Abstract
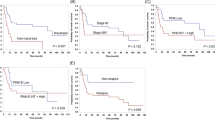
Extranodal, nasal-type natural killer (NK)/T-cell lymphoma (NKCL) is an aggressive malignancy with poor prognosis in which, usually, signal transducer and activator of transcription 3 (STAT3) is constitutively activated and oncogenic. Here, we demonstrate that STAT3 activation mostly results from constitutive Janus kinase (JAK)3 phosphorylation on tyrosine 980, as observed in three of the four tested NKCL cell lines and in 20 of the 23 NKCL tumor samples under study. In one of the cell lines and in 4 of 19 (21%) NKCL primary tumor samples, constitutive JAK3 activation was related to an acquired mutation (A573V or V722I) in the JAK3 pseudokinase domain. We then show that constitutive activation of the JAK3/STAT3 pathway has a major role in NKCL cell growth and survival and in the invasive phenotype. Indeed, NKCL cell growth was slowed down in vitro by targeting JAK3 with chemical inhibitors or small-interfering RNAs. In a human NKCL xenograft mouse model, tumor growth was significantly delayed by the JAK3 inhibitor CP-690550. Altogether, the constitutive activation of JAK3, which can result from JAK3-activating mutations, is a frequent feature of NKCL that deserves to be tested as a therapeutic target.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
Accession codes
References
Jaffe ES, Krenacs L, Raffeld M . Classification of cytotoxic T-cell and natural killer cell lymphomas. Semin Hematol 2003; 40: 175–184.
Jaffe ES, Harris NL, Stein H, Isaacson PG . Classification of lymphoid neoplasms: the microscope as a tool for disease discovery. Blood 2008; 112: 4384–4399.
Kanavaros P, Lescs MC, Briere J, Divine M, Galateau F, Joab I et al. Nasal T-cell lymphoma: a clinicopathologic entity associated with peculiar phenotype and with Epstein-Barr virus. Blood 1993; 81: 2688–2695.
Kim TM, Lee SY, Jeon YK, Ryoo BY, Cho GJ, Hong YS et al. Clinical heterogeneity of extranodal NK/T-cell lymphoma, nasal type: a national survey of the Korean Cancer Study Group. Ann Oncol 2008; 19: 1477–1484.
Nagafuji K, Fujisaki T, Arima F, Ohshima K . L-asparaginase induced durable remission of relapsed nasal NK/T-cell lymphoma after autologous peripheral blood stem cell transplantation. Int J Hematol 2001; 74: 447–450.
Jaccard A, Gachard N, Marin B, Rogez S, Audrain M, Suarez F et al. Efficacy of L-asparaginase with methotrexate and dexamethasone (AspaMetDex regimen) in patients with refractory or relapsing extranodal NK/T-cell lymphoma, a phase 2 study. Blood 2011; 117: 1834–1839.
Yamaguchi M, Kwong YL, Kim WS, Maeda Y, Hashimoto C, Suh C et al. Phase II study of SMILE chemotherapy for newly diagnosed stage IV, relapsed, or refractory extranodal natural killer (NK)/T-cell lymphoma, nasal type: the NK-Cell Tumor Study Group study. J Clin Oncol 2011; 29: 4410–4416.
Au WY, Weisenburger DD, Intragumtornchai T, Nakamura S, Kim WS, Sng I et al. Clinical differences between nasal and extranasal natural killer/T-cell lymphoma: a study of 136 cases from the International Peripheral T-Cell Lymphoma Project. Blood 2009; 113: 3931–3937.
Coppo P, Gouilleux-Gruart V, Huang Y, Bouhlal H, Bouamar H, Bouchet S et al. STAT3 transcription factor is constitutively activated and is oncogenic in nasal-type NK/T-cell lymphoma. Leukemia 2009; 23: 1667–1678.
Huang Y, de Reynies A, de Leval L, Ghazi B, Martin-Garcia N, Travert M et al. Gene expression profiling identifies emerging oncogenic pathways operating in extranodal NK/T-cell lymphoma, nasal type. Blood 2010; 115: 1226–1237.
