Abstract
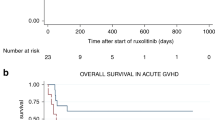
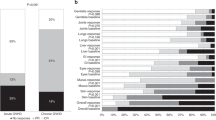
Despite major improvements in allogeneic hematopoietic cell transplantation over the past decades, corticosteroid-refractory (SR) acute (a) and chronic (c) graft-versus-host disease (GVHD) cause high mortality. Preclinical evidence indicates the potent anti-inflammatory properties of the JAK1/2 inhibitor ruxolitinib. In this retrospective survey, 19 stem cell transplant centers in Europe and the United States reported outcome data from 95 patients who had received ruxolitinib as salvage therapy for SR-GVHD. Patients were classified as having SR-aGVHD (n=54, all grades III or IV) or SR-cGVHD (n=41, all moderate or severe). The median number of previous GVHD-therapies was 3 for both SR-aGVHD (1–7) and SR-cGVHD (1–10). The overall response rate was 81.5% (44/54) in SR-aGVHD including 25 complete responses (46.3%), while for SR-cGVHD the ORR was 85.4% (35/41). Of those patients responding to ruxolitinib, the rate of GVHD-relapse was 6.8% (3/44) and 5.7% (2/35) for SR-aGVHD and SR-cGVHD, respectively. The 6-month-survival was 79% (67.3–90.7%, 95% confidence interval (CI)) and 97.4% (92.3–100%, 95% CI) for SR-aGVHD and SR-cGVHD, respectively. Cytopenia and cytomegalovirus-reactivation were observed during ruxolitinib treatment in both SR-aGVHD (30/54, 55.6% and 18/54, 33.3%) and SR-cGVHD (7/41, 17.1% and 6/41, 14.6%) patients. Ruxolitinib may constitute a promising new treatment option for SR-aGVHD and SR-cGVHD that should be validated in a prospective trial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
MacMillan ML, DeFor TE, Weisdorf DJ . The best endpoint for acute GVHD treatment trials. Blood 2010; 115: 5412–5417.
Westin JR, Saliba RM, De Lima M, Alousi A, Hosing C, Qazilbash MH et al. Steroid-refractory acute GVHD: predictors and outcomes. Adv Hematol 2011; 2011: 601953–601953.
Martin P, Rizzo JD, Wingard JR, Ballen K, Curtin PT, Cutler C et al. First- and second-line systemic treatment of acute graft-versus-host disease: recommendations of the American Society of Blood and Marrow Transplantation. Biol Blood Marrow Transplant 2012; 18: 1150–1163.
Socié G, Ritz J . Current issues in chronic graft-versus-host disease. Blood 2014; 124: 374–384.
Wolff D, Ayuk F, Elmaagacli A, Bertz H, Lawitschka A, Schleuning M et al. Current practice in diagnosis and treatment of acute graft-versus-host disease: results from a survey among German-Austrian-Swiss hematopoietic stem cell transplant centers. Biol Blood Marrow Transplant 2013; 19: 767–776.
Koreth J, Matsuoka K, Kim HT, McDonough SM, Bindra B, Alyea EP et al. Interleukin-2 and regulatory T cells in graft-versus-host disease. N Engl J Med 2011; 365: 2055–2066.
Greinix HT, Worel N, Just U, Knobler R . Extracorporeal photopheresis in acute and chronic graft-versus-host disease. Transfus Apher Sci 2014; 50: 349–357.
Harrison C, Kiladjian JJ, Al-Ali HK, Gisslinger H, Waltzman R, Stalbovskaya V et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med 2012; 366: 787–798.
Spoerl S, Mathew NR, Bscheider M, Schmitt-Graeff A, Chen S, Mueller T et al. Activity of therapeutic JAK 1/2 blockade in graft-versus-host disease. Blood 2014; 123: 3832–3842.
He YW, Adkins B, Furse RK, Malek TR . Expression and function of the gamma c subunit of the IL-2, IL-4, and IL-7 receptors. Distinct interaction of gamma c in the IL-4 receptor. J Immunol 1995; 154: 1596–1606.
