Abstract
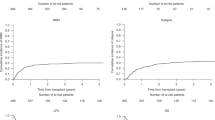
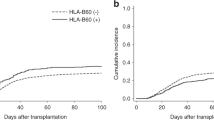
Disease stage and recipient/donor human leukocyte antigen (HLA) matching are important determinants of outcome in transplantation using volunteer-unrelated donors (VUD). Matching for HLA-A, -B, -C, -DRB1, -DQB1 is beneficial, whereas the importance of DPB1 matching is more controversial. The impact of HLA matching status may differ dependent on disease stage. We investigated the outcome according to the degree of HLA matching at 6 loci, in 488 recipients of predominantly T-cell depleted bone marrow VUD transplants for leukaemia. Survival was significantly better in 12/12-matched transplants in those with early leukaemia (5 years: 63 versus 41% in 10/10 matched, P=0.006), but not late stage disease. Conversely, within the HLA-mismatched group (⩽9/10), there was a significant survival advantage to DPB1 mismatching (5 years: 39 versus 21% in DPB1 matched, P=0.008), particularly in late leukaemia (P=0.01), persisting in multivariate analysis (odds ratio 0.478; 95% confidence interval 0.30, 0.75; P=0.001). These novel findings suggest that the best outcome for patients with early leukaemia, with a 10/10-matched donor, is achieved by matching for DPB1. Conversely, our results suggest that in patients receiving an HLA-mismatched graft, the outcome is significantly better if they are also mismatched for DPB1. We recommend validation of these results in independent datasets.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Flomenberg N, Baxter-Lowe LA, Confer D, Fernandez-Vina M, Filipovich A, Horowitz M et al. Impact of HLA class I and class II high-resolution matching on outcomes of unrelated donor bone marrow transplantation: HLA-C mismatching is associated with a strong adverse effect on transplantation outcome. Blood 2004; 104: 1923–1930.
Lee SJ, Klein J, Haagenson M, Baxter-Lowe LA, Confer DL, Eapen M et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood 2007; 110: 4576–4583.
Morishima Y, Sasazuki T, Inoko H, Juji T, Akaza T, Yamamoto K et al. The clinical significance of human leukocyte antigen (HLA) allele compatibility in patients receiving a marrow transplant from serologically HLA-A, HLA-B, and HLA-DR matched unrelated donors. Blood 2002; 99: 4200–4206.
Morishima Y, Yabe T, Matsuo K, Kashiwase K, Inoko H, Saji H et al. Effects of HLA allele and killer immunoglobulin-like receptor ligand matching on clinical outcome in leukemia patients undergoing transplantation with T-cell-replete marrow from an unrelated donor. Biol Blood Marrow Transplant 2007; 13: 315–328.
Keever-Taylor CA, Bredeson C, Loberiza FR, Casper JT, Lawton C, Rizzo D et al. Analysis of risk factors for the development of GVHD after T cell-depleted allogeneic BMT: effect of HLA disparity, ABO incompatibility, and method of T-cell depletion. Biol Blood Marrow Transplant 2001; 7: 620–630.
Petersdorf EW, Anasetti C, Martin PJ, Gooley T, Radich J, Malkki M et al. Limits of HLA mismatching in unrelated hematopoietic cell transplantation. Blood 2004; 104: 2976–2980.
Shaw BE, Russell NH, Devereux S, Das-Gupta E, Mackinnon S, Madrigal JA et al. The impact of donor factors on primary non-engraftment in recipients of reduced intensity conditioned transplants from unrelated donors. Haematologica 2005; 90: 1562–1569.
Kawase T, Morishima Y, Matsuo K, Kashiwase K, Inoko H, Saji H et al. High-risk HLA allele mismatch combinations responsible for severe acute graft-versus-host disease and implication for its molecular mechanism. Blood 2007; 110: 2235–2241.
Shaw BE, Gooley TA, Malkki M, Madrigal JA, Begovich AB, Horowitz MM et al. The importance of HLA-DPB1 in unrelated donor hematopoietic cell transplantation. Blood 2007; 110: 4560–4566.
