Abstract
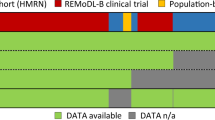
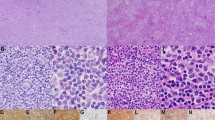
Approximately 15% of follicular lymphomas (FLs) lack breaks in the BCL2 locus. The aim of this study was to better define molecular and clinical features of BCL2-breakpoint/t(14;18)-negative FLs. We studied the presence of BCL2, BCL6 and MYC breaks by fluorescence in situ hybridization and the expression of BCL2, MUM1, CD10, P53 and Ki67 in large clinical trial cohorts of 540 advanced-stage FL cases and 116 early-stage disease FL patients treated with chemotherapy regimens and radiation, respectively. A total of 86% and 53% of advanced- and early-stage FLs were BCL2-breakpoint-positive, respectively. BCL2 was expressed in almost all FLs with BCL2 break and also in 86% and 69% of BCL2-breakpoint-negative advanced- and early-stage FLs, respectively. CD10 expression was significantly reduced in BCL2-breakpoint-negative FLs of all stages and MUM1 and Ki67 expression were significantly increased in BCL2-break-negative early-stage FLs. Patient characteristics did not differ between FLs with and without BCL2 breaks and neither did survival times in advanced-stage FLs. These results suggest that the molecular profile differs to some extent between FLs with and without BCL2 breaks and support the notion that FLs with and without BCL2 breaks belong to the same lymphoma entity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Harris NL, Swerdlow SH, Jaffe ES, Ott G. Follicular lymphoma. In: Swerdlow S, Campo E, Harris NL, Jaffe ES, Pileri S, Stein H et al. (eds). WHO Classification of Tumors of Haematopoietic and Lymphoid Tissues. IARC: Lyon, France, 2008, pp 220–226.
Fisher RI, LeBlanc M, Press OW, Maloney DG, Unger JM, Miller TP . New treatment options have changed the survival of patients with follicular lymphoma. J Clin Oncol 2005; 23: 8447–8452.
Kridel R, Sehn LH, Gascoyne RD . Pathogenesis of follicular lymphoma. J Clin Invest 2012; 122: 3424–3431.
Leich E, Salaverria I, Bea S, Zettl A, Wright G, Moreno V et al. Follicular lymphomas with and without translocation t(14;18) differ in gene expression profiles and genetic alterations. Blood 2009; 114: 826–834.
Roulland S, Kelly RS, Morgado E, Sungalee S, Solal-Celigny P, Colombat P et al. t(14;18) Translocation: a predictive blood biomarker for follicular lymphoma. J Clin Oncol 2014; 32: 1347–1355.
Sungalee S, Mamessier E, Morgado E, Gregoire E, Brohawn PZ, Morehouse CA et al. Germinal center reentries of BCL2-overexpressing B cells drive follicular lymphoma progression. J Clin Invest 2014; 124: 5337–5351.
Tellier J, Menard C, Roulland S, Martin N, Monvoisin C, Chasson L et al. Human t(14;18)positive germinal center B cells: a new step in follicular lymphoma pathogenesis? Blood 2014; 123: 3462–3465.
Weigert O, Kopp N, Lane AA, Yoda A, Dahlberg SE, Neuberg D et al. Molecular ontogeny of donor-derived follicular lymphomas occurring after hematopoietic cell transplantation. Cancer Discov 2012; Jan 2: 47–55.
Horsman DE, Okamoto I, Ludkovski O, Le N, Harder L, Gesk S et al. Follicular lymphoma lacking the t(14;18)(q32;q21): identification of two disease subtypes. Br J Haematol 2003; 120: 424–433.
Gagyi E, Balogh Z, Bodor C, Timar B, Reiniger L, Deak L et al. Somatic hypermutation of IGVH genes and aberrant somatic hypermutation in follicular lymphoma without BCL-2 gene rearrangement and expression. Haematologica 2008; 93: 1822–1828.
Leich E, Zamo A, Horn H, Haralambieva E, Puppe B, Gascoyne RD et al. MicroRNA profiles of t(14;18)-negative follicular lymphoma support a late germinal center B-cell phenotype. Blood 2011; 118: 5550–5558.
Hiddemann W, Kneba M, Dreyling M, Schmitz N, Lengfelder E, Schmits R et al. Frontline therapy with rituximab added to the combination of cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) significantly improves the outcome for patients with advanced-stage follicular lymphoma compared with therapy with CHOP alone: results of a prospective randomized study of the German Low-Grade Lymphoma Study Group. Blood 2005; 106: 3725–3732.
Koch K, Hoster E, Unterhalt M, Ott G, Rosenwald A, Hansmann ML et al. The composition of the microenvironment in follicular lymphoma is associated with the stage of the disease. Hum Pathol 2012; 43: 2274–2281.
Nickenig C, Dreyling M, Hoster E, Pfreundschuh M, Trumper L, Reiser M et al. Combined cyclophosphamide, vincristine, doxorubicin, and prednisone (CHOP) improves response rates but not survival and has lower hematologic toxicity compared with combined mitoxantrone, chlorambucil, and prednisone (MCP) in follicular and mantle cell lymphomas: results of a prospective randomized trial of the German Low-Grade Lymphoma Study Group. Cancer 2006; 107: 1014–1022.
Engelhard M, Unterhalt M, Hansmann M, Stuschke M . Follicular lymphoma: curability by radiotherapy in limited stage nodal disease? Updated results of a randomized trial. Ann Oncol 2011; 22 (Suppl 4): 90-(abstract 027).
