Abstract
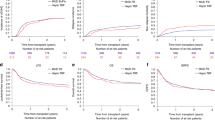
The use of unmanipulated graft is increasingly adopted in the setting of allogeneic hematopoietic stem cell transplantation from haploidentical family donors (haplo-SCT) in acute leukemia (AL). We analyzed the outcome of 229 adult patients with de novo AL, who received an unmanipulated haploidentical transplant as their first allo-SCT between 2007 and 2011. Median follow-up was 30 months. Disease status at transplant was: first complete remission (CR1) for 77, second CR (CR2) for 56, and advanced for 96 patients. One hundred and seventy-one patients received in vivo T-cell depletion by monoclonal antibodies (75%). The 60-day cumulative incidence (CI) of engraftment was 93±2%. The 100-day CI of acute graft-versus-host disease (GvHD) was 32±3% for grade II–IV, 12±3% for grade III–IV. The 3-year CI of chronic GvHD was 34±3%. The 3-year CI of non-relapse mortality was 31±4% with in vivo T-cell depletion and 17±5% without. At 3 years, for patients transplanted in CR1, CR2 or advanced disease leukemia-free survival was 44±6, 42±7 and 12±3%, overall survival was 55±6, 51±7 and 14±4% and CI of relapse was 32±6, 24±6 and 61±5%, respectively. These data suggest that unmanipulated haplo-SCT is a valid treatment option for adult AL patients in complete remission lacking a matched donor.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Mrozek K, Marcucci G, Nicolet D, Maharry KS, Becker H, Whitman SP et al. Prognostic significance of the European LeukemiaNet standardized system for reporting cytogenetic and molecular alterations in adults with acute myeloid leukemia. J Clin Oncol 2012; 30: 4515–4523.
Ballen KK, Spitzer TR . The great debate: haploidentical or cord blood transplant. Bone Marrow Transplant 2011; 46: 323–329.
Beatty PG, Clift RA, Mickelson EM, Nisperos BB, Flournoy N, Martin PJ et al. Marrow transplantation from related donors other than HLA-identical siblings. N Engl J Med 1985; 313: 765–771.
Anasetti C, Amos D, Beatty PG, Appelbaum FR, Bensinger W, Buckner CD et al. Effect of HLA compatibility on engraftment of bone marrow transplants in patients with leukemia or lymphoma. N Engl J Med 1989; 320: 197–204.
O’Reilly RJ, Kernan NA, Cunningham I . Allogeneic transplants depleted of T cells by soybean lectin agglutination and E-rosette depletion. Bone Marrow Transplant 1988; 3: 3–6.
Aversa F, Tabilio A, Terenzi A, Velardi A, Falzetti F, Giannoni C et al. Successful engraftment of T-cell depleted haploidentical three loci incompatible transplants in leukemia patients by addition of recombinant human granulocyte colony stimulating factor mobilized peripheral blood progenitor cells to bone marrow inoculum. Blood 1994; 84: 3948–3955.
Aversa F, Tabilio A, Velardi A, Cunningham I, Terenzi A, Falzetti F et al. Treatment of high-risk acute leukemia with T-cell-depleted stem cells from related donors with one fully mismatched HLA haplotype. N Engl J Med 1998; 339: 1186–1193.
Aversa F, Terenzi A, Carotti A, Felicini R, Jacucci R, Zei T et al. Improved outcome with T-cell-depleted bone marrow transplantation for acute leukemia. J Clin Oncol 1999; 17: 1545–1550.
Ciceri F, Labopin M, Aversa F, Rowe JM, Bunjes D, Lewalle P et al. A survey of fully haploidentical hematopoietic stem cell transplantation in adults with high-risk acute leukemia: a risk factor analysis of outcomes for patients in remission at transplantation. Blood 2008; 112: 3574–3581.
Champlin R, Hesdorffer C, Lowenberg B, Martelli MF, Mertelsmann RH, Reisner Y et al. Haploidentical 'megadose' stem cell transplantation in acute leukaemia: recommendations for a protocol agreed upon at the Perugia and Chicago meetings. Leukemia 2002; 16: 427–428.
Waller EK, Giver CR, Rosenthal H, Somani J, Langston AA, Lonial S et al. Facilitating T-cell immune reconstitution after haploidentical transplantation in adults. Blood Cells Mol Dis 2004; 33: 233–237.
Aversa F, Terenzi A, Tabilio A, Falzetti F, Carotti A, Ballanti S et al. Full haplotype-mismatched hematopoietic stem-cell transplantation: a phase II study in patients with acute leukaemia at high risk of relapse. J Clin Oncol 2005; 23: 3447–3454.
Ciceri F, Bonini C, Stanghellini MT, Bondanza A, Traversari C, Salomoni M et al. Infusion of suicide-gene-engineered donor lymphocytes after family haploidentical stem-cell transplantation for leukemia (the TK007 trial): a non-randomised phase I-II study. Lancet Oncol 2009; 10: 489–500.
