Abstract
An expert panel convened to reach a consensus regarding the optimal use of lenalidomide in combination with dexamethasone (Len/Dex) in patients with relapsed or refractory multiple myeloma (RRMM). On the basis of the available evidence, the panel agreed that Len/Dex is a valid and effective treatment option for most patients with RRMM. As with other therapies, using Len/Dex at first relapse is more effective regarding response rate and durability than using it after multiple salvage therapies. Len/Dex may be beneficial regardless of patient age, disease stage and renal function, although the starting dose of lenalidomide should be adjusted for renal impairment and cytopenias. Long-term treatment until there is evidence of disease progression may be recommended at the best-tolerated doses of both lenalidomide and dexamethasone. Recommendations regarding the prevention and management of adverse events, particularly venous thromboembolism and myelosuppression, were provided on the basis of the available evidence and practical experience of panel members. Ongoing trials will provide more insight into the effects of continuous lenalidomide-based therapy in myeloma.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Kumar SK, Rajkumar SV, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Kastritis E, Zervas K, Symeonidis A, Terpos E, Delimbassi S, Anagnostopoulos N et al. Improved survival of patients with multiple myeloma after the introduction of novel agents and the applicability of the International Staging System (ISS): an analysis of the Greek Myeloma Study Group (GMSG). Leukemia 2009; 23: 1152–1157.
Rajkumar SV . Treatment of myeloma: cure vs control. Mayo Clinic Proc 2008; 83: 1142–1145.
Gandhi AK, Kang J, Capone L, Parton A, Wu L, Zhang LH et al. Dexamethasone synergizes with lenalidomide to inhibit multiple myeloma tumor growth, but reduces lenalidomide-induced immunomodulation of T and NK cell function. Curr Cancer Drug Targets 2010; 10: 155–167.
Davies FE, Raje N, Hideshima T, Lentzsch S, Young G, Tai YT et al. Thalidomide and immunomodulatory derivatives augment natural killer cell cytotoxicity in multiple myeloma. Blood 2001; 98: 210–216.
Verhelle D, Corral LG, Wong K, Mueller JH, Moutouh-de Parseval L, Jensen-Pergakes K et al. Lenalidomide and CC-4047 inhibit the proliferation of malignant B cells while expanding normal CD34+ progenitor cells. Cancer Res 2007; 67: 746–755.
Wu L, Adams M, Carter T, Chen R, Muller G, Stirling D et al. Lenalidomide enhances natural killer cell and monocyte-mediated antibody-dependent cellular cytotoxicity of rituximab-treated CD20+ tumor cells. Clin Cancer Res 2008; 14: 4650–4657.
Reddy N, Hernandez-Ilizaliturri FJ, Deeb G, Roth M, Vaughn M, Knight J et al. Immunomodulatory drugs stimulate natural killer-cell function, alter cytokine production by dendritic cells, and inhibit angiogenesis enhancing the anti-tumour activity of rituximab in vivo. Br J Haematol 2008; 140: 36–45.
Tai YT, Li XF, Catley L, Coffey R, Breitkreutz I, Bae J et al. Immunomodulatory drug lenalidomide (CC-5013, IMiD3) augments anti-CD40 SGN-40-induced cytotoxicity in human multiple myeloma: clinical implications. Cancer Res 2005; 65: 11712–11720.
Chiarenza A, Parrinello N, La Cava P, Spina E, Tibullo D, Giallongo C et al. Lenalidomide is able to restore immune system in multiple myeloma patients. Blood 2009; 114: (abstract 4909).
Harousseau JL, Dimopoulos MA, Wang M, Corso A, Chen C, Attal M et al. Better quality of response to lenalidomide plus dexamethasone is associated with improved clinical outcomes in patients with relapsed or refractory multiple myeloma. Haematologica 2010; 95: 1738–1744.