Haralambieva E, Kleiverda K, Mason DY, Schuuring E, Kluin PM . Detection of three common translocation breakpoints in non-Hodgkin's lymphomas by fluorescence in situ hybridization on routine paraffin-embedded tissue sections. J Pathol 2002; 198: 163–170.
Ventura RA, Martin-Subero JI, Jones M, McParland J, Gesk S, Mason DY et al. FISH analysis for the detection of lymphoma-associated chromosomal abnormalities in routine paraffin-embedded tissue. J Mol Diagn 2006; 8: 141–151.
Adam P, Baumann R, Schmidt J, Bettio S, Weisel K, Bonzheim I et al. The BCL2 E17 and SP66 antibodies discriminate 2 immunophenotypically and genetically distinct subgroups of conventionally BCL2-‘negative’ grade 1/2 follicular lymphomas. Hum Pathol 2013; 44: 1817–1826.
Skinnider BF, Horsman DE, Dupuis B, Gascoyne RD . Bcl-6 and Bcl-2 protein expression in diffuse large B-cell lymphoma and follicular lymphoma: correlation with 3q27 and 18q21 chromosomal abnormalities. Hum Pathol 1999; 30: 803–808.
Vaandrager JW, Schuuring E, Raap T, Philippo K, Kleiverda K, Kluin P . Interphase FISH detection of BCL2 rearrangement in follicular lymphoma using breakpoint-flanking probes. Genes Chromosomes Cancer 2000; 27: 85–94.
Guo Y, Karube K, Kawano R, Suzumiya J, Takeshita M, Kikuchi M et al. Bcl2-negative follicular lymphomas frequently have Bcl6 translocation and/or Bcl6 or p53 expression. Pathol Int 2007; 57: 148–152.
Horn H, Schmelter C, Leich E, Salaverria I, Katzenberger T, Ott MM et al. Follicular lymphoma grade 3B is a distinct neoplasm according to cytogenetic and immunohistochemical profiles. Haematologica 2011; 96: 1327–1334.
Jardin F, Gaulard P, Buchonnet G, Contentin N, Lepretre S, Lenain P et al. Follicular lymphoma without t(14;18) and with BCL-6 rearrangement: a lymphoma subtype with distinct pathological, molecular and clinical characteristics. Leukemia 2002; 16: 2309–2317.
Marafioti T, Copie-Bergman C, Calaminici M, Paterson JC, Shende VH, Liu H et al. Another look at follicular lymphoma: immunophenotypic and molecular analyses identify distinct follicular lymphoma subgroups. Histopathology 2013; 62: 860–875.
Pasqualucci L, Khiabanian H, Fangazio M, Vasishtha M, Messina M, Holmes AB et al. Genetics of follicular lymphoma transformation. Cell Rep 2014; 6: 130–140.
Dave SS, Wright G, Tan B, Rosenwald A, Gascoyne RD, Chan WC et al. Prediction of survival in follicular lymphoma based on molecular features of tumor-infiltrating immune cells. N Engl J Med 2004; 351: 2159–2169.
Nickenig C, Dreyling M, Hoster E, Pfreundschuh M, Trumper L, Reiser M et al. Combined cyclophosphamide, vincristine, doxorubicin, and prednisone (CHOP) improves response rates but not survival and has lower hematologic toxicity compared with combined mitoxantrone, chlorambucil, and prednisone (MCP) in follicular and mantle cell lymphomas: results of a prospective randomized trial of the German Low-Grade Lymphoma Study Group. Cancer. 2006; 107: 1014–1022.
Katzenberger T, Kalla J, Leich E, Stocklein H, Hartmann E, Barnickel S et al. A distinctive subtype of t(14;18)-negative nodal follicular non-Hodgkin lymphoma characterized by a predominantly diffuse growth pattern and deletions in the chromosomal region 1p36. Blood 2009; 113: 1053–1061.
Pham-Ledard A, Cowppli-Bony A, Doussau A, Prochazkova-Carlotti M, Laharanne E, Jouary T et al. Diagnostic and prognostic value of BCL2 rearrangement in 53 patients with follicular lymphoma presenting as primary skin lesions. Am J Clin Pathol 2015; 143: 362–373.
Masir N, Campbell LJ, Goff LK, Jones M, Marafioti T, Cordell J et al. BCL2 protein expression in follicular lymphomas with t(14;18) chromosomal translocations. Br J Haematol 2009; 144: 716–725.
Acknowledgements
GO, HH and AS were supported by the Robert-Bosch-Stiftung (Stuttgart, Germany) and the German José Carreras Leukemia Foundation (München, Germany) grant DJCLS R 10/28. We thank all members of the German Low Grade Lymphoma Study Group (GLSG) who are not co-authors of this study as well as Theodora Nedeva, Heike Brückner, Eva Bachmann, Olivera Batic and Claudia Becher and Reina Zühlke-Jenisch for technical assistance.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Leich, E., Hoster, E., Wartenberg, M. et al. Similar clinical features in follicular lymphomas with and without breaks in the BCL2 locus. Leukemia 30, 854–860 (2016). https://doi.org/10.1038/leu.2015.330
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2015.330
This article is cited by
-
Novel insights into the pathogenesis of follicular lymphoma by molecular profiling of localized and systemic disease forms
Leukemia (2023)
-
EBV-positive follicular lymphoma and concurrent EBV-negative diffuse large B-cell lymphoma illustrating branched evolution model and “Hit and Run” hypothesis
Journal of Hematopathology (2022)
-
How we treat mature B-cell neoplasms (indolent B-cell lymphomas)
Journal of Hematology & Oncology (2021)
-
Distinct genetic changes reveal evolutionary history and heterogeneous molecular grade of DLBCL with MYC/BCL2 double-hit
Leukemia (2020)
-
Follicular lymphoma
Nature Reviews Disease Primers (2019)