Ji SQ, Chen HR, Wang HX, Yan HM, Zhu L, Liu J et al. G-CSF-primed haploidentical marrow transplantation without ex vivo T cell depletion: an excellent alternative for high-risk leukemia. Bone Marrow Transplant 2002; 30: 861–866.
Lee KH, Lee JH, Kim DY, Kim SH, Shin HJ, Lee YS et al. Hematopoietic cell transplantation from an HLA-mismatched familial donor is feasible without ex-vivo T-cell depletion after reduced-intensity conditioning with busulfan, fludarabine and antithymocyte globulin. Biol Blood Marrow Transplant 2009; 15: 61–72.
Lu DP, Dong L, Wu T, Huang XJ, Zhang MJ, Han W et al. Conditioning including antithymocyte globulin followed by unmanipulated HLA-mismatched/haploidentical blood and marrow transplantation can achieve comparable outcomes with HLA-identical sibling transplantation. Blood 2006; 107: 3065–3073.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant 2008; 14: 641–650.
Raiola AM, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood and Marrow Transplant 2013; 19: 117–122.
Di Bartolomeo P, Santarone S, De Angelis G, Picardi A, Cudillo L, Cerretti R et al. Haploidentical, unmanipulated, G-CSF-primed bone marrow transplantation for patients with high-risk hematologic malignancies. Blood 2013; 121: 849–857.
Peccatori J, Forcina A, Clerici D, Crocchiolo R, Vago L, Stanghellini MTL et al. Sirolimus-based graft-versus-host disease prophylaxis promotes the in vivo expansion of regulatory T cells and permits peripheral blood stem cell transplantation from haploidentical donors. Leukemia 2014; e-pub ahead of print 4 June 2014; doi:10.1038/leu.2014.180.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al. 1994 consensus conference on AGvHD grading. Bone Marrow Transplant 1995; 15: 825–828.
Lee SJ, Vogelsang G, Flowers ME . Chronic graft versus host disease. Biol Blood Marrow Transplant 2003; 9: 215–233.
Kaplan EL, Meier P . Non-parametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Gooley TA, Leisenring W, Crowley J, Storer BE . Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 1999; 18: 695–706.
Mantel N . Evaluation of survival data and two new rank order statitics arising in its consideration. Cancer Chemother Rep 1996; 503: 163–170.
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Cox DR . Regression models and life tables. J R Stat Soc 1972; 34: 187–202.
Döhner H, Estey EH, Amadori S, Appelbaum FR, Büchner T, Burnett AK et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 2010; 115: 453–474.
Rowe JM . Prognostic factors in adult acute lymphoblastic leukemia. Br J Haematol 2010; 150: 389–405.
Ringdén O, Labopin M, Ehninger G, Niederwieser D, Olsson R, Basara N et al. Reduced intensity conditioning compared with myeloablative conditioning using unrelated donor transplants in patients with acute myeloid leukemia. J Clin Oncol 2009; 27: 4570–4577.
Saber W, Opie S, Rizzo JD, Zhang MJ, Horowitz MM, Schriber J . Outcomes after matched unrelated donor versus identical sibling hematopoietic cell transplantation in adults with acute myelogenous leukemia. Blood 2012; 119: 3908–3916.
Szydlo R, Goldman JM, Klein JP, Gale RP, Ash RC, Bach FH et al. Results of allogeneic bone marrow transplants for leukemia using donors other than HLA-identical sibling. J Clin Oncol 1997; 15: 1767–1777.
Gorin NC, Labopin M, Rocha V, Arcese W, Beksac M, Gluckman E et al. Marrow versus peripheral blood for geno-identical allogeneic stem cell transplantation in acute myelocitic leukemia: influence of dose and stem cell source shows better outcome with rich marrow. Blood 2003; 102: 3043–3051.
Flower ME, Inamoto Y, Carpenter PA, Lee SJ, Kiem HP, Petersdorf EW et al. Comparative analysis of risk factors for acute graft-versus-host disease Institutes of Health consensus criteria and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood 2011; 117: 3214–3219.
Jagasia M, Arora M, Flowers ME, Chao NJ, McCarthy PL, Cutler CS et al. Risk factors for acute GVHD and survival after hematopoietic cell transplantation. Blood 2012; 119: 296–307.
Luznik L, O’Donnel PV, Fuchs JE . Post-transplantation cyclophosphamide for tolerance induction in HLA-haploidentical BMT. Semin Oncol 2012; 39: 1–16.
Rizzieri DA, Koh LP, Long GD, Gasparetto C, Sullivan KM, Horwitz M et al. Partially matched, nonmyeloablative allogeneic transplantation: clinical outcomes and immune reconstitution. J Clin Oncol 2007; 25: 690–697.
van Rood JJ, Loberiza FR Jr, Zhang MJ, Oudshoorn M, Claas F, Cairo MS et al. Effect of tolerance to non-inherited maternal antigens on the occurrence of graft-versus-host disease after bone marrow transplantation from a parent or an HLA-haploidentical sibling. Blood 2002; 99: 1572–1577.