Hechinger AK, Smith BA, Flynn R, Hanke K, McDonald-Hyman C, Taylor PA et al. Therapeutic activity of multiple common gamma chain cytokine inhibition in acute and chronic GVHD. Blood 2015; 125: 570–580.
Nicholson SE, Oates AC, Harpur AG, Ziemiecki A, Wilks AF, Layton JE . Tyrosine kinase JAK1 is associated with the granulocyte-colony-stimulating factor receptor and both become tyrosine-phosphorylated after receptor activation. PNAS 1994; 91: 2985–2988.
Schwab L, Goroncy L, Palaniyandi S, Gautam S, Triantafyllopoulou A, Mocsai A et al. Neutrophil granulocytes recruited upon translocation of intestinal bacteria enhance GVHD via tissue damage. Nat Med 2014; 20: 648–654.
Giroux M, Delisle JS, Gauthier SD, Heinonen KM, Hinsinger J, Houde B et al. SMAD3 prevents graft-versus-host disease by restraining Th1 differentiation and granulocyte-mediated tissue damage. Blood 2011; 117: 1734–1744.
Heine A, Held SA, Daecke SN, Wallner S, Yajnanarayana SP, Kurts C et al. The JAK-inhibitor ruxolitinib impairs dendritic cell function in vitro and in vivo. Blood 2013; 122: 1192–1202.
Kremer J, Li ZG, Hall S, Fleischmann R, Genovese M, Martin-Mola E et al. Tofacitinib in combination with nonbiologic disease-modifying antirheumatic drugs in patients with active rheumatoid arthritis: a randomized trial. Ann Intern Med 2013; 159: 253–261.
Sandborn WJ, Ghosh S, Panes J, Vranic I, Su C, Rousell S et al. Tofacitinib, an oral Janus kinase inhibitor, in active ulcerative colitis. N Engl J Med 2012; 367: 616–624.
Lerner K, Kao GF, Storb R, Buckner CD, Clift RA, Thomas ED . Histopathology of graft-vs.-host reaction (GvHR) in human recipients of marrow from HL-A-matched sibling donors. Transplant Proc 1974; 6: 367–371.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transplant 2005; 11: 945–956.
Greinix HT, Volc-Platzer B, Kalhs P, Fischer G, Rosenmayr A, Keil F et al. Extracorporeal photochemotherapy in the treatment of severe steroid-refractory acute graft-versus-host disease: a pilot study. Blood 2000; 96: 2426–2431.
Cutler C, Miklos D, Kim HT, Treister N, Woo SB, Bienfang D et al. Rituximab for steroid-refractory chronic graft-versus-host disease. Blood 2006; 108: 756–762.
Flynn R, Du J, Veenstra RG, Reichenbach DK, Panoskaltsis-Mortari A, Taylor PA et al. Increased T follicular helper cells and germinal center B cells are required for chronic GVHD (cGVHD) and bronchiolitis obliterans. Blood 2014; 123: 3988–3998.
Gooley TA, Leisenring W, Crowley J, Storer BE . Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 1999; 18: 695–706.
Verstovsek S, Mesa RA, Gotlib J, Levy RS, Gupta V, DiPersio JF et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med 2012; 366: 799–807.
Benito AI, Furlong T, Martin PJ, Anasetti C, Appelbaum FR, Doney K et al. Sirolimus (rapamycin) for the treatment of steroid-refractory acute graft-versus-host disease. Transplantation 2001; 72: 1924–1929.
Ghez D, Rubio MT, Maillard N, Suarez F, Chandesris MO, Delarue R et al. Rapamycin for refractory acute graft-versus-host disease. Transplantation 2009; 88: 1081–1087.
Hoda D, Pidala J, Salgado-Vila N, Kim J, Perkins J, Bookout R et al. Sirolimus for treatment of steroid-refractory acute graft-versus-host disease. Bone Marrow Transplant 2010; 45: 1347–1351.
Furlong T, Martin P, Flowers ME, Carnevale-Schianca F, Yatscoff R, Chauncey T et al. Therapy with mycophenolate mofetil for refractory acute and chronic GVHD. Bone Marrow Transplant 2009; 44: 739–748.
