ patients did not differ from that of other patients (EFS 43±7%, P=0.099 and OS 58±7%, P=0.082; Table 2). After exclusion of patients with additional criteria for MK+, the remaining patients had an EFS of 47±8% (P=0.46) and OS of 68±7% (P=0.91; Table 2). An additional analysis showed that complex karyotypes with 2–3, 4–5 or >5 aberrations according to the definition of Grimwade et al. did not show significant changes in EFS, whereas patients with >5 aberrations had a reduced OS (P=0.0008) independent of the presence of MK (Supplementary Table 4).
Prognosis with hypodiploid karyotype
A HK (n=37, 6%) was frequently detected in FAB M2 patients (54%) (Table 1). HK+ associated with t(8;21) was characterized by loss of sex chromosomes (n=21, 57%). Overall, the outcomes among HK+ patients did not differ from those of other patients (EFS 44±8%, P=0.30; Table 2). As described the presence of MK significantly influenced patient’s outcome (EFS HK+/MK− vs HK+/MK+, P=0.04). In patients with t(8;21), concurrent HK did not have a significant impact on prognosis (EFS 70±10% (n=21 HK+) vs 63±7% (n=55 HK−), P=0.5) However, after exclusion of patients with t(8;21), the remaining HK+ patients had a very poor prognosis (n=16, EFS 9±8%, P<0.0001; Table 2). Six of these patients did not have concurrent MK+ and all had an event (EFS=0).
Discussion
Conflicting data from trial groups regarding the prognostic value of several cytogenetic and molecular aberrations have prevented the establishment of uniform risk-adapted therapy in pediatric AML. Accordingly, the prognostic significance of the isolated or combined occurrence of several factors such as MK, CK, HK and trisomy 8 has remained largely unclear. Our aim was to elucidate the role of potentially unfavorable risk factors in a large cohort of pediatric AML patients. So far, no pediatric study has included a clearly defined MK as a high-risk factor. In adults with AML, MK is a well-recognized adverse prognostic factor based on several large studies demonstrating the extremely poor prognosis of these patients.8, 10, 12 These studies further showed an association of MK with multidrug resistance activity and reported conflicting results regarding the possible benefit of HSCT.9, 38, 39, 40, 41 Therefore, the best risk-adapted therapeutic approach for these high-risk patients is still under debate.
In one pediatric study, Manola et al. did not detect significant differences in the initial response to induction therapy in 15 out of 244 (6%) patients with MK. However, small patient numbers and a high percentage of patients categorized as having AML with MDS-related features limited their study.14 Notably, in childhood MDS, MK is associated with a heterogeneous prognosis,42 which is in accordance with adult studies and thus creates doubt concerning the independent prognostic value of this karyotype in MDS.43, 44, 45
Here, in a much larger cohort of pediatric AML patients we identified MK as a strong and independent predictor of high-risk AML in univariate and multivariate analysis that does not require involvement of chromosome 7. These patients showed an extremely poor EFS and OS. Consistent with studies in adults, we did not detect any FLT3 mutations in our MK+ patients, but also identified a relevant overlap between MK and CK.46, 47 We included the presence of a marker chromosome that may be a result of pronounced clonal instability, even though a monosomy combined with a marker chromosome often may not be a complete monosomy. However, we excluded patients with only one autosomal monosomy combined with a marker chromosome, but no additional aberration as described by Breems et al.8 As described before in patients with MDS, 45% of our patients with MK showed the presence of a marker chromosome, which is in a range with Schanz et al.45 Of note, an additional analysis with exclusion of patients with any involvement of a marker chromosome still showed a very poor survival (EFS P=0.007 and OS P=0.011).8 The prognosis did not differ compared to the other definitions of MK in this cohort. The EFS of patients with presence of a marker chromosome but no MK was not significantly different compared to the remaining patients of the comparator group.
Patients with a CK only and no MK did not experience outcomes worse than the remaining patients. However, the better results of patients with CK in the current study must be interpreted with caution due to changes in therapy schedules. In the study AML-BFM 04, 11 CK+ patients received HCST in 1st CR, whereas in the trial AML-BFM 98, only one patient underwent transplantation. This might indicate treatment-dependent variability of this finding and should be considered in the establishment of further risk definitions.
