Abstract
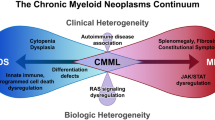
Acute leukemia with a mixed phenotype is a rare disease and comprises 2–5% of all acute leukemias. These disorders have been known historically by a variety of names, such as mixed lineage leukemia, bilineal leukemia and biphenotypic leukemia, and the criteria for diagnosis have often been arbitrary. The scoring criteria proposed by the European Group for the Immunological Characterization of Leukemias represented a major attempt to define this disorder. However, the relative weight given to some markers and the lack of lineage specificity of most markers have raised questions regarding the significance of this approach. In 2008, the World Health Organization classification of hematopoietic and lymphoid tumors proposed a simpler diagnostic algorithm, which relies on fewer and more lineage-specific markers to define mixed-phenotype acute leukemia (MPAL). MPAL with t(9;22) and MLL rearrangement have been separated. Several studies have suggested that patients with acute leukemia of mixed phenotype have a worse clinical outcome when compared with matched controls with acute myeloid leukemia or acute lymphoblastic leukemia. Further studies are needed to confirm the significance of MPAL as currently defined, to determine a standardized treatment approach and to better understand the biological and clinical aspects of this disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Weir EG, Borowitz MJ . Acute leukemias of ambiguous lineage. In: Jaffe ES, Harris NL, Vardiman JW, Campo E, Arber DA (eds). Hematopathology. Elsevier: Philadelphia, 2010.
Weir EG, Ali Ansari-Lari M, Batista DA, Griffin CA, Fuller S, Smith BD et al. Acute bilineal leukemia: a rare disease with poor outcome. Leukemia 2007; 21: 2264–2270.
Kita K, Nakase K, Miwa H, Masuya M, Nishii K, Morita N et al. Phenotypical characteristics of acute myelocytic leukemia associated with the t(8;21)(q22;q22) chromosomal abnormality: frequent expression of immature B-cell antigen CD19 together with stem cell antigen CD34. Blood 1992; 80: 470–477.
Hurwitz CA, Raimondi SC, Head D, Krance R, Mirro Jr J, Kalwinsky DK et al. Distinctive immunophenotypic features of t(8;21)(q22;q22) acute myeloblastic leukemia in children. Blood 1992; 80: 3182–3188.
Adriaansen HJ, te Boekhorst PA, Hagemeijer AM, van der Schoot CE, Delwel HR, van Dongen JJ . Acute myeloid leukemia M4 with bone marrow eosinophilia (M4Eo) and inv(16)(p13q22) exhibits a specific immunophenotype with CD2 expression. Blood 1993; 81: 3043–3051.
Khalidi HS, Medeiros LJ, Chang KL, Brynes RK, Slovak ML, Arber DA . The immunophenotype of adult acute myeloid leukemia: high frequency of lymphoid antigen expression and comparison of immunophenotype, French-American-British classification, and karyotypic abnormalities. Am J Clin Pathol 1998; 109: 211–220.
Khalidi HS, Chang KL, Medeiros LJ, Brynes RK, Slovak ML, Murata-Collins JL et al. Acute lymphoblastic leukemia. Survey of immunophenotype, French-American-British classification, frequency of myeloid antigen expression, and karyotypic abnormalities in 210 pediatric and adult cases. Am J Clin Pathol 1999; 111: 467–476.
Childs CC, Hirsch-Ginsberg C, Walters RS, Andersson BS, Reuben J, Trujillo JM et al. Myeloid surface antigen-positive acute lymphoblastic leukemia (My+ ALL): immunophenotypic, ultrastructural, cytogenetic, and molecular characteristics. Leukemia 1989; 3: 777–783.
Bene MC . Biphenotypic, bilineal, ambiguous or mixed lineage: strange leukemias!. Hematologica 2009; 94: 891–893.
McGraw TP, Folds JD, Bollum FJ, Strass SA . Terminal deoxynucleotidyl transferase-positive acute myeloblastic leukemia. Am J Hematol 1981; 10: 251–258.
Scamurra DO, Davey FR, Nelson DA, Kurec AS, Goldberg J . Acute leukemia presenting with myeloid and lymphoid cell markers. Ann Clin Lab Sci 198; 13: 396–502.
Mirro J, Zipf TF, Pui CH, Kitchingman G, Williams D, Melvin S et al. Acute mixed lineage leukemia: clinicopathologic correlation and prognostic significance. Blood 1985; 66: 1115–1123.