Kim JG, Sohn SK, Kim DH, Lee NY, Suh J, Lee KS et al. Different efficacy of mycophenolate mofetil as salvage treatment for acute and chronic GVHD after allogeneic stem cell transplant. Eur J Haematol 2004; 73: 56–61.
Greinix HT, Knobler RM, Worel N, Schneider B, Schneeberger A, Hoecker P et al. The effect of intensified extracorporeal photochemotherapy on long-term survival in patients with severe acute graft-versus-host disease. Haematologica 2006; 91: 405–408.
Perfetti P, Carlier P, Strada P, Gualandi F, Occhini D, Van Lint MT et al. Extracorporeal photopheresis for the treatment of steroid refractory acute GVHD. Bone Marrow Transplant 2008; 42: 609–617.
Berger M, Albiani R, Sini B, Fagioli F . Extracorporeal photopheresis for graft-versus-host disease: the role of patient, transplant, and classification criteria and hematologic values on outcome-results from a large single-center study. Transfusion 2014; e-pub ahead of print 29 October 2014 doi:10.1111/trf.12900.
Hautmann AH, Wolff D, Hahn J, Edinger M, Schirmer N, Ammer J et al. Extracorporeal photopheresis in 62 patients with acute and chronic GVHD: results of treatment with the COBE Spectra System. Bone Marrow Transplant 2013; 48: 439–445.
Busca A, Locatelli F, Marmont F, Ceretto C, Falda M et al. Recombinant human soluble tumor necrosis factor receptor fusion protein as treatment for steroid refractory graft-versus-host disease following allogeneic hematopoietic stem cell transplantation. Am J Hematol 2007; 82: 45–52.
Arai S, Margolis J, Zahurak M, Anders V, Vogelsang GB . Poor outcome in steroid-refractory graft-versus-host disease with antithymocyte globulin treatment. Biol Blood Marrow Transplant 2002; 8: 155–160.
Ballesteros M, Ferra C, Serrano D, Batlle M, Ribera JM, Díez-Martín JL . Antithymocyte globulin therapy for steroid-resistant acute graft versus host disease. Am J Hematol 2008; 83: 824–825.
Van Lint MT, Milone G, Leotta S, Uderzo C, Scimè R, Dallorso S et al. Treatment of acute graft-versus-host disease with prednisolone: significant survival advantage for day +5 responders and no advantage for nonresponders receiving anti-thymocyte globulin. Blood 2006; 107: 4177–4181.
Schnitzler M, Hasskarl J, Egger M, Bertz H, Finke J . Successful treatment of severe acute intestinal graft-versus-host resistant to systemic and topical steroids with alemtuzumab. Biol Blood Marrow Transplant 2009; 15: 910–918.
Schub N, Gunther A, Schrauder A, Claviez A, Ehlert C, Gramatzki M et al. Therapy of steroid-refractory acute GVHD with CD52 antibody alemtuzumab is effective. Bone Marrow Transplant 2011; 46: 143–147.
de Lavallade H, Mohty M, Faucher C, Fürst S, El-Cheikh J, Blaise D . Low-dose methotrexate as salvage therapy for refractory graft-versus-host disease after reduced-intensity conditioning allogeneic stem cell transplantation. Haematologica 2006; 91: 1438–1440.
MacMillan MLW, Davies SM, DeFor TE, Burns LJ, Ramsay NK et al. Early antithymothyte globulin therapy improves survival in patients with steroid-resistant acute graft-versus-host disease. Biol Blood Marrow Transplant 2002; 8: 40–46.
Rager A, Frey N, Goldstein SC, Reshef R, Hexner EO, Loren A et al. Inflammatory cytokine inhibition with combination daclizumab and infliximab for steroid-refractory acute GVHD. Bone Marrow Transplant 2011; 46: 430–435.
Martínez C, Solano C, Ferrá C, Sampol A, Valcárcel D, Pérez-Simón JA . Alemtuzumab as treatment of steroid-refractory acute graft-versus-host disease: results of a phase II study. Biol Blood Marrow Transplant 2009; 15: 639–642.