Of note, a small subgroup of patients that fulfilled the definition of MK has been described in case reports: monosomy 7 combined with ectopic virus integration site-1 aberrations and/or abnormalities in chromosome 3q26/inv3. This karyotype seems to confer a very poor prognosis and may be associated with diabetes insipidus.48, 49, 50 One patient in our cohort had this karyotype. He showed an exceedingly complicated course, never achieving CR and dying only 6 months after diagnosis.
In our study cohort, we confirmed the incidence (6%) of hypodiploidy in pediatric AML and its association with t(8;21) and AML FAB M2 as reported by the pediatric Nordic Society of Pediatric Hematology and Oncology (NOPHO) study (incidence 8%).15 We could not verify a male predominance or an unfavorable overall prognosis for these patients (EFS 44±8%, P=0.3). However, the small subgroup of patients who fulfilled criteria for MK and HK or HK without concurrent t(8;21) were identified as having a very high risk of relapse and poor survival.
The prognostic significance of trisomy 8 in pediatric AML remains unclear. In adult AML, controversial studies have underlined the heterogeneity of this cytogenetic group.48, 49, 50 In our cohort, trisomy 8 was associated with very poor survival, but only if detected as the only cytogenetic aberration. Notably, 4 of 16 patients with trisomy 8 showed FLT3 mutations. Owing to the observed heterogeneity and conflicting data in adult AML, more pediatric studies are required to determine the prognostic impact of trisomy 8 or hypodiploidy (without t(8;21)).
In conclusion, we identified MK as a strong prognostic factor for poor outcome in pediatric AML. Isolated trisomy 8 or HK without t(8;21) are potentially predicting a dismal prognosis. In contrast, CK alone or HK did not seem to confer an adverse prognosis. Our current study protocol (AML-BFM 2012) includes cytogenetic risk factors for stratification (standard-, intermediate- and high-risk), and HSCT in 1st CR is recommended in cytogenetically and response-defined high-risk patients. Validation of these findings in independent pediatric patient cohorts will indicate that MK+ should be included as an important, novel adverse parameter in the list of high-risk criteria.
References
Harrison CJ, Hills RK, Moorman AV, Grimwade DJ, Hann I, Webb DK et al. Cytogenetics of childhood acute myeloid leukemia: United Kingdom Medical Research Council Treatment trials AML 10 and 12. J Clin Oncol 2010; 28: 2674–2681.
von Neuhoff C, Reinhardt D, Sander A, Zimmermann M, Bradtke J, Betts DR et al. Prognostic impact of specific chromosomal aberrations in a large group of pediatric patients with acute myeloid leukemia treated uniformly according to trial AML-BFM 98. J Clin Oncol 2010; 28: 2682–2689.
Campo E, Swerdlow S, Harris N, Pileri S, Stein H, Jaffe E . WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC: Lyon, France, 2008.
Pession A, Masetti R, Rizzari C, Putti MC, Casale F, Fagioli F et al. Results of the AIEOP AML 2002/01 multicenter prospective trial for the treatment of children with acute myeloid leukemia. Blood 2013; 122: 170–178.
Karol SE, Coustan-Smith E, Cao X, Shurtleff SA, Raimondi SC, Choi JK et al. Prognostic factors in children with acute myeloid leukaemia and excellent response to remission induction therapy. Br J Haematol 2015; 168: 94–101.
Creutzig U, van den Heuvel-Eibrink MM, Gibson B, Dworzak MN, Adachi S, de Bont E et al. Diagnosis and management of acute myeloid leukemia in children and adolescents: recommendations from an international expert panel. Blood 2012; 120: 3187–3205.
Hasle H, Alonzo TA, Auvrignon A, Behar C, Chang M, Creutzig U et al. Monosomy 7 and deletion 7q in children and adolescents with acute myeloid leukemia: an international retrospective study. Blood 2007; 109: 4641–4647.