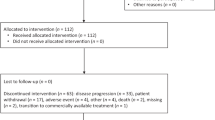
San Miguel JF, Dimopoulos MA, Stadtmauer AE, Rajkumar SV, Siegel D, Bravo ML et al. Effects of lenalidomide and dexamethasone treatment duration on survival in patients with relapsed or refractory multiple myeloma treated with lenalidomide and dexamethasone. Clinl Lymphoma Myeloma Leuk 2010; E-pub ahead of print 26 October 2010.
Attal M, Cristini C, Marit G, Caillot D, Facon T, Hullin C et al. Lenalidomide maintenance after transplantation for myeloma. J Clin Oncol (ASCO Ann Meet Proc) 2010; 28 (Suppl): (abstract 8018).
McCarthy PL, Owzar K, Anderson KC, Hofmeister CC, Hassoun H, Hurd DD et al. Phase III intergroup study of lenalidomide versus placebo maintenance therapy following single autologous stem cell transplant (ASCT) for multiple myeloma (MM): CALGB 100104. J Clin Oncol (ASCO Ann Meet Proc) 2010; 28 (Suppl): (abstract 8017).
Palumbo A, Dimopoulos M, Delforge M, Hajek R, Kropff M, Petrucci MT et al. A phase 3 study to determine the efficacy and safety of lenalidomide combined with melphalan and prednisone in patients ⩾65 years with newly diagnosed multiple myeloma (NDMM). Haematol (EHA Annu Meet Abstr) 2010; 95 (Suppl 2): 234 (abstract 0566).
Richardson PG, Schlossman RL, Weller E, Hideshima T, Mitsiades C, Davies F et al. Immunomodulatory drug CC-5013 overcomes drug resistance and is well tolerated in patients with relapsed multiple myeloma. Blood 2002; 100: 3063–3067.
Richardson PG, Blood E, Mitsiades CS, Jagannath S, Zeldenrust SR, Alsina M et al. A randomized phase 2 study of lenalidomide therapy for patients with relapsed or relapsed and refractory multiple myeloma. Blood 2006; 108: 3458–3464.
Richardson P, Jagannath S, Hussein M, Berenson J, Singhal S, Irwin D et al. Safety and efficacy of single-agent lenalidomide in patients with relapsed and refractory multiple myeloma. Blood 2009; 114: 772–778.
European Medicines Agency. Revlimid summary of product characteristics. European Public Assessment Report: Revlimid. Available from: http://www.emea.europa.eu. Accessed July 2010.
Celgene Corporation. Revlimid Package Insert. Summit, NJ, Available at: http://www.revlimid.com/pdf/REVLIMID_PI.pdf. Accessed July 2010.
Dimopoulos M, Spencer A, Attal M, Prince HM, Harousseau JL, Dmoszynska A et al. Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med 2007; 357: 2123–2132.
Weber DM, Chen C, Niesvizky R, Wang M, Belch A, Stadtmauer EA et al. Lenalidomide plus dexamethasone for relapsed multiple myeloma in North America. N Engl J Med 2007; 357: 2133–2142.
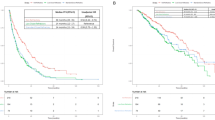
Dimopoulos MA, Chen C, Spencer A, Niesvizky R, Attal M, Stadtmauer EA et al. Long-term follow-up on overall survival from the MM-009 and MM-010 phase III trials of lenalidomide plus dexamethasone in patients with relapsed or refractory multiple myeloma. Leukemia 2009; 23: 2147–2152.
Stadtmauer EA, Weber DM, Niesvizky R, Belch A, Prince MH, San Miguel JF et al. Lenalidomide in combination with dexamethasone at first relapse in comparison with its use as later salvage therapy in relapsed or refractory multiple myeloma. Eur J Haematol 2009; 82: 426–432.
