Abstract
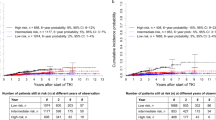
This population-based registry was designed to provide robust and updated information on the characteristics and the epidemiology of chronic myeloid leukemia (CML). All cases of newly diagnosed Philadelphia positive, BCR-ABL1+ CML that occurred in a sample of 92.5 million adults living in 20 European countries, were registered over a median period of 39 months. 94.3% of the 2904 CML patients were diagnosed in chronic phase (CP). Median age was 56 years. 55.5% of patients had comorbidities, mainly cardiovascular (41.9%). High-risk patients were 24.7% by Sokal, 10.8% by EURO, and 11.8% by EUTOS risk scores. The raw incidence increased with age from 0.39/100 000/year in people 20–29 years old to 1.52 in those >70 years old, and showed a maximum of 1.39 in Italy and a minimum of 0.69 in Poland (all countries together: 0.99). The proportion of Sokal and Euro score high-risk patients seen in many countries indicates that trial patients were not a positive selection. Thus from a clinical point of view the results of most trials can be generalized to most countries. The incidences observed among European countries did not differ substantially. The estimated number of new CML cases per year in Europe is about 6370.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Hehlmann R, Hochhaus A, Baccarani M, on behalf of the European LeukemiaNet. Chronic myeloid leukaemia. Lancet 2007; 370: 342–50.
Björkholm M, Ohm L, Eloranta S, Derolf A, Hultcrantz M, Sjöberg J et al. Success story of targeted therapy in chronic myeloid leukemia: a population-based study of patients diagnosed in Sweden from 1973 to 2008. J Clin Oncol 2011; 29: 2514–2520.
Kantarjian H, O’Brien S, Jabbour E, Garcia-Manero G, Quintas-Cardama A, Shan J et al. Improved survival in chronic myeloid leukemia since the introduction of imatinib therapy: a single-institution historical experience. Blood 2012; 119: 1981–1987.
Baccarani M, Deininger MW, Rosti G, Hochhaus A, Soverini S, Apperley JF et al. European LeukemiaNet recommendations for the management of chronic myeloid leukemia: 2013. Blood 2013; 122: 872–884.
O’Brien S, Abboud CN, Akhtari M, Altman J, Berman E, DeAngelo DJ et al. Chronic Myelogenous Leukemia, Version 1.2014. J Natl Compr Canc Netw 2013; 11: 1327–1340.
Storey S . Chronic myelogenous leukaemia market. Nat Rev Drug Discov 2009; 8: 447–448.
Huang X, Cortes J, Kantarjian H . Estimation of the increasing prevalence and plateau prevalence of chronic myeloid leukemia in the era of tyrosine kinase inhibitor therapy. Cancer 2012; 118: 3123–3127.
Experts in Chronic Myeloid Leukemia (Kantarjian H. et al.). The price of drugs for chronic myeloid leukemia (CML) is a reflection on the unsustainable prices of cancer drugs: from the perspective of a large group of CML experts. Blood 2013; 121: 4439–4442.
O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 2003; 348: 994–1004.
Cortes JE, Baccarani M, Guilhot F, Druker BJ, Branford S, Kim DW et al. Phase III, randomized, open-label study of daily imatinib mesylate 400 mg versus 800 mg in patients with newly diagnosed, previously untreated chronic myeloid leukemia in chronic phase using molecular end points: tyrosine kinase inhibitor optimization and selectivity study. J Clin Oncol 2010; 28: 424–430.
Saglio G, Kim DW, Issaragrisil S, le Coutre P, Etienne G, Lobo C et al. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med 2010; 362: 2251–2259.
Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M et al. Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med 2010; 362: 2260–2270.
Cortes JE, Kim DW, Kantarjian HM, Brümmendorf TH, Dyagil I, Griskevicius L et al. Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: results from the BELA trial. J Clin Oncol 2012; 30: 3486–3492.
Castagnetti F, Testoni N, Luatti S, Marzocchi G, Mancini M, Kerim S et al. Deletions of the derivative chromosome 9 do not influence the response and the outcome of chronic myeloid leukemia in early chronic phase treated with imatinib mesylate: GIMEMA CML Working Party analysis. J Clin Oncol 2010; 28: 2748–2754.
Gugliotta G, Castagnetti F, Palandri F, Breccia M, Intermesoli T, Capucci A et al. Frontline imatinib treatment of chronic myeloid leukemia: no impact of age on outcome, a survey by the GIMEMA CML working party. Blood 2011; 117: 5591–5599.
Preudhomme C, Guilhot J, Nicolini FE, Guerci-Bresler A, Rigal-Huguet F, Maloisel F et al. Imatinib plus peginterferon alfa-2a in chronic myeloid leukemia. N Engl J Med 2010; 363: 2511–2521.
