Abstract
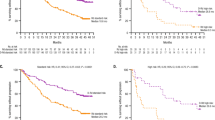
We present a pooled update of two large, multicenter MM-009 and MM-010 placebo-controlled randomized phase III trials that included 704 patients and assessed lenalidomide plus dexamethasone versus dexamethasone plus placebo in patients with relapsed/refractory multiple myeloma (MM). Patients in both studies were randomized to receive 25 mg daily oral lenalidomide or identical placebo, plus 40 mg oral dexamethasone. In this pooled analysis, using data up to unblinding (June 2005 for MM-009 and August 2005 for MM-010), treatment with lenalidomide plus dexamethasone significantly improved overall response (60.6 vs 21.9%, P<0.001), complete response rate (15.0 vs 2.0%, P<0.001), time to progression (median of 13.4 vs 4.6 months, P<0.001) and duration of response (median of 15.8 months vs 7 months, P<0.001) compared with dexamethasone-placebo. At a median follow-up of 48 months for surviving patients, using data up to July 2008, a significant benefit in overall survival (median of 38.0 vs 31.6 months, P=0.045) was retained despite 47.6% of patients who were randomized to dexamethasone-placebo receiving lenalidomide-based treatment after disease progression or study unblinding. Low β2-microglobulin and low bone marrow plasmacytosis were associated with longer survival. In conclusion, these data confirm the significant response and survival benefit with lenalidomide and dexamethasone.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Piazza FA, Gurrieri C, Trentin L, Semenzato G . Towards a new age in the treatment of multiple myeloma. Ann Hematol 2007; 86: 159–172.
Kyle RA, Gertz MA, Witzig TE, Lust JA, Lacy MQ, Dispenzieri A et al. Review of 1027 patients with newly diagnosed multiple myeloma. Mayo Clin Proc 2003; 78: 21–33.
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T et al. Cancer statistics, 2008. CA Cancer J Clin 2008; 58: 71–96.
Facon T, Mary JY, Hulin C, Benboubker L, Attal M, Pegourie B et al. Melphalan and prednisone plus thalidomide versus melphalan and prednisone alone or reduced-intensity autologous stem cell transplantation in elderly patients with multiple myeloma (IFM 99-06): a randomised trial. Lancet 2007; 370: 1209–1218.
Richardson PG, Sonneveld P, Schuster MW, Irwin D, Stadtmauer EA, Facon T et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med 2005; 352: 2487–2498.
Dimopoulos MA, Spencer A, Attal M, Prince HM, Harousseau JC, Dmoszynska A et al. Multiple Myeloma (010) study investigators. Lenalidomide plus dexamethasone for relapsed or refractory multiple myeloma. N Engl J Med 2007; 357: 2123–2132.
Weber DM, Chen C, Niesvizky R, Wang M, Belch A, Stadtmauer EA et al. Multiple Myeloma (009) study investigators. Lenalidomide plus dexamethasone for relapsed multiple myeloma in North America. N Engl J Med 2007; 357: 2133–2142.
Kumar SK, Rajkumar V, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK et al. Improved survival in multiple myeloma and the impact of novel therapies. Blood 2008; 111: 2516–2520.
Richardson PG, Mitsiades C, Hideshima T, Anderson KC . Lenalidomide in multiple myeloma. Expert Rev Anticancer Ther 2006; 6: 1165–1173.
Kastritis E, Dimopoulos MA . The evolving role of lenalidomide in the treatment of hematologic malignancies. Expert Opin Pharmacother 2007; 8: 497–509.
Thomas SK, Richards TA, Weber DM . Lenalidomide in multiple myeloma. Best Pract Res Clin Haematol 2007; 20: 717–735.
Richardson PG, Schlossman RL, Weller E, Hideshima T, Mitsiades C, Davies F et al. Immunomodulatory drug CC-5013 overcomes drug resistance and is well tolerated in patients with relapsed multiple myeloma. Blood 2002; 100: 3063–3067.
Richardson PG, Blood E, Mitsiades CS, Jagannath S, Zeldenrust SR, Alsina M et al. A randomized phase 2 study of lenalidomide therapy for patients with relapsed or relapsed and refractory multiple myeloma. Blood 2006; 108: 3458–3464.
Bladé J, Samson D, Reece D, Apperley J, Björkstrand B, Gahrton G et al. Criteria for evaluating disease response and progression in patients with multiple myeloma treated by high-dose therapy and haemopoietic stem cell transplantation. Myeloma Subcommittee of the EBMT. European Group for Blood and Marrow Transplant. Br J Haematol 1998; 102: 1115–1123.
Stadtmauer EA, Weber DM, Niesvizky R, Belch A, Prince PH, San Miguel JF et al. Lenalidomide in combination with dexamethasone at first relapse in comparison with its use as later salvage therapy in relapsed or refractory multiple myeloma. Eur J Haematol 2009; 82: 426–432.
San Miguel JF, Schlag R, Khuageva NK, Dimopoulos MA, Shpilberg O, Kropff M et al. Bortezomib plus melphalan and prednisone for initial treatment for multiple myeloma. N Engl J Med 2008; 359: 906–917.
Rajkumar SV, Jacobus S, Callander N, Fonseca R, Vesole D, Williams M et al. Phase III trial of lenalidomide plus high-dose dexamethasone versus lenalidomide plus low-dose dexamethasone in newly diagnosed multiple myeloma (E4A03): a trial coordinated by the Eastern cooperative oncology group. J Clin Oncol 2007; 25, Abstract LBA8025.
Zonder JA, Crowley J, Hussein MA, Bolejack V, Moore DF, Whittenberger BF et al. Superiority of Lenalidomide (Len) Plus High-Dose Dexamethasone (HD) Compared to HD Alone as Treatment of Newly-Diagnosed Multiple Myeloma (NDMM): results of the randomized, double-blinded, placebo-controlled SWOG Trial S0232. Blood 2007; 110, Abstract 77.
Acknowledgements
We received editorial support in the preparation of this article, funded by Celgene. We, however, were fully responsible for content and editorial decisions for this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dimopoulos, M., Chen, C., Spencer, A. et al. Long-term follow-up on overall survival from the MM-009 and MM-010 phase III trials of lenalidomide plus dexamethasone in patients with relapsed or refractory multiple myeloma. Leukemia 23, 2147–2152 (2009). https://doi.org/10.1038/leu.2009.147
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2009.147
Keywords
This article is cited by
-
Cardiac toxicities in multiple myeloma: an updated and a deeper look into the effect of different medications and novel therapies
Blood Cancer Journal (2023)
-
Thrombosis events in Chinese patients with newly diagnosed multiple myeloma
Clinical and Experimental Medicine (2023)
-
Cost utility and budget impact analysis of dexamethasone compared with bortezomib and lenalidomide for the treatment of second line multiple myeloma from a South African public health perspective
Cost Effectiveness and Resource Allocation (2022)
-
Oral ixazomib-dexamethasone vs oral pomalidomide-dexamethasone for lenalidomide-refractory, proteasome inhibitor-exposed multiple myeloma: a randomized Phase 2 trial
Blood Cancer Journal (2022)
-
Thromboembolic events and thromboprophylaxis associated with immunomodulators in multiple myeloma patients: a real-life study
Journal of Cancer Research and Clinical Oncology (2022)