Abstract
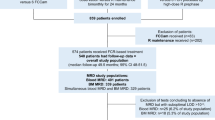
Detection of minimal residual disease (MRD) is the most sensitive method to evaluate treatment response and one of the strongest predictors of outcome in childhood acute lymphoblastic leukemia (ALL). The 10-year update on the I-BFM-SG MRD study 91 demonstrates stable results (event-free survival), that is, standard risk group (MRD-SR) 93%, intermediate risk group (MRD-IR) 74%, and high risk group (MRD-HR) 16%. In multicenter trial AIEOP-BFM ALL 2000, patients were stratified by MRD detection using quantitative PCR after induction (TP1) and consolidation treatment (TP2). From 1 July 2000 to 31 October 2004, PCR target identification was performed in 3341 patients: 2365 (71%) patients had two or more sensitive targets (⩽10−4), 671 (20%) patients revealed only one sensitive target, 217 (6%) patients had targets with lower sensitivity, and 88 (3%) patients had no targets. MRD-based risk group assignment was feasible in 2594 (78%) patients: 40% were classified as MRD-SR (two sensitive targets, MRD negativity at both time points), 8% as MRD-HR (MRD ⩾10−3 at TP2), and 52% as MRD-IR. The remaining 823 patients were stratified according to clinical risk features: HR (n=108) and IR (n=715). In conclusion, MRD-PCR-based stratification using stringent criteria is feasible in almost 80% of patients in an international multicenter trial.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Conter V, Arico M, Valsecchi MG, Basso G, Biondi A, Madon E et al. Long-term results of the Italian Association of Pediatric Hematology and Oncology (AIEOP) acute lymphoblastic leukemia studies, 1982–1995. Leukemia 2000; 14: 2196–2204.
Schrappe M, Reiter A, Zimmermann M, Harbott J, Ludwig WD, Henze G et al. Long-term results of four consecutive trials in childhood ALL performed by the ALL-BFM study group from 1981 to 1995. Berlin–Frankfurt–Munster. Leukemia 2000; 14: 2205–2222.
Gaynon PS, Trigg ME, Heerema NA, Sensel MG, Sather HN, Hammond GD et al. Children's Cancer Group trials in childhood acute lymphoblastic leukemia: 1983–1995. Leukemia 2000; 14: 2223–2233.
Kamps WA, Veerman AJ, van Wering ER, van Weerden JF, Slater R, van der Does-van den Berg A . Long-term follow-up of Dutch Childhood Leukemia Study Group (DCLSG) protocols for children with acute lymphoblastic leukemia, 1984–1991. Leukemia 2000; 14: 2240–2246.
Silverman LB, Declerck L, Gelber RD, Dalton VK, Asselin BL, Barr RD et al. Results of Dana-Farber Cancer Institute Consortium protocols for children with newly diagnosed acute lymphoblastic leukemia (1981–1995). Leukemia 2000; 14: 2247–2256.
Vilmer E, Suciu S, Ferster A, Bertrand Y, Cave H, Thyss A et al. Long-term results of three randomized trials (58831, 58832, 58881) in childhood acute lymphoblastic leukemia: a CLCG-EORTC report. Children Leukemia Cooperative Group. Leukemia 2000; 14: 2257–2266.
Gustafsson G, Schmiegelow K, Forestier E, Clausen N, Glomstein A, Jonmundsson G et al. Improving outcome through two decades in childhood ALL in the Nordic countries: the impact of high-dose methotrexate in the reduction of CNS irradiation. Nordic Society of Pediatric Haematology and Oncology (NOPHO). Leukemia 2000; 14: 2267–2275.
Maloney KW, Shuster JJ, Murphy S, Pullen J, Camitta BA . Long-term results of treatment studies for childhood acute lymphoblastic leukemia: Pediatric Oncology Group studies from 1986–1994. Leukemia 2000; 14: 2276–2285.
Pui CH, Boyett JM, Rivera GK, Hancock ML, Sandlund JT, Ribeiro RC et al. Long-term results of Total Therapy studies 11, 12 and 13A for childhood acute lymphoblastic leukemia at St Jude Children's Research Hospital. Leukemia 2000; 14: 2286–2294.
Eden OB, Harrison G, Richards S, Lilleyman JS, Bailey CC, Chessells JM et al. Long-term follow-up of the United Kingdom Medical Research Council protocols for childhood acute lymphoblastic leukaemia, 1980–1997. Medical Research Council Childhood Leukaemia Working Party. Leukemia 2000; 14: 2307–2320.