Iqbal J, Weisenburger DD, Chowdhury A, Tsai MY, Srivastava G, Greiner TC et al. Natural killer cell lymphoma shares strikingly similar molecular features with a group of non-hepatosplenic gamma delta T-cell lymphoma and is highly sensitive to a novel aurora kinase A inhibitor in vitro. Leukemia 2011; 25: 348–358.
Karube K, Nakagawa M, Tsuzuki S, Takeuchi I, Honma K, Nakashima Y et al. Identification of FOXO3 and PRDM1 as tumor-suppressor gene candidates in NK-cell neoplasms by genomic and functional analyses. Blood 2011; 118: 3195–3204.
Kucuk C, Iqbal J, Hu X, Gaulard P, De Leval L, Srivastava G et al. PRDM1 is a tumor suppressor gene in natural killer cell malignancies. Proc Natl Acad Sci USA 2011; 108: 20119–20124.
Quintanilla-Martinez L, Kremer M, Keller G, Nathrath M, Gamboa-Dominguez A, Meneses A et al. p53 Mutations in nasal natural killer/T-cell lymphoma from Mexico: association with large cell morphology and advanced disease. Am J Pathol 2001; 159: 2095–2105.
Takakuwa T, Dong Z, Nakatsuka S, Kojya S, Harabuchi Y, Yang WI et al. Frequent mutations of Fas gene in nasal NK/T cell lymphoma. Oncogene 2002; 21: 4702–4705.
Takahara M, Kishibe K, Bandoh N, Nonaka S, Harabuchi Y . P53, N- and K-Ras, and beta-catenin gene mutations and prognostic factors in nasal NK/T-cell lymphoma from Hokkaido, Japan. Hum Pathol 2004; 35: 86–95.
Jeon YK, Kim H, Park SO, Choi HY, Kim YA, Park SS et al. Resistance to Fas-mediated apoptosis is restored by cycloheximide through the downregulation of cellular FLIPL in NK/T-cell lymphoma. Lab Invest 2005; 85: 874–884.
Ng SB, Yan J, Huang G, Selvarajan V, Tay JL, Lin B et al. Dysregulated microRNAs affect pathways and targets of biologic relevance in nasal-type natural killer/T-cell lymphoma. Blood 2011; 118: 4919–4929.
Yamaguchi M, Kita K, Miwa H, Nishii K, Oka K, Ohno T et al. Frequent expression of P-glycoprotein/MDR1 by nasal T-cell lymphoma cells. Cancer 1995; 76: 2351–2356.
Bossard C, Belhadj K, Reyes F, Martin-Garcia N, Berger F, Kummer JA et al. Expression of the granzyme B inhibitor PI9 predicts outcome in nasal NK/T-cell lymphoma: results of a Western series of 48 patients treated with first-line polychemotherapy within the Groupe d'Etude des Lymphomes de l'Adulte (GELA) trials. Blood 2007; 109: 2183–2189.
Malamut G, El Machhour R, Montcuquet N, Martin-Lanneree S, Dusanter-Fourt I, Verkarre V et al. IL-15 triggers an antiapoptotic pathway in human intraepithelial lymphocytes that is a potential new target in celiac disease-associated inflammation and lymphomagenesis. J Clin Invest 2011; 120: 2131–2143.
Drexler HG, Matsuo Y . Malignant hematopoietic cell lines: in vitro models for the study of natural killer cell leukemia-lymphoma. Leukemia 2000; 14: 777–782.
De Wever O, Hendrix A, De Boeck A, Westbroek W, Braems G, Emami S et al. Modeling and quantification of cancer cell invasion through collagen type I matrices. Int J Dev Biol 2010; 54: 887–896.
Ju W, Zhang M, Jiang JK, Thomas CJ, Oh U, Bryant BR et al. CP-690,550, a therapeutic agent, inhibits cytokine-mediated Jak3 activation and proliferation of T cells from patients with ATL and HAM/TSP. Blood 2011; 117: 1938–1946.
Gozgit JM, Bebernitz G, Patil P, Ye M, Parmentier J, Wu J et al. Effects of the JAK2 inhibitor, AZ960, on Pim/BAD/BCL-xL survival signaling in the human JAK2 V617F cell line SET-2. J Biol Chem 2008; 283: 32334–32343.
Kim TM, Heo DS . Extranodal NK/ T-cell lymphoma, nasal type: new staging system and treatment strategies. Cancer Sci 2009; 100: 2242–2248.