Shaw BE, Marsh SG, Mayor NP, Russell NH, Madrigal JA . HLA-DPB1 matching status has significant implications for recipients of unrelated donor stem cell transplants. Blood 2006; 107: 1220–1226.
Loiseau P, Esperou H, Busson M, Sghiri R, Tamouza R, Hilarius M et al. DPB1 disparities contribute to severe GVHD and reduced patient survival after unrelated donor bone marrow transplantation. Bone Marrow Transplant 2002; 30: 497–502.
Fleischhauer K, Zino E, Mazzi B, Sironi E, Servida P, Zappone E et al. Peripheral blood stem cell allograft rejection mediated by CD4(+) T lymphocytes recognizing a single mismatch at HLA-DP beta 1*0901. Blood 2001; 98: 1122–1126.
Gaschet J, Gallot G, Ibisch C, Lim A, Even J, Vivien R et al. Acute graft-versus-host disease after bone marrow transplantation with a single HLA-DPB1*1001 mismatch: involvement of different TCRBV subsets. Bone Marrow Transplant 1998; 22: 385–392.
Ibisch C, Gallot G, Vivien R, Diez E, Jotereau F, Garand R et al. Recognition of leukemic blasts by HLA-DPB1-specific cytotoxic T cell clones: a perspective for adjuvant immunotherapy post-bone marrow transplantation. Bone Marrow Transplant 1999; 23: 1153–1159.
Rutten CE, van Luxemburg-Heijs SA, Griffioen M, Marijt EW, Jedema I, Heemskerk MH et al. HLA-DP as specific target for cellular immunotherapy in HLA class II-expressing B-cell leukemia. Leukemia 2008; 22: 1387–1394.
Valdes AM, McWeeney SK, Meyer D, Nelson MP, Thomson G . Locus and population specific evolution in HLA class II genes. Ann Hum Genet 1999; 63 (Part 1): 27–43.
Hollenbach JA, Thomson G, Cao K, Fernandez-Vina M, Erlich HA, Bugawan TL et al. HLA diversity, differentiation, and haplotype evolution in Mesoamerican natives. Hum Immunol 2001; 62: 378–390.
Tiercy JM, Nicoloso G, Passweg J, Schanz U, Seger R, Chalandon Y et al. The probability of identifying a 10/10 HLA allele-matched unrelated donor is highly predictable. Bone Marrow Transplant 2007; 40: 515–522.
Hurley CK, Baxter-Lowe LA, Begovich AB, Fernandez-Vina M, Noreen H, Schmeckpeper B et al. The extent of HLA class II allele level disparity in unrelated bone marrow transplantation: analysis of 1259 National Marrow Donor Program donor-recipient pairs. Bone Marrow Transplant 2000; 25: 385–393.
Petersdorf EW, Gooley T, Malkki M, Anasetti C, Martin P, Woolfrey A et al. The biological significance of HLA-DP gene variation in haematopoietic cell transplantation. Br J Haematol 2001; 112: 988–994.
Rodriguez T, Mendez R, Del Campo A, Aptsiauri N, Martin J, Orozco G et al. Patterns of constitutive and IFN-gamma inducible expression of HLA class II molecules in human melanoma cell lines. Immunogenetics 2007; 59: 123–133.
Shaw S, Johnson AH, Shearer GM . Evidence for a new segregant series of B cell antigens that are encoded in the HLA-D region and that stimulate secondary allogenic proliferative and cytotoxic responses. J Exp Med 1980; 152: 565–580.
Laux G, Mansmann U, Deufel A, Opelz G, Mytilineos J . A new epitope-based HLA-DPB matching approach for cadaver kidney retransplants. Transplantation 2003; 75: 1527–1532.
de Koster HS, Anderson DC, Termijtelen A . T cells sensitized to synthetic HLA-DR3 peptide give evidence of continuous presentation of denatured HLA-DR3 molecules by HLA-DP. J Exp Med 1989; 169: 1191–1196.