Schrappe M, Reiter A, Ludwig WD, Harbott J, Zimmermann M, Hiddemann W et al. Improved outcome in childhood acute lymphoblastic leukemia despite reduced use of anthracyclines and cranial radiotherapy: results of trial ALL-BFM 90. German-Austrian-Swiss ALL-BFM Study Group. Blood 2000; 95: 3310–3322.
Szczepanski T . Why and how to quantify minimal residual disease in acute lymphoblastic leukemia? Leukemia 2007; 21: 622–626.
Cazzaniga G, Biondi A . Molecular monitoring of childhood acute lymphoblastic leukemia using antigen receptor gene rearrangements and quantitative polymerase chain reaction technology. Haematologica 2005; 90: 382–390.
Szczepanski T, Flohr T, van der Velden VH, Bartram CR, van Dongen JJ . Molecular monitoring of residual disease using antigen receptor genes in childhood acute lymphoblastic leukaemia. Best Pract Res Clin Haematol 2002; 15: 37–57.
Bruggemann M, Raff T, Flohr T, Gokbuget N, Nakao M, Droese J et al. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lymphoblastic leukemia. Blood 2006; 107: 1116–1123.
Marshall GM, Haber M, Kwan E, Zhu L, Ferrara D, Xue C et al. Importance of minimal residual disease testing during the second year of therapy for children with acute lymphoblastic leukemia. J Clin Oncol 2003; 21: 704–709.
Panzer-Grumayer ER, Schneider M, Panzer S, Fasching K, Gadner H . Rapid molecular response during early induction chemotherapy predicts a good outcome in childhood acute lymphoblastic leukemia. Blood 2000; 95: 790–794.
Coustan-Smith E, Sancho J, Hancock ML, Boyett JM, Behm FG, Raimondi SC et al. Clinical importance of minimal residual disease in childhood acute lymphoblastic leukemia. Blood 2000; 96: 2691–2696.
Foroni L, Harrison CJ, Hoffbrand AV, Potter MN . Investigation of minimal residual disease in childhood and adult acute lymphoblastic leukaemia by molecular analysis. Br J Haematol 1999; 105: 7–24.
Cave H, van der Werff ten Bosch J, Suciu S, Guidal C, Waterkeyn C, Otten J et al. Clinical significance of minimal residual disease in childhood acute lymphoblastic leukemia. European Organization for Research and Treatment of Cancer—Childhood Leukemia Cooperative Group. N Engl J Med 1998; 339: 591–598.
Steenbergen EJ, Verhagen OJ, van Leeuwen EF, van den Berg H, Behrendt H, Slater RM et al. Prolonged persistence of PCR-detectable minimal residual disease after diagnosis or first relapse predicts poor outcome in childhood B-precursor acute lymphoblastic leukemia. Leukemia 1995; 9: 1726–1734.
Brisco MJ, Condon J, Hughes E, Neoh SH, Sykes PJ, Seshadri R et al. Outcome prediction in childhood acute lymphoblastic leukaemia by molecular quantification of residual disease at the end of induction. Lancet 1994; 343: 196–200.
van Dongen JJ, Seriu T, Panzer-Grumayer ER, Biondi A, Pongers-Willemse MJ, Corral L et al. Prognostic value of minimal residual disease in acute lymphoblastic leukaemia in childhood. Lancet 1998; 352: 1731–1738.
Bene MC, Castoldi G, Knapp W, Ludwig WD, Matutes E, Orfao A et al. Proposals for the immunological classification of acute leukemias. European Group for the Immunological Characterization of Leukemias (EGIL). Leukemia 1995; 9: 1783–1786.
Viehmann S, Borkhardt A, Lampert F, Harbott J . Multiplex PCR—a rapid screening method for detection of gene rearrangements in childhood acute lymphoblastic leukemia. Ann Hematol 1999; 78: 157–162.
Verhagen OJ, Wijkhuijs AJ, van der Sluijs-Gelling AJ, Szczepanski T, van der Linden-Schrever BE, Pongers-Willemse MJ et al. Suitable DNA isolation method for the detection of minimal residual disease by PCR techniques. Leukemia 1999; 13: 1298–1299.
van der Velden VH, Hochhaus A, Cazzaniga G, Szczepanski T, Gabert J, van Dongen JJ . Detection of minimal residual disease in hematologic malignancies by real-time quantitative PCR: principles, approaches, and laboratory aspects. Leukemia 2003; 17: 1013–1034.