Walters DK, Mercher T, Gu TL, O'Hare T, Tyner JW, Loriaux M et al. Activating alleles of JAK3 in acute megakaryoblastic leukemia. Cancer Cell 2006; 10: 65–75.
Malinge S, Ragu C, Della-Valle V, Pisani D, Constantinescu SN, Perez C et al. Activating mutations in human acute megakaryoblastic leukemia. Blood 2008; 112: 4220–4226.
Fleischmann R, Kremer J, Cush J, Schulze-Koops H, Connell CA, Bradley JD et al. Placebo-controlled trial of tofacitinib monotherapy in rheumatoid arthritis. N Engl J Med 2012; 367: 495–507.
van Vollenhoven RF, Fleischmann R, Cohen S, Lee EB, Garcia Meijide JA, Wagner S et al. Tofacitinib or adalimumab versus placebo in rheumatoid arthritis. N Engl J Med 2012; 367: 508–519.
Knoops L, Renauld JC . IL-9 and its receptor: from signal transduction to tumorigenesis. Growth Factors 2004; 22: 207–215.
Knoops L, Hornakova T, Royer Y, Constantinescu SN, Renauld JC . JAK kinases overexpression promotes in vitro cell transformation. Oncogene 2008; 27: 1511–1519.
Cornejo MG, Boggon TJ, Mercher T . JAK3: a two-faced player in hematological disorders. Int J Biochem Cell Biol 2009; 41: 2376–2379.
Cornejo MG, Kharas MG, Werneck MB, Le Bras S, Moore SA, Ball B et al. Constitutive JAK3 activation induces lymphoproliferative syndromes in murine bone marrow transplantation models. Blood 2009; 113: 2746–2754.
Crockett DK, Lin Z, Elenitoba-Johnson KS, Lim MS . Identification of NPM-ALK interacting proteins by tandem mass spectrometry. Oncogene 2004; 23: 2617–2629.
Elliott NE, Cleveland SM, Grann V, Janik J, Waldmann TA, Dave UP . FERM domain mutations induce gain of function in JAK3 in adult T-cell leukemia/lymphoma. Blood 2011; 118: 3911–3921.
Zhang J, Ding L, Holmfeldt L, Wu G, Heatley SL, Payne-Turner D et al. The genetic basis of early T-cell precursor acute lymphoblastic leukaemia. Nature 2012; 481: 157–163.
Yu JB, Zhang YC, Yang QP, Wang XL, Tang Y, Zhao S et al. Invasion-associated genes identified by gene expression profiling in extranodal natural killer/T-cell lymphoma, nasal type. Leuk Lymphoma 2012; 54: 90–98.
Friedl P, Alexander S . Cancer invasion and the microenvironment: plasticity and reciprocity. Cell 2011; 147: 992–1009.
Carragher NO, Walker SM, Scott Carragher LA, Harris F, Sawyer TK, Brunton VG et al. Calpain 2 and Src dependence distinguishes mesenchymal and amoeboid modes of tumour cell invasion: a link to integrin function. Oncogene 2006; 25: 5726–5740.
Koo GC, Tan SY, Tang T, Poon SL, Allen GE, Tan L et al. Janus Kinase 3-Activating Mutations Identified in Natural Killer/T-cell Lymphoma. Cancer Discov 2012; 2: 591–597.