Breems DA, Van Putten WL, De Greef GE, Van Zelderen-Bhola SL, Gerssen-Schoorl KB, Mellink CH et al. Monosomal karyotype in acute myeloid leukemia: a better indicator of poor prognosis than a complex karyotype. J Clin Oncol 2008; 26: 4791–4797.
Fang M, Storer B, Estey E, Othus M, Zhang L, Sandmaier BM et al. Outcome of patients with acute myeloid leukemia with monosomal karyotype who undergo hematopoietic cell transplantation. Blood 2011; 118: 1490–1494.
Voutiadou G, Papaioannou G, Gaitatzi M, Lalayanni C, Syrigou A, Vadikoliou C et al. Monosomal karyotype in acute myeloid leukemia defines a distinct subgroup within the adverse cytogenetic risk category. Cancer Genet 2013; 206: 32–36.
Kayser S, Zucknick M, Dohner K, Krauter J, Kohne CH, Horst HA et al. Monosomal karyotype in adult acute myeloid leukemia: prognostic impact and outcome after different treatment strategies. Blood 2012; 119: 551–558.
Medeiros BC, Othus M, Fang M, Roulston D, Appelbaum FR . Prognostic impact of monosomal karyotype in young adult and elderly acute myeloid leukemia: the Southwest Oncology Group (SWOG) experience. Blood 2010; 116: 2224–2228.
McQuilten ZK, Sundararajan V, Andrianopoulos N, Curtis DJ, Wood EM, Campbell LJ et al. Monosomal karyotype predicts inferior survival independently of a complex karyotype in patients with myelodysplastic syndromes. Cancer 2015; 121: 2892–2899.
Manola KN, Panitsas F, Polychronopoulou S, Daraki A, Karakosta M, Stavropoulou C et al. Cytogenetic abnormalities and monosomal karyotypes in children and adolescents with acute myeloid leukemia: correlations with clinical characteristics and outcome. Cancer Genet 2013; 206: 63–72.
Sandahl JD, Kjeldsen E, Abrahamsson J, Ha SY, Heldrup J, Jahnukainen K et al. Ploidy and clinical characteristics of childhood acute myeloid leukemia: a NOPHO-AML study. Genes Chromosomes Cancer 2014; 53: 667–675.
Hasle H . A critical review of which children with acute myeloid leukaemia need stem cell procedures. Br J Haematol 2014; 166: 23–33.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Criteria for the diagnosis of acute leukemia of megakaryocyte lineage (M7). A report of the French-American-British Cooperative Group. Ann Intern Med 1985; 103: 460–462.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med 1985; 103: 620–625.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Proposal for the recognition of minimally differentiated acute myeloid leukaemia (AML-MO). Br J Haematol 1991; 78: 325–329.
Shaffer LG, Slovak ML, Campbell LJ . An International System for Human Cytogenetic Nomenclature (2009). Recommendations of the International Standing Committee on Human Cytogenetic Nomenclature: Karger, 2009.
Gohring G, Karow A, Steinemann D, Wilkens L, Lichter P, Zeidler C et al. Chromosomal aberrations in congenital bone marrow failure disorders—an early indicator for leukemogenesis? Ann Hematol 2007; 86: 733–739.
Wilkens L, Gerr H, Gadzicki D, Kreipe H, Schlegelberger B . Standardised fluorescence in situ hybridisation in cytological and histological specimens. Virchows Arch 2005; 447: 586–592.
Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002; 99: 4326–4335.
Hovland R, Gjertsen BT, Bruserud O . Acute myelogenous leukemia with internal tandem duplication of the Flt3 gene appearing or altering at the time of relapse: a report of two cases. Leuk Lymphoma 2002; 43: 2027–2029.
Kottaridis PD, Gale RE, Langabeer SE, Frew ME, Bowen DT, Linch DC . Studies of FLT3 mutations in paired presentation and relapse samples from patients with acute myeloid leukemia: implications for the role of FLT3 mutations in leukemogenesis, minimal residual disease detection, and possible therapy with FLT3 inhibitors. Blood 2002; 100: 2393–2398.