Chanan-Khan AA, Yu Z, Weber D, Chen C, Niesvizky R, Spencer A et al. Lenalidomide (L) in combination with dexamethasone (D) significantly improves time to progression (TTP) in non-stem cell transplant patients (pts) with relapsed or refractory (rel/ref) multiple myeloma (MM): Analysis from MM-009 and MM-010 randomized phase III clinical trials. Blood (ASH Annu Meet Abstr) 2006; 108: (abstract 3554).
Wang M, Dimopoulos MA, Chen C, Cibeira MT, Attal M, Spencer A et al. Lenalidomide plus dexamethasone is more effective than dexamethasone alone in patients with relapsed or refractory multiple myeloma regardless of prior thalidomide exposure. Blood 2008; 112: 4445–4451.
Dimopoulos M, Alegre A, Stadtmauer EA, Goldschmidt H, Zonder JA, de Castro CM et al. The efficacy and safety of lenalidomide plus dexamethasone in relapsed and/or refractory multiple myeloma patients with impaired renal function. Cancer 2010; 116: 3807–3814.
Delforge M, Facon T, Bravo M-L, Dimopoulos MA . Lenalidomide plus dexamethasone has similar tolerability and efficacy in treatment of relapsed/refractory multiple myeloma patients with or without history of neuropathy. Blood (ASH Annu Meet Abstr) 2009; 114: (abstract 3873).
Lonial S, Knight R, Dimopoulos M, Chanan-Khan A, San Miguel JM, Facon T et al. Effect of Len/Dex in MM in different age groups. Haematol (EHA Annu Meet Abstr) 2007; 92 (Suppl 2): (abstract PO-663).
Chanan-Khan AA, Dimopoulos MA, Weber DM, Spencer A, Attal M, Belch A et al. Safety and efficacy outcomes with lenalidomide plus dexamethasone in relapsed or refractory multiple myeloma were not significantly different for the treatment of patients with or without high-risk disease or elderly status. Blood (ASH Annu Meet Abstr) 2008; 112: (abstract 3701).
Dimopoulos MA, Hussein M, Swern AS, Weber D . Full dose of lenalidomide for 12 months followed by a lower maintenance dose improves progression-free survival in patients with relapsed/refractory multiple myeloma. Blood (ASH Annu Meet Abstr) 2009; 114: (abstract 2874).
San Miguel JF, Dimopoulos M, Weber D, Olesnyckyj M, Yu Z, Zeldis J et al. Dexamethasone dose adjustments seem to result in better efficacy and improved tolerability in patients with relapsed/refractory multiple myeloma who are treated with lenalidomide/dexamethasone (MM009/010 sub-analysis). Blood (ASH Annu Meet Abstr) 2007; 110: (abstract 2712).
Kneppers E, Lokhorst HM, Eeltink CM, Huls G, Kersten MJ, Koedam J et al. Analysis of efficacy and prognostic factors of lenalidomide treatment as part of a Dutch compassionate use program. Clin Lymphoma Myeloma Leuk 2010; 10: 138–143.
Avet-Loiseau H, Soulier J, Fermand JP, Yakoub-Agha I, Attal M, Hulin C et al. Impact of high-risk cytogenetics and prior therapy on outcomes in patients with advanced relapsed or refractory multiple myeloma treated with lenalidomide plus dexaméthasone. Leukemia 2010; 24: 623–628.
Dimopoulos MA, Kastritis E, Christoulas D, Migkou M, Gavriatopoulou M, Gkotzamanidou M et al. Treatment of patients with relapsed/refractory multiple myeloma with lenalidomide and dexamethasone with or without bortezomib: prospective evaluation of the impact of cytogenetic abnormalities and of previous therapies. Leukemia 2010; 24: 1769–1778.
Reece D, Song KW, Fu T, Roland B, Chang H, Horsman DE et al. Influence of cytogenetics in patients with relapsed or refractory multiple myeloma treated with lenalidomide plus dexamethasone: adverse effect of deletion 17p13. Blood 2009; 114: 522–525.