Pongers-Willemse MJ, Seriu T, Stolz F, d'Aniello E, Gameiro P, Pisa P et al. Primers and protocols for standardized detection of minimal residual disease in acute lymphoblastic leukemia using immunoglobulin and T cell receptor gene rearrangements and TAL1 deletions as PCR targets: report of the BIOMED-1 CONCERTED ACTION: investigation of minimal residual disease in acute leukemia. Leukemia 1999; 13: 110–118.
Szczepanski T, Willemse MJ, van Wering ER, van Weerden JF, Kamps WA, van Dongen JJ . Precursor-B-ALL with D(H)-J(H) gene rearrangements have an immature immunogenotype with a high frequency of oligoclonality and hyperdiploidy of chromosome 14. Leukemia 2001; 15: 1415–1423.
Szczepanski T, Pongers-Willemse MJ, Langerak AW, Harts WA, Wijkhuijs AJ, van Wering ER et al. Ig heavy chain gene rearrangements in T-cell acute lymphoblastic leukemia exhibit predominant DH6-19 and DH7-27 gene usage, can result in complete V-D-J rearrangements, and are rare in T-cell receptor alpha beta lineage. Blood 1999; 93: 4079–4085.
Breit TM, Beishuizen A, Ludwig WD, Mol EJ, Adriaansen HJ, van Wering ER et al. tal-1 deletions in T-cell acute lymphoblastic leukemia as PCR target for detection of minimal residual disease. Leukemia 1993; 7: 2004–2011.
van Dongen JJ, Langerak AW, Bruggemann M, Evans PA, Hummel M, Lavender FL et al. Design and standardization of PCR primers and protocols for detection of clonal immunoglobulin and T-cell receptor gene recombinations in suspect lymphoproliferations: report of the BIOMED-2 Concerted Action BMH4-CT98-3936. Leukemia 2003; 17: 2257–2317.
Langerak AW, Szczepanski T, van der Burg M, Wolvers-Tettero IL, van Dongen JJ . Heteroduplex PCR analysis of rearranged T cell receptor genes for clonality assessment in suspect T cell proliferations. Leukemia 1997; 11: 2192–2199.
Nakao M, Janssen JW, Flohr T, Bartram CR . Rapid and reliable quantification of minimal residual disease in acute lymphoblastic leukemia using rearranged immunoglobulin and T-cell receptor loci by LightCycler technology. Cancer Res 2000; 60: 3281–3289.
Pongers-Willemse MJ, Verhagen OJ, Tibbe GJ, Wijkhuijs AJ, de Haas V, Roovers E et al. Real-time quantitative PCR for the detection of minimal residual disease in acute lymphoblastic leukemia using junctional region specific TaqMan probes. Leukemia 1998; 12: 2006–2014.
van der Velden VH, Panzer-Grumayer ER, Cazzaniga G, Flohr T, Sutton R, Schrauder A et al. Optimization of PCR-based minimal residual disease diagnostics for childhood acute lymphoblastic leukemia in a multi-center setting. Leukemia 2007; 21: 706–713.
van der Velden VH, Cazzaniga G, Schrauder A, Hancock J, Bader P, Panzer-Grumayer ER et al. Analysis of minimal residual disease by Ig/TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia 2007; 21: 604–611.
Burger B, Zimmermann M, Mann G, Kuhl J, Loning L, Riehm H et al. Diagnostic cerebrospinal fluid examination in children with acute lymphoblastic leukemia: significance of low leukocyte counts with blasts or traumatic lumbar puncture. J Clin Oncol 2003; 21: 184–188.
Arico M, Valsecchi MG, Conter V, Rizzari C, Pession A, Messina C et al. Improved outcome in high-risk childhood acute lymphoblastic leukemia defined by prednisone-poor response treated with double Berlin-Frankfurt-Muenster protocol II. Blood 2002; 100: 420–426.
Gruhn B, Hongeng S, Yi H, Hancock ML, Rubnitz JE, Neale GA et al. Minimal residual disease after intensive induction therapy in childhood acute lymphoblastic leukemia predicts outcome. Leukemia 1998; 12: 675–681.
Nyvold C, Madsen HO, Ryder LP, Seyfarth J, Svejgaard A, Clausen N et al. Precise quantification of minimal residual disease at day 29 allows identification of children with acute lymphoblastic leukemia and an excellent outcome. Blood 2002; 99: 1253–1258.