Shih LY, Huang CF, Wu JH, Lin TL, Dunn P, Wang PN et al. Internal tandem duplication of FLT3 in relapsed acute myeloid leukemia: a comparative analysis of bone marrow samples from 108 adult patients at diagnosis and relapse. Blood 2002; 100: 2387–2392.
Schnittger S, Schoch C, Kern W, Hiddemann W, Haferlach T . FLT3 length mutations as marker for follow-up studies in acute myeloid leukaemia. Acta Haematol 2004; 112: 68–78.
Stirewalt DL, Kopecky KJ, Meshinchi S, Engel JH, Pogosova-Agadjanyan EL, Linsley J et al. Size of FLT3 internal tandem duplication has prognostic significance in patients with acute myeloid leukemia. Blood 2006; 107: 3724–3726.
Breitenbuecher F, Schnittger S, Grundler R, Markova B, Carius B, Brecht A et al. Identification of a novel type of ITD mutations located in nonjuxtamembrane domains of the FLT3 tyrosine kinase receptor. Blood 2009; 113: 4074–4077.
Kayser S, Schlenk RF, Londono MC, Breitenbuecher F, Wittke K, Du J et al. Insertion of FLT3 internal tandem duplication in the tyrosine kinase domain-1 is associated with resistance to chemotherapy and inferior outcome. Blood 2009; 114: 2386–2392.
Creutzig U, Zimmermann M, Bourquin JP, Dworzak MN, Fleischhack G, Graf N et al. Randomized trial comparing liposomal daunorubicin with idarubicin as induction for pediatric acute myeloid leukemia: results from Study AML-BFM 2004. Blood 2013; 122: 37–43.
Klusmann JH, Reinhardt D, Zimmermann M, Kremens B, Vormoor J, Dworzak M et al. The role of matched sibling donor allogeneic stem cell transplantation in pediatric high-risk acute myeloid leukemia: results from the AML-BFM 98 study. Haematologica 2012; 97: 21–29.
Creutzig U, Zimmermann M, Bourquin JP, Dworzak MN, Fleischhack G, von Neuhoff C et al. CNS irradiation in pediatric acute myleoid leukemia: equal results by 12 or 18Gy in studies AML-BFM98 and 2004. Pediatr Blood Cancer 2011; 57: 986–992.
Cheson BD, Cassileth PA, Head DR, Schiffer CA, Bennett JM, Bloomfield CD et al. Report of the National Cancer Institute-sponsored workshop on definitions of diagnosis and response in acute myeloid leukemia. J Clin Oncol 1990; 8: 813–819.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood 2010; 116: 354–365.
Kalbfleisch JD, Prentice RL . The Statistical Analysis of Failure Time Data. John Wiley & Sons: New York, NY, 2011.
Creutzig U, Zimmermann M, Bourquin JP, Dworzak MN, von Neuhoff C, Sander A et al. Second induction with high-dose cytarabine and mitoxantrone: different impact on pediatric AML patients with t(8;21) and with inv(16). Blood 2011; 118: 5409–5415.
Guo RJ, Atenafu EG, Craddock K, Chang H . Allogeneic hematopoietic cell transplantation may alleviate the negative prognostic impact of monosomal and complex karyotypes on patients with acute myeloid leukemia. Biol Blood Marrow Transplant 2014; 20: 690–695.
Deeg HJ, Scott BL, Fang M, Shulman HM, Gyurkocza B, Myerson D et al. Five-group cytogenetic risk classification, monosomal karyotype, and outcome after hematopoietic cell transplantation for MDS or acute leukemia evolving from MDS. Blood 2012; 120: 1398–1408.
Ahn HK, Jang JH, Kim K, Kim HJ, Kim SH, Jung CW et al. Monosomal karyotype in acute myeloid leukemia predicts adverse treatment outcome and associates with high functional multidrug resistance activity. Am J Hematol 2012; 87: 37–41.