Hehlmann R, Lauseker M, Jung-Munkwitz S, Leitner A, Müller MC, Pletsch N et al. Tolerability-adapted imatinib 800 mg/d versus 400 mg/d versus 400 mg/d plus interferon-α in newly diagnosed chronic myeloid leukemia. J Clin Oncol 2011; 29: 1634–1642.
de Lavallade H, Apperley JF, Khorashad J, Milojkovic D, Reid AG, Bua M et al. Imatinib for newly diagnosed patients with chronic myeloid leukemia: incidence of sustained responses in an intention-to-treat analysis. J Clin Oncol 2008; 26: 3358–3363.
Jain P, Kantarjian H, Nazha A, O’Brien S, Jabbour E, Romo CG et al. Early responses predict better outcomes in patients with newly diagnosed chronic myeloid leukemia: results with four tyrosine kinase inhibitor modalities. Blood 2013; 121: 4867–4874.
Hasford J, Baccarani M, Hoffmann V, Guilhot J, Saussele S, Rosti G et al. Predicting complete cytogenetic response and subsequent progression-free survival in 2060 patients with CML on imatinib treatment: the EUTOS score. Blood 2011; 118: 686–692.
Hoffmann VS, Baccarani M, Lindoerfer D, Castagnetti F, Turkina A, Zaritsky A et al. The EUTOS prognostic score: review and validation in 1288 patients with CML treated frontline with imatinib. Leukemia 2013; 27: 2016–2022.
Höglund M, Sandin F, Hellström K, Björeman M, Björkholm M, Brune M et al. Tyrosine kinase inhibitor usage, treatment outcome, and prognostic scores in CML: report from the population-based Swedish CML registry. Blood 2013; 122: 1284–1292.
Sokal JE, Cox EB, Baccarani M, Tura S, Gomez GA, Robertson JE et al. Prognostic discrimination in ‘good-risk’ chronic granulocytic leukemia. Blood 1984; 63: 789–799.
Hasford J, Pfirrmann M, Hehlmann R, Allan NC, Baccarani M, Kluin-Nelemans JC et al. A new prognostic score for survival of patients with chronic myeloid leukemia treated with interferon alfa. J Natl Cancer Inst. 1998; 90: 850–858.
Waterhouse JAH, Muir CS, Correa P, Powell J (eds). Cancer incidence in five continents. IARC: Lyon, France, 1976; 3: 456.
Fabarius A, Leitner A, Hochhaus A, Müller MC, Hanfstein B, Haferlach C et al. Impact of additional cytogenetic aberrations at diagnosis on prognosis of CML: long-term observation of 1151 patients from the randomized CML Study IV. Blood 2011; 118: 6760–6768.
Luatti S, Castagnetti F, Marzocchi G, Baldazzi C, Gugliotta G, Iacobucci I et al. Additional chromosomal abnormalities in Philadelphia-positive clone: adverse prognostic influence on frontline imatinib therapy: a GIMEMA Working Party on CML analysis. Blood 2012; 120: 761–767.
Gambacorti-Passerini C, Antolini L, Mahon FX, Guilhot F, Deininger M, Fava C et al. Multicenter independent assessment of oucomes in chronic myeloid leukemia patients treated with imatinib. J Natl Cancer Inst 2011; 103: 553–561.
McNally RJ, Rowland D, Roman E, Cartwright RA . Age and sex distribution of haematological malignancies in the UK. Hematol Oncol 1997; 15: 173–189.
Phekoo KJ, Richards MA, Moller H, Schey SA . The incidence and outcome of myeloid malignancies in 2112 adult patients in south-east England. Haematologica 2006; 91: 1400–1404.
Rohrbacher M, Berger U, Hochhaus A, Metzgeroth G, Adam K, Lahaye T et al. Clinical trials underestimate the age of chronic myeloid leukemia (CML) patients. Incidence and median age of Ph/BCR-ABL-positive CML and other chronic myeloproliferative disorders in a representative area in Germany. Leukemia 2009; 23: 602–604.
Sant M, Allemani C, Tereanu C, De Angelis R, Capocaccia R, Visser O et al. Incidence of hematologic malignancies in Europe by morphologic subtype: results of the HAEMACARE project. Blood 2010; 116: 3724–3734.
Gatta G, van der Zwan JM, Casali PG, Siesling S, Dei Tos AP, Kunkler I et al. Rare cancers are not so rare. Eur J Cancer 2011; 47: 2493–2511.
Maynadié M, Girodon F, Manivet-Janoray I, Mounier M, Mugneret F, Bailly F et al. Twenty-five years of epidemiological recording on myeloid malignancies: data from the specialized registry of hematologic malignancies of Cote d’Or (Burgundy, France). Haematologica 2011; 96: 55–61.
Osca-Gelis G, Puig-Vives M, Saez M, Gallardo D, Lloveras N, Marcos-Gragera R . Population-based incidence of myeloid malignancies: fifteen years of epidemiological data in the province of Girona, Spain. Haematologica 2013; 98: e95–e97.
Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Incidence - SEER 18 Regs Research Data, November 2013 Sub (2000–2011) <Katrina/Rita Population Adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2014, based on the November 2013 submission.