Coustan-Smith E, Behm FG, Sanchez J, Boyett JM, Hancock ML, Raimondi SC et al. Immunological detection of minimal residual disease in children with acute lymphoblastic leukaemia. Lancet 1998; 351: 550–554.
van der Velden VH, de Bie M, van Wering ER, van Dongen JJ . Immunoglobulin light chain gene rearrangements in precursor-B-acute lymphoblastic leukemia: characteristics and applicability for the detection of minimal residual disease. Haematologica 2006; 91: 679–682.
Bruggemann M, van der Velden VH, Raff T, Droese J, Ritgen M, Pott C et al. Rearranged T-cell receptor beta genes represent powerful targets for quantification of minimal residual disease in childhood and adult T-cell acute lymphoblastic leukemia. Leukemia 2004; 18: 709–719.
van der Velden VH, Szczepanski T, Wijkhuijs JM, Hart PG, Hoogeveen PG, Hop WC et al. Age-related patterns of immunoglobulin and T-cell receptor gene rearrangements in precursor-B-ALL: implications for detection of minimal residual disease. Leukemia 2003; 17: 1834–1844.
van der Velden VH, Bruggemann M, Hoogeveen PG, de Bie M, Hart PG, Raff T et al. TCRB gene rearrangements in childhood and adult precursor-B-ALL: frequency, applicability as MRD-PCR target, and stability between diagnosis and relapse. Leukemia 2004; 18: 1971–1980.
Szczepanski T, Beishuizen A, Pongers-Willemse MJ, Hahlen K, van Wering ER, Wijkhuijs AJ et al. Cross-lineage T cell receptor gene rearrangements occur in more than ninety percent of childhood precursor-B acute lymphoblastic leukemias: alternative PCR targets for detection of minimal residual disease. Leukemia 1999; 13: 196–205.
Beishuizen A, de Bruijn MA, Pongers-Willemse MJ, Verhoeven MA, van Wering ER, Hahlen K et al. Heterogeneity in junctional regions of immunoglobulin kappa deleting element rearrangements in B cell leukemias: a new molecular target for detection of minimal residual disease. Leukemia 1997; 11: 2200–2207.
Bruggemann M, Droese J, Bolz I, Luth P, Pott C, von Neuhoff N et al. Improved assessment of minimal residual disease in B cell malignancies using fluorogenic consensus probes for real-time quantitative PCR. Leukemia 2000; 14: 1419–1425.
van der Velden VH, Willemse MJ, van der Schoot CE, Hahlen K, van Wering ER, van Dongen JJ . Immunoglobulin kappa deleting element rearrangements in precursor-B acute lymphoblastic leukemia are stable targets for detection of minimal residual disease by real-time quantitative PCR. Leukemia 2002; 16: 928–936.
van der Velden VH, Wijkhuijs JM, Jacobs DC, van Wering ER, van Dongen JJ . T cell receptor gamma gene rearrangements as targets for detection of minimal residual disease in acute lymphoblastic leukemia by real-time quantitative PCR analysis. Leukemia 2002; 16: 1372–1380.
Szczepanski T, Langerak AW, Willemse MJ, Wolvers-Tettero IL, van Wering ER, van Dongen JJ . T cell receptor gamma (TCRG) gene rearrangements in T cell acute lymphoblastic leukemia reflect ‘end-stage’ recombinations: implications for minimal residual disease monitoring. Leukemia 2000; 14: 1208–1214.
Breit TM, Wolvers-Tettero IL, Beishuizen A, Verhoeven MA, van Wering ER, van Dongen JJ . Southern blot patterns, frequencies, and junctional diversity of T-cell receptor-delta gene rearrangements in acute lymphoblastic leukemia. Blood 1993; 82: 3063–3074.
van Dongen JJ, Wolvers-Tettero IL . Analysis of immunoglobulin and T cell receptor genes. Part II: possibilities and limitations in the diagnosis and management of lymphoproliferative diseases and related disorders. Clin Chim Acta 1991; 198: 93–174.
Breit TM, Mol EJ, Wolvers-Tettero IL, Ludwig WD, van Wering ER, van Dongen JJ . Site-specific deletions involving the tal-1 and sil genes are restricted to cells of the T cell receptor alpha/beta lineage: T cell receptor delta gene deletion mechanism affects multiple genes. J Exp Med 1993; 177: 965–977.