Wang Y, Chang Y-J, Xu L-P, Liu K-Y, Liu D-H, Zhang X-H et al. Who is the best donor for a related HLA- haplotype-mismatched transplant? Blood 2014; 124: 843–850.
Wang Y, Liu D-H, Liu K-Y, Xu L-P, Zhang X-H, Han W et al. Long-term follow-up of haploidentical hematopoietic stem cell transplantation without in vitro T cell depletion for the treatment of leukemia. Cancer 2013; 119: 978–985.
Kasamon YL, Luznik L, Leffell MS, Kowalski J, Tsai HL, Bolaños-Meade J et al. Nonmyeloablative HLA-haploidentical BMT with high-dose postransplantation cyclophosphamide: effect of HLA disparity on outcome. Biol Blood Marrow Transplant 2010; 16: 482–489.
Brunstein CG, Fuchs EJ, Carter SJ, Karanes C, Costa LJ, Wu J et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood 2011; 118: 282–288.
Acknowledgements
We thank all the allogeneic transplantation centers of the EBMT group for reporting the data included in this analysis to this registry. A list of the participating EBMT centers appears in the Appendix.
Author Contributions
SP designed research, collected and checked the data, contacted transplantation centers, analyzed data and wrote the paper; ML designed research, analyzed data and wrote the paper; FC designed research and wrote the paper; AB and JT provided data and wrote the paper; N-CG wrote the paper; HH SS, YK, WD, BD, EG and WA provided data; AN and MM wrote the paper.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix
EBMT participating centers: Hematology and Bone Marrow Transplant Unit, San Raffaele Hospital, Milan (61 patients); Stem Cell Transplant Unit, Fondazione Policlinico Tor Vergata, Tor Vergata University, Rome, Italy (30 patients); Division of Hematology II, IRCCS, San Martino University Hospital—IST, Genoa, Italy (21 patients); The First Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, China (17 patients); Department of Hematology, Ospedale Civile, Pescara, Italy (16 patients); Hematopoietic Stem Cell Transplantation Unit, MedicalPark Hospital, Antalya, Turkey (13 patients); First Affiliated Hospital of Soochow University, Suzhou, China (13 patients); Department of Bone Marrow Transplantation, University Hospital, Essen, Germany (8 patients); University Hospital of Munich-Klinikum Grosshadern (LMU), Department of Internal Medicine III, Hematopoietic Cell Transplantation, Munich, Germany (6 patients); Medizinische Klinik und Poliklinik I, Universitaetsklinikum Carl Gustav Carus der TU Dresden, Dresden, Germany (6 patients); Azienda Ospedaliera, Reggio Calabria, Italy (5 patients); University Hospital Gasthuisberg, Leuven, Belgium (4 patients); Azienda Ospedali Riuniti di Ancona, Ancona-Torrete, Italy (4 patients); University Hospital, Basel, Switzerland (3 patients); University Hospital, Udine, Italy (3 patients); Gazi Universitesi Tip Fakültesi, Ankara, Turkey (2 patients); University Med. Center, Ljubljana, Slovenia (2 patients); Heilig Hartziekenhuis, Roeselare, Belgium (2 patients); Tel-Aviv University, Tel-Hashomer, Israel (2 patients); Hospital Guglielmo da Saliceto, Piacenza, Italy (1 patient); Universität Tübingen, Tübingen, Germany (1 patient); Unité de transplantation et de thérapie cellulaire, Marseille, France (1 patient); Ospedale S. Camillo-Forlanini, Rome, Italy (1 patient); Centre For Clinical Haematology, Birmingham, United Kingdom (1 patient); King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia (1 patient); Helsinki University Central Hospital, Helsinki, Finland (1 patient); University Hospital Eppendorf, Hamburg, Germany (1 patient); Shariati Hospital,Teheran, Iran (1 patient); Umea University Hospital, Umeå, Sweden (1 patient); and University of Freiburg, Freiburg, Germany (1 patient).
Rights and permissions
About this article
Cite this article
Piemontese, S., Ciceri, F., Labopin, M. et al. A survey on unmanipulated haploidentical hematopoietic stem cell transplantation in adults with acute leukemia. Leukemia 29, 1069–1075 (2015). https://doi.org/10.1038/leu.2014.336
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2014.336
This article is cited by
-
EASIX predicts non-relapse mortality after haploidentical transplantation with post-transplant cyclophosphamide
Bone Marrow Transplantation (2023)
-
Second haploidentical stem cell transplantation (HAPLO-SCT2) after relapse from a first HAPLO-SCT in acute leukaemia—a study on behalf of the Acute Leukaemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT)
Bone Marrow Transplantation (2023)
-
Comparison of central nervous system relapse outcomes following haploidentical vs identical-sibling transplant for acute lymphoblastic leukemia
Annals of Hematology (2020)
-
Haploidentical stem cell transplantation (HaploSCT) for patients with acute leukemia—an update on behalf of the ALWP of the EBMT
Bone Marrow Transplantation (2019)
-
Eltrombopag is an effective and safe therapy for refractory thrombocytopenia after haploidentical hematopoietic stem cell transplantation
Bone Marrow Transplantation (2019)