Acknowledgements
For the contribution to patients registration, data collection and follow-up we kindly acknowledge: Daniela Zackova, Brno, Hana Klamova, Prague and Jan Muzik, Brno, Czech Republic; Antonio de Vivo and Riccardo Ragionieri, Bologna, and Alessandra Cupi and Antonio Spitalieri, Catania, Italy; CM Kulikow and E Yu Chelysheva, Moscow, and Elza Lomaia, St. Petersburg, Russia; M Hoglund, Uppsala, Sweden; Luis-Felipe Casado, Toledo, and Pilar Giraldo, Zaragoza, Spain; Marzena Watek and Marek Dudzinsky, Krakow, and Witold Prejzner and Monika Szarejko, Gdansk, Poland; Florence Tartarin, Poirtiers, France; Barbara Braithwhite, Liverpool, UK; Violeta Milosevic and Olivera Markovic, Belgrade, Serbia; Tadas Zvirblis, Vilnius, Lithuania; Michael Ploetscher, Wels, Austria; Ingrida Udre, Riga, Latvia; Saara Vaalas and Minna Pajuportti, Helsinki, Finland; E Laane and Mary Punab, Tartu, Estonia; F Melanthiou and C Prokopiou, Cyprus; Yi Hao and Sandra Frank, Munich, Germany. The contribution of the investigators of other regions and countries is also acknowledged: Susanne Saussele, Mannheim, Germany; Andreas Hochhaus, Jena, Germany; Dimopoulos Panayiotidis, Athens, Greece; Tamasz Masszi, Budapest, Hungary; Antonio Medina Almeida, Lisboa, Portugal; Adriana Colita, Bucharest, Romania; Iryna Dyagil, Kyiv, Ukraina. The European Treatment and Outcome Study (EUTOS) is a project supported by Novartis Oncology Europe through a contract with European LeukemiaNet and the University of Heidelberg.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
VSH, MB, JH and DL receive research funding from Novartis. NT and ZS have a consulting or advisory role at Novartis. AC and GG are employed by Novartis. KI has a consulting or advisory role at Amgen and Novartis. BS has a consulting or advisory role at BMS. AB receives funding of travel, accommodations or expenses from Novartis Oncology, Serbia. RH receives honoraria from BMS and research funding from Novartis and BMS. SB receives honoraria from Novartis, Celgene and AOP, has a consulting or advisory role at Novartis and Celgene, and receives funding of travel, accommodations or expenses from Novartis and AOP. AGT and JM have a consulting or advisory role at Novartis and BMS, and JM receives research funding and funding of travel, accommodations or expenses from Novartis and BMS. AZ has a consulting or advisory role at and participated in a speakers’ bureau for Novartis and received research funding from BMS. LG receives research funding from Novartis and Roche and funding of travel, accommodations, or expenses from Novartis, Roche and Takeda. PK has a consulting or advisory role at GSK, BMS and Novartis, receives funding from Novartis, provides expert testimony for Pfizer and Novartis, and receives funding of travel, accommodations or expenses from BMS and Ariad. FR receives honoraria from BMS and Novartis, has a consulting or advisory role at BMS and Ariad, participated in a speakers’ bureau for BMS and Novartis, and receives research funding from BMS. AH participated in a speakers’ bureau for Novartis and BMS, receives research funding and funding of travel, accommodations or expenses from Novartis and BMS, and provides expert testimony for Novartis and BMS. FC has a consulting or advisory role and receives honoraria and funding of travel, accommodations or expenses from Novartis and BMS. TS has a consulting or advisory role at, participated in a speakers’ bureau for and receives honoraria from Novartis, BMS, ADAMED and receives research funding and funding of travel, accommodations or expenses from Novartis and BMS. JLS has a consulting or advisory role at and receives honoraria and research funding from BMS, Novartis and Pfizer, and funding of travel, accommodations or expenses from BMS and Novartis. REC participated in a speakers’ bureau for Novartis, receives funding from and has a consulting or advisory role at Novartis, BMS, Pfizer and Sanofi, and receives honoraria from Novartis, BMS, Pfizer, Sanofi and TEVA. The remaining authors declare no conflict of interests.
Rights and permissions
About this article
Cite this article
Hoffmann, V., Baccarani, M., Hasford, J. et al. The EUTOS population-based registry: incidence and clinical characteristics of 2904 CML patients in 20 European Countries. Leukemia 29, 1336–1343 (2015). https://doi.org/10.1038/leu.2015.73
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2015.73
This article is cited by
-
BCR/ABL-Positive Chronic Myeloid Leukemia in Children: Current Treatment Approach
Current Oncology Reports (2024)
-
Family Planning and Pregnancy in Patients with Chronic Myeloid Leukemia
Current Hematologic Malignancy Reports (2023)
-
Chronic myeloid leukaemia (CML) presenting in B-lymphoblastic crisis: a diagnostic challenge
Journal of Hematopathology (2023)
-
Guidelines for the treatment of chronic myeloid leukemia from the NCCN and ELN: differences and similarities
International Journal of Hematology (2023)
-
Questions concerning tyrosine kinase-inhibitor therapy and transplants in chronic phase chronic myeloid leukaemia
Leukemia (2022)