Campana D, Coustan-Smith E . Minimal residual disease studies by flow cytometry in acute leukemia. Acta Haematol 2004; 112: 8–15.
Schrauder A, Reiter A, Gadner H, Niethammer D, Klingebiel T, Kremens B et al. Superiority of allogeneic hematopoietic stem-cell transplantation compared with chemotherapy alone in high-risk childhood T-cell acute lymphoblastic leukemia: results from ALL-BFM 90 and 95. J Clin Oncol 2006; 24: 5742–5749.
Stanulla M, Schaeffeler E, Flohr T, Cario G, Schrauder A, Zimmermann M et al. Thiopurine methyltransferase (TPMT) genotype and early treatment response to mercaptopurine in childhood acute lymphoblastic leukemia. JAMA 2005; 293: 1485–1489.
Acknowledgements
We thank Nicola Passow, Kirsten Linsmeier, Cornelia Rütz, Carmen Scherer, Heike Kuzan, Ivonne Schmitt, Daniela Mueller, Claudia Holzschuh, Yvonne Yeboah, and Anne Camminady (Heidelberg, Germany); Nicole Wittner and Annette Müller-Brechlin (Hannover, Germany); Lilia Corral, Elisabetta d'Aniello, Monica Manenti, Eugenia Mella, Antonella Musarò, Simona Songia, Tiziana Villa, and Giuseppe Gaipa (Monza, Italy); Giuseppe Germano, Laura Del Giudice, Emanuela Giarin, Monica Spinelli, and Marinella Veltroni (Padua, Italy); Marianne Konrad, Eva Csinadi, and Ulrike Monschein (Vienna, Austria); Rahel Schaub, Marco Thali, and Silvia van Essen (Zurich, Switzerland) for their excellent technical assistance and Anja Mörike and Gunnar Cario for their great help in preparing figures and tables and for critically reviewing the paper. We gratefully acknowledge the clinicians of the participating hospitals for their excellent cooperation and compliance and for sending bone marrow samples to the national study centers. We also thank the participants of the International BFM Study Group and all the centers of the Associazione Italiana Ematologia e Oncologia Pediatrica (AIEOP) for their close collaboration. The collaborative study was supported by the Deutsche Krebshilfe (Germany), the St Anna Kinderkrebsforschung, a grant from the FWF (P-13575-MED) to RP-G (Austria), the Associazione Italiana Ricerca Cancro (AIRC), Comitato ML Verga, Fondazione M Tettamanti (Monza, Italy), Fondazione Cariplo (Milano, Italy), Fondazione Città della Speranza (Padua, Italy), OncoSuisse (grant no. OCS01230-02-2002), Swiss Cancer League (grant no. SKL-01230-02-2002), and Swiss Research Foundation Child and Cancer (Switzerland). RS acknowledges support of NHMRC and TCCN Australia. The external quality control rounds were organized by the European Study Group on MRD detection in ALL (ESG-MRD-ALL; coordinated by JJM van Dongen and VHJ van der Velden), which was supported by Leukaemia Research Fund (LRF) and the European LeukemiaNet (ELN). From 2000 to 2006, the laboratory meetings of the MRD Task Force, which established the quality rounds, were supported by the German ‘Kind-Philipp-Foundation for Leukemia Research’.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Flohr, T., Schrauder, A., Cazzaniga, G. et al. Minimal residual disease-directed risk stratification using real-time quantitative PCR analysis of immunoglobulin and T-cell receptor gene rearrangements in the international multicenter trial AIEOP-BFM ALL 2000 for childhood acute lymphoblastic leukemia. Leukemia 22, 771–782 (2008). https://doi.org/10.1038/leu.2008.5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2008.5
Keywords
This article is cited by
-
Minimal residual disease detection by next-generation sequencing of different immunoglobulin gene rearrangements in pediatric B-ALL
Nature Communications (2023)
-
Prospective use of molecular minimal residual disease for risk stratification in children and adolescents with acute lymphoblastic leukemia
Wiener klinische Wochenschrift (2023)
-
Utility of Measurable Residual Disease (MRD) Assessment in Mantle Cell Lymphoma
Current Treatment Options in Oncology (2023)
-
Minimal residual disease detection by mutation-specific droplet digital PCR for leukemia/lymphoma
International Journal of Hematology (2023)
-
One-point flow cytometric MRD measurement to identify children with excellent outcome after intermediate-risk BCP-ALL: results of the ALL-MB 2008 study
Journal of Cancer Research and Clinical Oncology (2023)