Catovsky D, Matutes E, Buccheri V, Shetty V, Hanslip J, Yoshida N et al. A classification of acute leukemia for the 1990s. Ann Hematol 1991; 62: 16–21.
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A et al. Proposals for the immunological classification of acute leukemias. European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia 1995; 9: 1783–1786.
Bene MC, Bernier M, Casasnovas RO, Castoldi G, Knapp W, Lanza F et al. The reliability and specificity of c-kit for the diagnosis of acute myeloid leukemias and undifferentiated leukemias. Blood 1998; 92: 596–599.
Jaffe E, Harris N, Stein HVJ, Vardiman JW (eds). Pathology and Genetics of Tumors of Hematopoietic and Lymphoid Tissues, 2nd printing, World Health Organization Classification of Tumours. IARC Press: Lyon, France, 2001.
Aribi A, Bueso-Ramos C, Estey E, Estrov Z, O’Brien S, Giles F et al. Biphenotypic acute leukaemia: a case series. Br J Haematol 2007; 138: 213–216.
Bagg A . Lineage ambiguity, infidelity, and promiscuity in immunophenotypically complex acute leukemias: genetic and morphologic correlates. Am J Clin Pathol 2007; 128: 545–548.
Valbuena JR, Medeiros LJ, Rassidakis GZ, Hao S, Wu CD, Chen L et al. Expression of B cell-specific activator protein/PAX5 in acute myeloid leukemia with t(8;21)(q22;q22). Am J Clin Pathol 2006; 126: 235–240.
Chapiro E, Delabesse E, Asnafi V, Millien C, Davi F, Nugent E et al. Expression of T-lineage-affiliated transcripts and TCR rearrangements in acute promyelocytic leukemia: implications for the cellular target of t(15;17). Blood 2006; 108: 3484–3493.
Hashimoto M, Yamashita Y, Mori N . Immunohistochemical detection of CD79a expression in precursor T cell lymphoblastic lymphoma/leukemias. J Pathol 2002; 197: 341–347.
Pilozzi E, Pulford K, Jones M, Müller-Hermelink HK, Falini B, Ralfkiaer E et al. Co-expression of CD79a (JCB117) and CD3 by lymphoblastic lymphoma. J Pathol 1998; 186: 140–143.
Arber DA, Jenkins KA, Slovak ML . CD79 alpha expression in acute myeloid leukemia. High frequency of expression in acute promyelocytic leukemia. Am J Pathol 1996; 149: 1105–1110.
Bhargava P, Kallakury BV, Ross JS, Azumi N, Bagg A . CD79a is heterogeneously expressed in neoplastic and normal myeloid precursors and megakaryocytes in an antibody clone-dependent manner. Am J Clin Pathol 2007; 128: 306–313.
Arber DA, Snyder DS, Fine M, Dagis A, Niland J, Slovak ML . Myeloperoxidase immunoreactivity in adult acute lymphoblastic leukemia. Am J Clin Pathol 2001; 116: 25–33.
Paietta E, Racevskis J, Bennett JM, Wiernik PH . Differential expression of terminal transferase (TdT) in acute lymphocytic leukaemia expressing myeloid antigens and TdT positive acute myeloid leukaemia as compared to myeloid antigen negative acute lymphocytic leukaemia. Br J Haematol 1993; 84: 416–422.
Borowitz MJ, Bene MC, Harris NL, Porwit A, Matutes E . Acute leukemias of ambiguous lineage. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW (eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press: Lyon, 2008, pp 150–155.
Khalidi HS, Brynes RK, Medeiros LJ, Chang KL, Slovak ML, Snyder DS et al. The immunophenotype of blast transformation of chronic myelogenous leukemia: a high frequency of mixed lineage phenotype in “lymphoid” blasts and a comparison of morphologic, immunophenotypic, and molecular findings. Mod Pathol 1998; 11: 1211–1221.
Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR et al. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med 1985; 103: 620–625.
Sevilla DW, Colovai AI, Emmons FN, Bhagat G, Alobeid B . Hematogones: a review and update. Leuk Lymphoma 2010; 51: 10–19.
Babusíková O, Zelezníková T, Kirschnerová G, Kankuri E . Hematogones in acute leukemia during and after therapy. Leuk Lymphoma 2008; 49: 1935–1944.
Rimsza LM, Larson RS, Winter SS, Foucar K, Chong YY, Garner KW et al. Benign hematogone-rich lymphoid proliferations can be distinguished from B-lineage acute lymphoblastic leukemia by integration of morphology, immunophenotype, adhesion molecule expression, and architectural features. Am J Clin Pathol 2000; 114: 66–75.
