Abstract
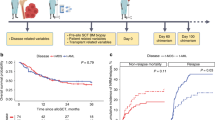
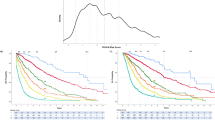
Myelodysplastic syndromes (MDS) with del(5q) are considered to have a benign course of the disease. In order to address the issue of the propensity of those patients to progress to acute myeloid leukemia (AML), data on 381 untreated patients with MDS and del(5q) characterized by low or intermediate I International Prognostic Scoring System (IPSS) risk score were collected from nine centers and registries. Median survival of the entire group was 74 months. Transfusion-dependent patients had a median survival of 44 months vs 97 months for transfusion-independent patients (P<0.0001). Transfusion need at diagnosis was the most important patient characteristic for survival. Of the 381 patients, 48 (12.6%) progressed to AML. The cumulative progression rate calculated using the Kaplan–Meier method was 4.9% at 2 years and 17.6% at 5 years. Factors associated with the risk of AML transformation were high-risk World Health Organization adapted Prognostic Scoring System (WPSS) score, marrow blast count >5% and red-cell transfusion dependency at diagnosis. In conclusion, patients with MDS and del(5q) are facing a considerable risk of AML transformation. More detailed cytogenetic and molecular studies may help to identify the patients at risk of progression.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Van den Berghe JH, Cassima JJ, David G, Fryns JP, Michaux JL, Sokal G . Distinct haematological disorder with deletion of long arm of no.5 chromosom. Nature 1974; 251: 437–443.
Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J et al. World Health Organization classification of neoplastic diseases of the hematopoietic and lymphoid tissues: report of the Clinical Advisory Committee meeting-Airlie House, Virginia, November 1997. J Clin Oncol 1999; 17: 3835–3849.
Brunning R, Orazi A, Germing U, Le Beau MM, Porwit A, Baumann I et al. Myelodysplastic syndromes/neoplasms. In Swerdlow S, et al (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press: Lyon, 2008.
Giagounidis A, Germing U, Wainscoat JS, Boultwood J, Aul C . The 5q- Syndrome. Hematology 2004; 9: 271–277.
Germing U, Gattermann N, Strupp C, Aivado M, Aul C . Validation of the WHO proposals for a new classification of primary myelodysplastic syndromes: a retrospective analysis of 1600 patients. Leuk Res 2000; 24: 983–992.
Germing U, Strupp C, Kuendgen A, Isa S, Knipp S, Hildebrandt B et al. Prospective validation of the WHO proposals for the classification of myelodysplastic syndromes. Haematologica 2006; 91: 1596–1604.
Greenberg P, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood 1997; 89: 2079–2088.
Malcovati L, Germing U, Kuendgen A, Della Porta MG, Pascutto C, Invernizzi R et al. Time-dependent prognostic scoring system for predicting survival and leukemic evolution in myelodysplastic syndromes. J Clin Oncol 2007; 25: 3503–3510.
Germing U, Aul C, Niemeyer CM, Haas R, Bennett JM . Epidemiology, classification and prognosis of adults and children with myelodysplastic syndromes. Ann Hematol 2008; 87: 691–699.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Gooley TA, Leisenring W, Crowley J, Storer BE . Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med 1999; 18: 695–706.
Gray RJ . A class of k-sample tests for comparing the cumulative incidence of a competing risk. Ann Stat 1988; 16: 1141–1154.
Cox DR . Regression models and life-tables. J Roy Stat Soc B 1972; 34: 187–220.
Pereira A, Nomdedeu M, Aguilar JL, Belkaid M, Carrio A, Cobo F et al. Transfusion intensity, not the cumulative red blood cell transfusion burden, determines the prognosis of patients with myelodysplastic syndrome on chronic transfusion support. Am J Hematol 2010; 86: 245–250.
Patnaik MM, Lasho TL, Finke CM, Gangat N, Caramazza D, Holtan SG et al. WHO-defined ‘myelodysplastic syndrome with isolated del(5q)’ in 88 consecutive patients: survival data, leukemic transformation rates and prevalence of JAK2, MPL and IDH mutations. Leukemia 2010; 24: 1283–1289.
Mallo M, Cervera J, Schanz J, Such E, García-Manero G, Luño E et al. Impact of adjunct cytogenetic abnormalities for prognostic stratification in patients with myelodysplastic syndrome and deletion 5q. Leukemia 2011; 25: 110–120.
Haase D, Germing U, Schanz J, Pfeilstöcker M, Nösslinger T, Hildebrandt B et al. New insights into the prognostic impact of the karyotype in MDS and correlation with subtypes: evidence from a core dataset of 2124 patients. Blood 2007; 110: 4385–4395.
Evers C, Beier M, Poelitz A, Hildebrandt B, Servan K, Drechsler M et al. Molecular definition of chromosome arm 5q deletion end points and detection of hidden aberrations in patients with myelodysplastic syndromes and isolated del(5q) using oligonucleotide array CGH. Genes Chromosomes Cancer 2007; 46: 1119–1128.
Thiel A, Beier M, Ingenhag D, Servan K, Hein M, Moeller V et al. Comprehensive array CGH of normal karyotype myelodysplastic syndromes reveals hidden recurrent and individual genomic copy number alterations with prognostic relevance. Leukemia 2011; 25: 387–399.