Acknowledgements
We are indebted to Professor Kaiss Lassoued for invaluable discussions and advice. This work was funded in part by grants from the following institutions: Etablissement Français du Sang (CS/2002/009), GIS-Institut des Maladies Rares (GIS MR0428), Fondation pour la Recherche Médicale (FRM) and Institut National du Cancer (INCA). We also thank Virginie Fataccioli for the management of the TENOMIC program, and Sandrine Malot and Cécile K Lopez for technical assistance, as well as the members of the consortium TENOMIC (cited in Appendix).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Leukemia website
Supplementary information
Appendix
Appendix
The members of the consortium TENOMIC are:
A Martin, Hôpital Avicenne, Bobigny; I Soubeyran, P Soubeyran, Institut Bergonié, Bordeaux; P Dechelotte, A Pilon, O Tournilhac, Hôtel-Dieu, Clermont Ferrand; K Leroy, P Gaulard, MH Delfau, C Copie-Bergman, A Plonquet, C Haïoun, F Le Bras, Hôpital Henri Mondor, Créteil; T Petrella, L Martin, JN Bastié, O Casasnovas, CHU, Dijon; B Fabre, D Salameire, R Gressin, D Leroux, MC Jacob, CHU, Grenoble; L de Leval, B Bisig, G Fillet, C Bonnet, CHU Sart-Tilman, Liège; MC Copin, B Bouchindhomme, F Morschhauser, CHU, Lille; B Petit, A Jaccard, Hôpital Dupuytren, Limoges; F Berger, B Coiffier, CHU Sud, Lyon; T Rousset, P Quittet, G Cartron, Hôpital Gui de Chauliac-St Eloi, Montpellier; S Thiebault, B Drenou, Hôpital E Muller, Mulhouse; K Montagne, C Bastien, S Bologna, CHU de Brabois, Nancy; C Bossard, S Le Gouill, Hôtel-Dieu, Nantes; T Molina, Hôtel-Dieu, Paris; J Brière, C Gisselbrecht, Hôpital St Louis, Paris; B Fabiani, A Aline-Fardin, P Coppo, Hôpital Saint-Antoine, Paris; F Charlotte, J Gabarre, Hôpital Pitié-Salpétrière, Paris; J Bruneau, D Canioni, V Verkarre, E Macintyre, V Asnafi, O Hermine, R Delarue, F Suarez, D Sibon, JP Jaïs, Hôpital Necker, Paris; M Parrens, JP Merlio, E Laharanne, K Bouabdallah, Hôpital Haut Lévêque, Bordeaux; S Maugendre-Caulet, P Tas, T Lamy, CHU Pontchaillou, Rennes; JM Picquenot, F Jardin, C Bastard, Centre H Becquerel, Rouen; M Peoc′h, J Cornillon, CHU, Saint Etienne; L Lamant, G Laurent, L Oberic, Hôpital Purpan, Toulouse; J Bosq, P Dartigues, V Ribrag, Institut G Roussy, Villejuif; M Patey, A Delmer, Hôpital R Debré, Reims; JF Emile, K Jondeau, Hôpital Ambroise Paré, Boulogne; MC Rousselet, M Hunault, CHU, Angers; C Badoual, Hôpital Européen Georges Pompidou, Paris; C Legendre, F Boidart, S Castaigne, AL Taksin, CH Versailles, Le Chesnay; J Vadrot, A Devidas, B Joly, CH Sud francilien, Corbeil; Dr Gandhi Damaj, CHU Amiens; F Lemonnier, M Travert, INSERM U955, Créteil; P Dessen, G Meurice, Institut G Roussy, Villejuif; M Delorenzi, E Missiaglia, N Houhou, P David, Swiss Institute of Bioinformatics, Lausanne, Switzerland; F Radvanyi, E Chapeaublanc, Institut Curie, Paris; P Ferrier, S Spicuglia, CIML, Marseille; J Soulier, Hôpital St Louis, Paris; C Thibault, IGBMC, Illkirsch. The LYSA (Lymphoma Study Association). Plate-Forme de Ressources Biologiques, Hôpital H Mondor, Créteil. V Fataccioli, Project Manager, Hôpital H Mondor, Créteil.
Rights and permissions
About this article
Cite this article
Bouchekioua, A., Scourzic, L., de Wever, O. et al. JAK3 deregulation by activating mutations confers invasive growth advantage in extranodal nasal-type natural killer cell lymphoma. Leukemia 28, 338–348 (2014). https://doi.org/10.1038/leu.2013.157
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2013.157
Keywords
This article is cited by
-
Idiopathic erythrocytosis: a germline disease?
Clinical and Experimental Medicine (2024)
-
Novel target and treatment agents for natural killer/T-cell lymphoma
Journal of Hematology & Oncology (2023)
-
Mature T-cell and NK-cell lymphomas: updates on molecular genetic features
International Journal of Hematology (2023)
-
In vivo impact of JAK3 A573V mutation revealed using zebrafish
Cellular and Molecular Life Sciences (2022)
-
Mesenchymal stem/stromal cells in cancer therapy
Journal of Hematology & Oncology (2021)