Mateos MV, Richardson PG, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O et al. Bortezomib plus melphalan and prednisone compared with melphalan and prednisone in previously untreated multiple myeloma: updated follow-up and impact of subsequent therapy in the phase III VISTA Trial. J Clin Oncol 2010; 28: 2259–2266.
Schey SA, Morgan GJ, Ramasamy K, Hazel B, Ladon D, Corderoy S et al. The addition of cyclophosphamide to lenalidomide and dexamethasone in multiply relapsed/refractory myeloma patients; a phase I/II study. Br J Haematol 2010; 150: 326–333.
Dimopoulos MA, Kastritis E, Christoulas D, Migkou M, Gavriatopoulou M, Gkotzamanidou M et al. Treatment of patients with relapsed/refractory multiple myeloma with lenalidomide and dexamethasone with or without bortezomib: prospective evaluation of the impact of cytogenetic abnormalities and of previous therapies. Leukemia 2010; 24: 1769–1778.
Knop S, Gerecke C, Liebisch P, Topp MS, Platzbecker U, Sezer O et al. Lenalidomide, adriamycin, and dexamethasone (RAD) in patients with relapsed and refractory multiple myeloma: a report from the German Myeloma Study Group DSMM (Deutsche Studiengruppe Multiples Myelom). Blood 2009; 113: 4137–4143.
Dimopoulos MA, Kastritis E, Rosinol L, Bladé J, Ludwig H et al. Pathogenesis and treatment of renal failure in multiple myeloma. Leukemia 2008; 22: 1485–1493.
Quan DJ, Aweeka FT . Dosing of drugs in renal failure. In: Koda-Kimble AM, Young L, Kradjan W, Guglielmo BJ, Aldredge B, Corelli R, Williams B (eds). Applied Therapeutics—The clinical use of drugs, Vol. 34, 8th ed, Lipponcott Williams & Wilkins: Vancouver, WA, 2005, pp 1–25.
Chen N, Lau H, Kong L, Kumar G, Zeldis JB, Knight R et al. Pharmacokinetics of lenalidomide in subjects with various degrees of renal impairment and in subjects on hemodialysis. J Clin Pharmacol 2007; 47: 1466–1475.
de la Rubia J, Roig M, Ibáñez A, García I, Vera JA, Aguilar C et al. Activity and safety of lenalidomide and dexamethasone in multiple myeloma patients requiring dialysis: a Spanish multicenter retrospective study. Eur J Haematol 2010; 85: 363–365.
Reece DE, Masih-Khan E, Chen C, Wang L, Dean S, Kukreti V et al. Use of lenalidomide (Revlimid® +/− corticosteroids in relapsed/refractory multiple myeloma patients with elevated baseline serum creatinine levels. Blood (ASH Annu Meet Abstr) 2006; 108: (abstract 3548).
Dimopoulos MA, Christoulas D, Roussou M, Kastritis E, Migkou M, Gavriatopoulou M et al. Lenalidomide and dexamethasone for the treatment of refractory/relapsed multiple myeloma: dosing of lenalidomide according to renal function and effect on renal impairment. Eur J Haematol 2010; 85: 1–5.
Ludwig H, Zojer N . Renal recovery with lenalidomide in a patient with bortezomib-resistant multiple myeloma. Nat Rev Clin Oncol 2010; 7: 289–294.
Mateos MV, García-Sanz R, Colado E, Olazábal J, San-Miguel J . Should prophylactic granulocyte-colony stimulating factor be used in multiple myeloma patients developing neutropenia under lenalidomide-based therapy? Br J Haematol 2008; 140: 324–326.
Rajkumar SV, Jacobus S, Callander NS, Fonseca R, Vesole DH, Williams ME et al. Lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone as initial therapy for newly diagnosed multiple myeloma: an open-label randomised controlled trial. Lancet Oncol 2010; 11: 29–37.
Klein U, Kosely F, Hillengass J, Hundemer M, Schmitt S, Neben K et al. Effective prophylaxis of thromboembolic complications with low molecular weight heparin in relapsed multiple myeloma patients treated with lenalidomide and dexamethasone. Ann Hematol 2009; 88: 67–71.