Boultwood J, Pellagati A, McKenzie AN, Wainscout JS . Advances in the 5q-syndrome. Blood 2010; 116: 5803–5811.
Crescenzi B, La Starza R, Romoli S, Beacci D, Matteucci C, Barba G et al. Submicroscopic deletions in 5q- associated malignancies. Haematologica 2004; 89: 281–285.
Pellagatti A, Marafioti T, Paterson JC, Barlow JL, Drynan LF, Giagounidis A et al. Induction of p53 and up-regulation of the p53 pathway in the human 5q- syndrome. Blood 2010; 115: 2721–2723.
Fidler C, Watkins F, Bowen DT, Littlewood TJ, Wainscoat JS, Boultwood J . NRAS, FLT3 and TP53 mutations in patients with myelodysplastic syndrome and a del(5q). Haematologica 2004; 89: 865–866.
Jadersten M, Saft L, Pellagatti A, Göhring G, Wainscoat JS, Boultwood J et al. Clonal heterogeneity in the 5q-syndrome: p53 expressing progenitors prevail during lenalidomide treatment and expand at disease progression. Haematologica 2009; 94: 1762–1766.
Ades L, Lebras F, Sebert M, Kelaidi C, Lamy T, Dreyfus F et al. Treatment with Lenalidomide does not appear to increase the risk of leukemia progression in lower risk myelodysplastic syndrome with 5q deletion. A comparative analysis by the GFM. Haematologica 2011, (in press).
Gohring G, Giagounidis A, Busche G, Kreipe HH, Zimmermann M, Hellstrom-Lindberg E et al. Patients with del(5q) MDS who fail to achieve sustained erythroid or cytogenetic remission after treatment with lenalidomide have an increased risk for clonal evolution and AML progression. Ann Hematol 2010; 89: 365–374.
Neukirchen J, Blum S, Kuendgen A, Strupp C, Aivado M, Haas R et al. Platelet counts and haemorrhagic diathesis in patients with myelodysplastic syndromes. Eur J Haematol 2009; 83: 477–482.
Matsuda A, Germing U, Jinnai I, Misumi M, Kuendgen A, Knipp S et al Difference in clinical features between Japanese and German patients with refractory anemia in myelodysplastic syndromes. Blood 2005; 106: 2633–2640.
Wang H, Wang X, Xu X, Lin G . Cytogenetic features and prognosis analysis in Chinese patients with myelodysplastic syndrome: a multicenter study. Ann Hematol 2010; 89: 535–544.
Jung SW, Lee SY, Jekarl DW, Kim M, Lim J, Kim Y et al. Cytogenetic characteristics and prognosis analysis in 231 myelodysplastic syndrome patients from a single institution. Leuk Res 2011; 35: 735–740.
Lee HR, Oh B, Hong DS, Zang DY, Yoon HJ, Kim HJ et al. Cytogenetic features of 5q deletion and 5q- syndrome in myelodysplastic syndrome in Korea; marker chromosomes proved to be chromosome 5 with interstitial deletion by fluorescence in situ hybridization. Cancer Genet Cytogenet 2010; 203: 193–202.
List A, Dewald G, Bennett J, Giagounidis A, Raza A, Feldman E et al. Lenalidomide in the myelodysplastic syndrome with chromosome 5q deletion. New Engl J Med 2006; 355: 1456–1465.
Fenaux P, Giagounidis A, Selleslag D, Beyne-Rauzy O, Mufti G, Mittelman M et al. A randomized phase 3 study of lenalidomide versus placebo in RBC transfusion-dependent patients with Low-/Intermediate-1-risk myelodysplastic syndromes with del5q. Blood 2011; 118: 3765–3776.
Acknowledgements
This work was supported by Celgene.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
U Germing, P Fenaux, J Maciejewski, D Haase, U Platzbecker, KA Kreuzer and A Giagounidis are on the advisory board as well as have received research funding from Celgene. M Pfeilstöcker, T Nösslinger, M Sekeres, J Seymour, P Valent and A Kündgen are on the advisory board of Celgene. M Kenealy and R Weide have received research funding from Celgene.
Rights and permissions
About this article
Cite this article
Germing, U., Lauseker, M., Hildebrandt, B. et al. Survival, prognostic factors and rates of leukemic transformation in 381 untreated patients with MDS and del(5q): A multicenter study. Leukemia 26, 1286–1292 (2012). https://doi.org/10.1038/leu.2011.391
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2011.391
Keywords
This article is cited by
-
Mutation rates and fitness consequences of mosaic chromosomal alterations in blood
Nature Genetics (2023)
-
Lenalidomide treatment of Japanese patients with myelodysplastic syndromes with 5q deletion: a post-marketing surveillance study
International Journal of Hematology (2023)
-
Myelodysplastic syndromes with del(5q): A real-life study of determinants of long-term outcomes and response to lenalidomide
Blood Cancer Journal (2022)
-
Infiltration of thyroid papillary cancer tissue with myeloid leukemic cells: a case report
World Journal of Surgical Oncology (2021)
-
Genome-wide DNA methylation analysis pre- and post-lenalidomide treatment in patients with myelodysplastic syndrome with isolated deletion (5q)
Annals of Hematology (2021)