Lu QS, Xu N, Zhou X, Huang JX, Li L, Li YL et al. Prognostic significance of monosomal karyotype in adult patients with acute myeloid leukemia treated with risk-adapted protocols. Clin Lymphoma Myeloma Leuk 2015; 15: 790–796.
Gohring G, Michalova K, Beverloo HB, Betts D, Harbott J, Haas OA et al. Complex karyotype newly defined: the strongest prognostic factor in advanced childhood myelodysplastic syndrome. Blood 2010; 116: 3766–3769.
Itzykson R, Thepot S, Eclache V, Quesnel B, Dreyfus F, Beyne-Rauzy O et al. Prognostic significance of monosomal karyotype in higher risk myelodysplastic syndrome treated with azacitidine. Leukemia 2011; 25: 1207–1209.
Valcarcel D, Adema V, Sole F, Ortega M, Nomdedeu B, Sanz G et al. Complex, not monosomal, karyotype is the cytogenetic marker of poorest prognosis in patients with primary myelodysplastic syndrome. J Clin Oncol 2013; 31: 916–922.
Schanz J, Tuchler H, Sole F, Mallo M, Luno E, Cervera J et al. Monosomal karyotype in MDS: explaining the poor prognosis? Leukemia 2013; 27: 1988–1995.
Weinberg OK, Ohgami RS, Ma L, Seo K, Ren L, Gotlib JR et al. Acute myeloid leukemia with monosomal karyotype: morphologic, immunophenotypic, and molecular findings. Am J Clin Pathol 2014; 142: 190–195.
Haferlach C, Alpermann T, Schnittger S, Kern W, Chromik J, Schmid C et al. Prognostic value of monosomal karyotype in comparison to complex aberrant karyotype in acute myeloid leukemia: a study on 824 cases with aberrant karyotype. Blood 2012; 119: 2122–2125.
Ma H, Yang J, Xiang B, Jia Y . Acute myeloid leukemia with monosomy 7, ectopic virus integration site-1 overexpression and central diabetes insipidus: a case report. Oncol Lett 2015; 9: 2459–2462.
Curley C, Kennedy G, Haughton A, Love A, McCarthy C, Boyd A . Acute myeloid leukemia, the 3q21q26 syndrome and diabetes insipidus: a case presentation. Asia Pac J Clin Oncol 2010; 6: 77–79.
Keung YK, Buss D, Powell BL, Pettenati M . Central diabetes insipidus and inv(3)(q21q26) and monosomy 7 in acute myeloid leukemia. Cancer Genet Cytogenet 2002; 136: 78–81.
Acknowledgements
We are grateful to patients for participation and data managers in all hospitals and offices for their efforts in this study. We thank JE Müller for data management and Laney Weber for proofreading the manuscript with regards to the language errors. This work was supported by the Deutsche Krebshilfe e.V. and partly by grant RVO-VFN64165 from the Ministry of Health of the Czech Republic.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented in part at the 47th Congress of the International Society of Paediatric Oncology, 8–11 October, 2015, Cape Town, South Africa and at Acute Leukemias XV 22–25 February, 2015, Munich and at the 21st Congress of European Hematology Association, Copenhagen, 9–12 June, 2016, Copenhagen.
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Rasche, M., von Neuhoff, C., Dworzak, M. et al. Genotype-outcome correlations in pediatric AML: the impact of a monosomal karyotype in trial AML-BFM 2004. Leukemia 31, 2807–2814 (2017). https://doi.org/10.1038/leu.2017.121
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2017.121
This article is cited by
-
The complex karyotype in hematological malignancies: a comprehensive overview by the Francophone Group of Hematological Cytogenetics (GFCH)
Leukemia (2022)
-
Cytogenetic and mutational analysis and outcome assessment of a cohort of 284 children with de novo acute myeloid leukemia reveal complex karyotype as an adverse risk factor for inferior survival
Molecular Cytogenetics (2021)
-
Acute Myeloid Leukemia in Children: Emerging Paradigms in Genetics and New Approaches to Therapy
Current Oncology Reports (2021)
-
Proportion of children with cancer that have an indication for genetic counseling and testing based on the cancer type irrespective of other features
Familial Cancer (2021)