Niesvizky R, Wang L, Orlowski RZ, Bensinger W, Alsina M, Gabrail N et al. Phase Ib multicenter dose escalation study of carfilzomib plus lenalidomide and low dose dexamethasone (CRd) in relapsed and refractory multiple myeloma (MM). Blood (ASH Annu Meet Abstr) 2009; 114: (abstract 304).
van de Donk NW, Wittebol S, Minnema MC, Lokhorst HM . Lenalidomide (Revlimid) combined with continuous oral cyclophosphamide (endoxan) and prednisone (REP) is effective in lenalidomide/dexamethasone-refractory myeloma. Br J Haematol 2010; 148: 335–337.
Hussein MA, Bolejack V, Zonder JA, Durie BG, Jakubowiak AJ, Crowley JJ et al. Phase II study of thalidomide plus dexamethasone induction followed by tandem melphalan-based autotransplantation and thalidomide-plus-prednisone maintenance for untreated multiple myeloma: a southwest oncology group trial (S0204). J Clin Oncol 2009; 27: 3510–3517.
Stewart AK, Chen CI, Howson-Jan K, White D, Roy J, Kovacs MJ et al. Results of a multicenter randomized phase II trial of thalidomide and prednisone maintenance therapy for multiple myeloma after autologous stem cell transplant. Clin Cancer Res 2004; 10: 8170–8176.
Palumbo A, Gay F, Falco P, Crippa C, Montefusco V, Patriarca F et al. Bortezomib as induction before autologous transplantation, followed by lenalidomide as consolidation-maintenance in untreated multiple myeloma patients. J Clin Oncol 2010; 28: 800–807.
Blau I, Gimsing P, Drenou B, Masini L, Lokhorst H, Waage A et al. Post-approval safety study (PASS) of lenalidomide compared with other treatments in patients with relapsed or refractory multiple myeloma: first report on 518 patients. Haematol (EHA Annu Meet Abstr) 2010; 95 (Suppl 2): 154 (abstract 383).
Niesvizky R, Naib T, Christos PJ, Jayabalan D, Furst JR, Jalbrzikowski J et al. Lenalidomide-induced myelosuppression is associated with renal dysfunction: adverse events evaluation of treatment-naïve patients undergoing front-line lenalidomide and dexamethasone therapy. Br J Haematol 2007; 138: 640–643.
Fonseca R, Bergsagel PL, Drach J, Shaughnessy J, Gutierrez N, Stewart AK et al. International Myeloma Working Group molecular classification of multiple myeloma: spotlight review. Leukemia 2009; 23: 2210–2221.
Barlogie B, Tricot GJ, van Rhee F, Angtuaco E, Walker R, Epstein J et al. Long-term outcome results of the first tandem autotransplant trial for multiple myeloma. Br J Haematol 2006; 135: 158–164.
Avet-Loiseau H, Attal M, Moreau P, Charbonnel C, Garban F, Hulin C et al. Genetic abnormalities and survival in multiple myeloma: the experience of the Intergroupe Francophone du Myélome. Blood 2007; 109: 3489–3495.
Hoering A, Crowley J, Shaughnessy Jr JD, Hollmig K, Alsayed Y, Szymonifka J et al. Complete remission in multiple myeloma examined as time-dependent variable in terms of both onset and duration in total therapy protocols. Blood 2009; 114: 1299–1305.
Moreau P, Attal M, Garban F, Hulin C, Facon T, Marit G et al. Heterogeneity of t(4;14) in multiple myeloma. Long-term follow-up of 100 cases treated with tandem transplantation in IFM99 trials. Leukemia 2007; 21: 2020–2024.
Lonial S . Risky business in myeloma. Blood 2009; 114: 496–497.