Essaket S, Fabron J, de Preval C, Thomsen M . Corecognition of HLA-A1 and HLA-DPw3 by a human CD4+ alloreactive T lymphocyte clone. J Exp Med 1990; 172: 387–390.
Zino E, Frumento G, Marktel S, Sormani MP, Ficara F, Di Terlizzi S et al. A T-cell epitope encoded by a subset of HLA-DPB1 alleles determines nonpermissive mismatches for hematologic stem cell transplantation. Blood 2004; 103: 1417–1424.
Shaw BE, Marsh SGE, Mayor NP, Madrigal JA . Matching status at amino acid positions 57 and 65 of the HLA–DPB1 beta chain determines outcome in recipients of Unrelated Donor Haematopoietic Stem Cell Transplants (abstract). Blood 2004; 104: 827.
Zino E, Vago L, Di Terlizzi S, Mazzi B, Zito L, Sironi E et al. Frequency and targeted detection of HLA-DPB1T cell epitope disparities relevant in unrelated hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2007; 13: 1031–1040.
Crocchiolo R, Zino E, Vago L, Oneto R, Bruno B, Pollichieni S et al. Nonpermissive HLA-DPB1 disparity is a significant independent risk factor for mortality after unrelated hematopoietic stem cell transplantation. Blood 2009; 114: 1437–1444.
Kawase T, Matsuo K, Kashiwase K, Inoko H, Saji H, Ogawa S et al. HLA mismatch combinations associated with decreased risk of relapse: implications for the molecular mechanism. Blood 2009; 113: 2851–2858.
Ludajic K, Balavarca Y, Bickeboller H, Pohlreich D, Kouba M, Dobrovolna M et al. Impact of HLA-DPB1 allelic and single amino acid mismatches on HSCT. Br J Haematol 2008; 142: 436–443.
Shaw BE, Potter MN, Mayor NP, Pay AL, Smith C, Goldman JM et al. The degree of matching at HLA-DPB1 predicts for acute graft-versus-host disease and disease relapse following haematopoietic stem cell transplantation. Bone Marrow Transplant 2003; 31: 1001–1008.
Acknowledgements
We thank all of the UK transplant teams who have contributed patient's data and samples to this study. We thank Andrew Howman for helpful comments on the manuscript. We also acknowledge valuable support from the European Union-FP6 project Allostem 503319 and the Immunobiology Working Party of the EBMT.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authorship statement
All authors were involved in the drafting of the article or critical revision for important intellectual content. BS, NM, NR, AML, SGEM and JAM were involved, in addition, in the conception and design or analysis and interpretation of the data.
Rights and permissions
About this article
Cite this article
Shaw, B., Mayor, N., Russell, N. et al. Diverging effects of HLA–DPB1 matching status on outcome following unrelated donor transplantation depending on disease stage and the degree of matching for other HLA alleles. Leukemia 24, 58–65 (2010). https://doi.org/10.1038/leu.2009.239
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2009.239
Keywords
This article is cited by
-
The impact of HLA donor-specific antibodies on engraftment and the evolving desensitization strategies
Bone Marrow Transplantation (2022)
-
HLA-DPB1 mismatch reduce relapse and improve survival in T-cell replete unrelated donor allogeneic stem cell transplantation
Bone Marrow Transplantation (2020)
-
HLA-DPB1 mismatch induces a graft-versus-leukemia effect without severe acute GVHD after single-unit umbilical cord blood transplantation
Leukemia (2018)
-
Recipient/donor HLA and CMV matching in recipients of T-cell-depleted unrelated donor haematopoietic cell transplants
Bone Marrow Transplantation (2017)
-
Directionality of non-permissive HLA-DPB1 T-cell epitope group mismatches does not improve clinical risk stratification in 8/8 matched unrelated donor hematopoietic cell transplantation
Bone Marrow Transplantation (2017)