Mielke S, Lutz M, Schmidhuber J, Kapp M, Ditz D, Ammer J et al. Salvage therapy with everolimus reduces the severity of treatment-refractory chronic GVHD without impairing disease control: a dual center retrospective analysis. Bone Marrow Transplant 2014; 49: 1412–1418.
Dean RM, Fry T, Mackall C, Steinberg SM, Hakim F, Fowler D et al. Association of serum interleukin-7 levels with the development of acute graft-versus-host disease. J Clin Oncol 2008; 26: 5735–5741.
Thiant S, Labalette M, Trauet J, Coiteux V, de Berranger E, Dessaint JP et al. Plasma levels of IL-7 and IL-15 after reduced intensity conditioned allo-SCT and relationship to acute GVHD. Bone Marrow Transplant 2011; 46: 1374–1381.
Bucher C, Koch L, Vogtenhuber C, Goren E, Munger M, Panoskaltsis-Mortari A et al. IL-21 blockade reduces graft-versus-host disease mortality by supporting inducible T regulatory cell generation. Blood 2009; 114: 5375–5384.
Onishi C, Ohashi K, Sawada T, Nakano M, Kobayashi T, Yamashita T et al. A high risk of life-threatening infectious complications in mycophenolate mofetil treatment for acute or chronic graft-versus-host disease. Int J Hematol 2010; 91: 464–470.
Poi MJ, Hofmeister CC, Johnston JS, Edwards RB, Jansak BS, Lucas DM et al. Standard pentostatin dose reductions in renal insufficiency are not adequate: selected patients with steroid-refractory acute graft-versus-host disease. Clin Pharmacokinet 2013; 52: 705–712.
Gor D, Sabin C, Prentice HG, Vyas N, Man S, Griffiths PD et al. Longitudinal fluctuations in cytomegalovirus load in bone marrow transplant patients: relationship between peak virus load, donor/recipient serostatus, acute GVHD and CMV disease. Bone Marrow Transplant 1998; 21: 597–605.
Te Boome LC, Mansilla C, van der Wagen LE, Lindemans CA, Petersen EJ, Spierings E et al. Biomarker profiling of steroid-resistant acute GVHD in patients after infusion of mesenchymal stromal cells. Leukemia 2015; e-pub ahead of print 3 April 2015 doi:10.1038/leu.2015.89.
Acknowledgements
DFG (RZ, ZE872/3-1), NIH (BRB, P01 CA142106), German José Carreras Leukemia Foundation (AN, AH06-01), DKTK (RZ, NVB).
Author contributions
Authors contributed patient data and reviewed the manuscript. ASG analyzed the histopathology of the intestinal GVHD patient that was treated with ruxolitinib and provided the images. JD, RF and BRB contributed the data on murine cGVHD. GI helped the statistical analysis of the study. RZ and NVB analyzed the data and wrote the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
FA, UH, CS, GB, JK, NK, NVB: Research support from Novartis, Bristol Meyer Squibb. DW: grants and personal fees from Novartis. RZ: Speakers fee from Bristol Meyer Squibb, travel grant from Gilead. All grants from Novartis were outside/unrelated to the submitted work. The other authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Rights and permissions
About this article
Cite this article
Zeiser, R., Burchert, A., Lengerke, C. et al. Ruxolitinib in corticosteroid-refractory graft-versus-host disease after allogeneic stem cell transplantation: a multicenter survey. Leukemia 29, 2062–2068 (2015). https://doi.org/10.1038/leu.2015.212
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2015.212
This article is cited by
-
Real-world experience with ruxolitinib therapy for steroid-refractory acute graft versus host disease
Bone Marrow Transplantation (2024)
-
ROCK1/2 signaling contributes to corticosteroid-refractory acute graft-versus-host disease
Nature Communications (2024)
-
Extracorporeal photopheresis (ECP) improves overall survival in the treatment of steroid refractory acute graft-versus-host disease (SR aGvHD)
Bone Marrow Transplantation (2023)
-
Acute graft-versus-host disease
Nature Reviews Disease Primers (2023)
-
The JAK1/2 inhibitor ruxolitinib in patients with COVID-19 triggered hyperinflammation: the RuxCoFlam trial
Leukemia (2023)