Zonder JA, Crowley JJ, Bolejack V, Hussein MA, Moore Sr DF, Whittenberger BF et al. A randomized Southwest Oncology Group study comparing dexamethasone (D) to lenalidomide + dexamethasone (LD) as treatment of newly-diagnosed multiple myeloma (NDMM): Impact of cytogenetic abnormalities on efficacy of LD, and updated overall study results. J Clin Oncol (ASCO Annu Meet Proc) 2008; 26 (Suppl): (abstract 8521).
Kapoor P, Kumar S, Fonseca R, Lacy MQ, Witzig TE, Hayman SR et al. Impact of risk stratification on outcome among patients with multiple myeloma receiving initial therapy with lenalidomide and dexamethasone. Blood 2009; 114: 518–521.
Richardson P, Jagannath S, Jakubowiak A, Lonial S, Raje N, Alsina M et al. Lenalidomide, bortezomib, and dexamethasone in patients with relapsed or relapsed/refractory multiple myeloma (MM): encouraging response rates and tolerability with correlation of outcome and adverse cytogenetics in a phase II study. Blood (ASH Annu Meet Abstr) 2008; 112: (abstract 1742).
Cavo M, Testoni N, Terragna C, Marzocchi G, Durante S, Zambello R et al. Superior rate of complete response with up-front Velcade-thalidomide-dexamethasone versus thalidomide-dexamethasone in newly diagnosed multiple myeloma is not affected by adverse prognostic factors, including high-risk cytogenetic abnormalities. Blood (ASH Annu Meet Abstr) 2008; 112: (abstract 1662).
Avet-Loiseau H, Leleu X, Roussel M, Moreau P, Guerin-Charbonnel C, Caillot D et al. Bortezomib plus dexamethasone induction improves outcome of patients with t(4;14) myeloma but not outcome of patients with del(17p). J Clin Oncol 2010; 28: 4630–4634.
Chen C, Reece DE, Siegel D, Niesvizky R, Boccia RV, Stadtmauer EA et al. Expanded safety experience with lenalidomide plus dexamethasone in relapsed or refractory multiple myeloma. Br J Haematol 2009; 146: 164–170.
Ishak J, Dimopoulos MA, Weber D, Knight RD, Shearer A, Caro JJ . Declining rates of adverse events and dose modifications with lenalidomide in combination with dexamethasone. Blood (ASH Annu Meet Abstr) 2008; 112: (abstract 3708).
Lonial S, Baz R, Swern AS, Weber D, Dimopoulos MA . Neutropenia is a predictable and early event in affected patients with relapsed/refractory multiple myeloma treated with lenalidomide in combination with dexamethasone. Blood (ASH Annu Meet Abstr) 2009; 114: (abstract 2879).
Bennett CL, Angelotta C, Yarnold PR, Evens AM, Zonder JA, Raisch DW et al. Thalidomide- and lenalidomide-associated thromboembolism among patients with cancer. JAMA 2006; 296: 2558–2560.
Niesvizky R, Spencer A, Wang M, Weber D, Chen C, Dimopoulos MA et al. Increased risk of thrombosis with lenalidomide in combination with dexamethasone and erythropoietin. J Clin Oncol (ASCO Annu Meet Proc) 2006; 24 (Suppl): (abstract 7506).
Rizzo JD, Somerfield MR, Hagerty KL, Seidenfeld J, Bohlius J, Bennett CL et al. Use of epoetin and darbepoetin in patients with cancer: 2007 American Society of Clinical Oncology/American Society of Hematology clinical practice guideline update. J Clin Oncol 2008; 26: 132–149.
Palumbo A, Rajkumar SV, Dimopoulos MA, Richardson PG, San Miguel J, Barlogie B et al. Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia 2008; 22: 414–423.
Zonder JA, Barlogie B, Durie BG, McCoy J, Crowley J, Hussein MA . Thrombotic complications in patients with newly diagnosed multiple myeloma treated with lenalidomide and dexamethasone: benefit of aspirin prophylaxis. Blood 2006; 108: 403.