Al-Seraihy AS, Owaidah TM, Ayas M, El-Solh H, Al-Mahr M, Al-Ahmari A et al. Clinical characteristics and outcome of children with biphenotypic acute leukemia. Haematologica 2009; 94: 1682–1690.
Killick S, Matutes E, Powles RL, Hamblin M, Swansbury J, Treleaven JG et al. Outcome of biphenotypic acute leukemia. Haematologica 1999; 84: 699–706.
Owaidah TM, Al Beihany A, Iqbal MA, Elkum N, Roberts GT . Cytogenetics, molecular and ultrastructural characteristics of biphenotypic acute leukemia identified by the EGIL scoring system. Leukemia 2006; 20: 620–626.
Xu XQ, Wang JM, Lü SQ, Chen L, Yang JM, Zhang WP et al. Clinical and biological characteristics of adult biphenotypic acute leukemia in comparison with that of acute myeloid leukemia and acute lymphoblastic leukemia: a case series of a Chinese population. Haematologica 2009; 94: 919–927.
Thalhammer-Scherrer R, Mitterbauer G, Simonitsch I, Jaeger U, Lechner K, Schneider B et al. The immunophenotype of 325 adult acute leukemias: relationship to morphologic and molecular classification and proposal for a minimal screening program highly predictive for lineage discrimination. Am J Clin Pathol 2002; 117: 380–389.
Rubnitz JE, Onciu M, Pounds S, Shurtleff S, Cao X, Raimondi SC et al. Acute mixed lineage leukemia in children: the experience of St Jude Children's Research Hospital. Blood 2009; 113: 5083–5089.
Lee JH, Min YH, Chung CW, Kim BK, Yoon HJ, Jo DY et al. Prognostic implications of the immunophenotype in biphenotypic acute leukemia. Leuk Lymphoma 2008; 49: 700–709.
Legrand O, Perrot JY, Simonin G, Baudard M, Cadiou M, Blanc C et al. Adult biphenotypic acute leukaemia: an entity with poor prognosis which is related to unfavourable cytogenetics and P-glycoprotein over-expression. Br J Haematol 1998; 100: 147–155.
Wouters BJ, Koss C, Delwel R . Gene expression profiling for improved dissection of acute leukemia: a recently identified immature myeloid/T-lymphoid subgroup as an example. Blood Cells Mol Dis 2008; 40: 395–400.
Buccheri V, Matutes E, Dyer MJS, Catovsky D . Lineage commitment in biphenotypic acute leukemia. Leukemia 1993; 7: 919–927.
Dupret C, Asnafi V, Leboeuf D, Millien C, Ben Abdelali R, Preudhomme C et al. IgH/TCR rearrangements are common in MLL translocated adult AML and suggest an early T/myeloid or B/myeloid maturation arrest, which correlates with the MLL partner. Leukemia 2005; 19: 2337–2338.
Zheng C, Wu J, Liu X, Ding K, Cai X, Zhu W . What is the optimal treatment for biphenotypic acute leukemia? Haematologica 2009; 94: 1778–1780.
Pui C-H, Sandlund JT, Pei D, Campana D, Rivera GK, Ribeiro RC et al. Improved outcome for children with acute lymphoblastic leukemia: results of Total Therapy Study XIIIB at St. Jude Children's Research Hospital. Blood 2004; 104: 2690–2696.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Weinberg, O., Arber, D. Mixed-phenotype acute leukemia: historical overview and a new definition. Leukemia 24, 1844–1851 (2010). https://doi.org/10.1038/leu.2010.202
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2010.202
Keywords
This article is cited by
-
Successful treatment of a B/T MPAL patient by chemo-free treatment with venetoclax, azacitidine, and blinatumomab
Annals of Hematology (2024)
-
Superior sagittal sinus thrombosis in the course of mixed phenotype acute leukaemia treated with acute lymphoblastic leukaemia-like therapy—a case report
Thrombosis Journal (2023)
-
A pro B cell population forms the apex of the leukemic hierarchy in Hoxa9/Meis1-dependent AML
Leukemia (2023)
-
The Role of PHF6 in Hematopoiesis and Hematologic Malignancies
Stem Cell Reviews and Reports (2023)
-
Multicenter retrospective analysis of clinical outcome of adult patients with mixed-phenotype acute leukemia treated with acute myeloid leukemia–like or acute lymphoblastic leukemia–like chemotherapy and impact of allogeneic stem cell transplantation: a Campus ALL study
Annals of Hematology (2023)