Zangari M, Tricot G, Polavaram L, Zhan F, Finlayson A, Knight R et al. Survival effect of venous thromboembolism in patients with multiple myeloma treated with lenalidomide and high-dose dexamethasone. J Clin Oncol 2010; 28: 132–135.
Sviggum HP, Davis MD, Rajkumar SV, Dispenzieri A . Dermatologic adverse effects of lenalidomide therapy for amyloidosis and multiple myeloma. Arch Dermatol 2006; 142: 1298–1302.
Palumbo A, Dimopoulos M, San Miguel J, Harousseau JL, Attal M, Hussein M et al. Lenalidomide in combination with dexamethasone for the treatment of relapsed or refractory multiple myeloma. Blood Rev 2009; 23: 87–93.
Acknowledgements
We received support regarding linguistic improvement, artwork and formatting of the manuscript from Excerpta Medica, funded by Celgene Corporation. We are fully responsible for content and editorial decisions for this manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
MAD had a consultant role for, and has received honoraria from, Celgene. AP is a speaker for, advisory board member of, and has received a research grant from, Celgene. HL has received honoraria from, and is a speakers’ bureau member of Celgene, Mundipharma and Ortho Biotech. MA is an advisory board member of Celgene. MB is a speakers’ bureau member of Celgene and Janssen-Cilag, and has received honorarium from Celgene. HE has received honoraria from Celgene. FLC had a consultant role for, and received honoraria from, Celgene, Amgen, MSD and Janssen-Cilag. U-HM is an advisory board member of Celgene and has received a research grant from Janssen-Cilag. FED has served as a speakers’ bureau member of Celgene and Ortho Biotech, and has participated in advisory boards of Celgene, Ortho Biotech and Novartis. J-LH has received consulting and lecture fees from Celgene. MD is an advisory board member of, and has received honoraria as a speaker from, Celgene. PS is an advisory board member of Celgene, Janssen-Cilag and Onyx, and has received research funding from Celgene and Janssen-Cilag. RH has received reimbursement of expenses and honoraria for attending symposia from Celgene. JFS-M has received compensation as a scientific advisory board member from Millennium, Celgene and Janssen-Cilag. SZ has received compensation as a scientific advisory board member of Celgene. GJM received payment for lectures including service on speakers’ bureaus from Novartis, Celgene and Ortho Biotech.
Additional information
Author contribution
MAD, AP and PS planned this review; MAD wrote the first draft of the manuscript. All authors reviewed and commented on the draft and approved the final manuscript.
Rights and permissions
About this article
Cite this article
Dimopoulos, M., Palumbo, A., Attal, M. et al. Optimizing the use of lenalidomide in relapsed or refractory multiple myeloma: consensus statement. Leukemia 25, 749–760 (2011). https://doi.org/10.1038/leu.2011.3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2011.3
Keywords
This article is cited by
-
Cost utility and budget impact analysis of dexamethasone compared with bortezomib and lenalidomide for the treatment of second line multiple myeloma from a South African public health perspective
Cost Effectiveness and Resource Allocation (2022)
-
The clinical management of lenalidomide-based therapy in patients with newly diagnosed multiple myeloma
Annals of Hematology (2020)
-
The effectiveness and safety of lenalidomide and dexamethasone in patients with relapsed/refractory multiple myeloma in real-world clinical practice: a study of the Korean Multiple Myeloma Working Party (KMMWP-151 study)
Annals of Hematology (2020)
-
Influence of ABCB1 polymorphisms on the pharmacokinetics and toxicity of lenalidomide in patients with multiple myeloma
Medical Oncology (2019)
-
Longer procoagulant phospholipid-dependent clotting time, lower endogenous thrombin potential and higher tissue factor pathway inhibitor concentrations are associated with increased VTE occurrence in patients with newly diagnosed multiple myeloma: results of the prospective ROADMAP-MM-CAT study
Blood Cancer Journal (2018)