Abstract
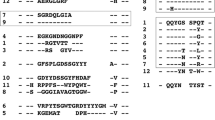
The chronic lymphocytic leukemia (CLL) immunoglobulin repertoire is uniquely characterized by the presence of stereotyped B-cell receptors (BCRs). A major BCR stereotype in CLL is shared by immunoglobulin G-switched cases utilizing the immunoglobulin heavy-chain variable 4-34 (IGHV4-34) gene. Increased titers of IGHV4-34 antibodies are detected in selective clinical conditions, including infection by B-cell lymphotropic viruses, particularly Epstein–Barr virus (EBV) and cytomegalovirus (CMV). In this context, we sought evidence for persistent activation by EBV and CMV in CLL cases expressing the IGHV4-34 gene. The study group included 93 CLL cases with an intentional bias for the IGHV4-34 gene. On the basis of real-time PCR results for CMV/EBV DNA, cases were assigned to three groups: (1) double-negative (59/93); (2) single-positive (CMV- or EBV-positive; 25/93); (3) double-positive (9/93). The double-negative group was characterized by heterogeneous IGHV gene repertoire. In contrast, a bias for the IGHV4-34 gene was observed in the single-positive group (9/25 cases; 36%). Remarkably, all nine double-positive cases utilized the IGHV4-34 gene; seven of nine cases expressed the major BCR stereotype as described above. In conclusion, our findings indicate that the interactions of CLL progenitor cells expressing distinctive IGHV4-34 BCRs with viral antigens/superantigens might facilitate clonal expansion and, eventually, leukemic transformation. The exact type, timing and location of these interactions remain to be determined.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Bhat NM, Bieber MM, Chapman CJ, Stevenson FK, Teng NN . Human antilipid A monoclonal antibodies bind to human B cells and the i antigen on cord red blood cells. J Immunol 1993; 151: 5011–5021.
Spellerberg MB, Chapman CJ, Mockridge CI, Isenberg DA, Stevenson FK . Dual recognition of lipid A and DNA by human antibodies encoded by the VH4-21 gene: a possible link between infection and lupus. Hum Antibodies Hybridomas 1995; 6: 52–56.
Li Y-C, Spellerberg MB, Stevenson FK, Capra JD, Potter KN . The I binding specificity of human IGHV4-34 (VH4.21) encoded antibodies is determined by both VH framework region 1 and complementarity determining region 3. J Mol Biol 1996; 256: 577–589.
Thomas MD, Clough K, Melamed MD, Stevenson FK, Chapman CJ, Spellerberg MB et al. A human monoclonal antibody encoded by the V4-34 gene segment recognises melanoma-associated ganglioside via CDR3 and FWR1. Hum Antibodies 1999; 9: 95–106.
Potter KN, Hobby P, Klijn S, Stevenson FK, Sutton BJ . Evidence for involvement of a hydrophobic patch in framework region 1 of human V4-34-encoded Igs in recognition of the red blood cell I antigen. J Immunol 2002; 169: 3777–3782.
Silberstein LE, George A, Durdik JM, Kipps TJ . The V4-34 encoded anti-i autoantibodies recognize a large subset of human and mouse B-cells. Blood Cells Mol Dis 1996; 22: 126–138.
Pugh-Bernard AE, Silverman GJ, Cappione AJ, Villano ME, Ryan DH, Insel RA et al. Regulation of inherently autoreactive VH4-34 B cells in the maintenance of human B cell tolerance. J Clin Invest 2001; 108: 1061–1070.
van Vollenhoven RF, Bieber MM, Powell MJ, Gupta PK, Bhat NM, Richards KL et al. VH4-34 encoded antibodies in systemic lupus erythematosus: a specific diagnostic marker that correlates with clinical disease characteristics. J Rheumatol 1999; 26: 1727–1733.
Cappione AJ, Pugh-Bernard AE, Anolik JH, Sanz I . Lupus IgG VH4.34 antibodies bind to a 220-kDa glycoform of CD45/B220 on the surface of human B lymphocytes. J Immunol 2004; 172: 4298–4307.
Mockridge CI, Rahman A, Buchan S, Hamblin T, Isenberg DA, Stevenson FK et al. Common patterns of B cell perturbation and expanded V4-34 immunoglobulin gene usage in autoimmunity and infection. Autoimmunity 2004; 37: 9–15.
Bhat NM, Bieber MM, Yang YC, Leu YS, van Vollenhoven RF, Teng NN . B cell lymphoproliferative disorders and IGHV4-34 gene encoded antibodies. Hum Antibodies 2004; 13: 63–68.
Loomes LM, Uemura K, Childs RA, Paulson JC, Rogers GN, Scudder PR et al. Erythrocyte receptors for Mycoplasma pneumoniae are sialylated oligosaccharides of Ii antigen type. Nature 1984; 307: 560–563.
Chapman C, Spellerberg M, Hamblin T, Stevenson F . Pattern of usage of the VH4-21 gene by B lymphocytesin a patient with EBV infection indicates ongoing mutation and class switching. Ann N Y Acad Sci 1995; 764: 195–197.
Fais F, Ghiotto F, Hashimoto S, Sellars B, Valetto A, Allen SL et al. Chronic lymphocytic leukemia B cells express restricted sets of mutated and unmutated antigen receptors. J Clin Invest 1998; 102: 1515–1525.
Ghia P, Stamatopoulos K, Belessi C, Moreno C, Stella S, Guida S et al. Geographic patterns and pathogenetic implications of IGHV gene usage in chronic lymphocytic leukemia: the lesson of the IGHV3-21 gene. Blood 2005; 105: 1678–1685.
Widhopf II GF, Kipps TJ . Normal B cells express 51p1-encoded Ig heavy chains that are distinct from those expressed by chronic lymphocytic leukemia B cells. J Immunol 2001; 166: 95–102.
Tobin G, Thunberg U, Johnson A, Eriksson I, Söderberg O, Karlsson K et al. Chronic lymphocytic leukemias utilizing the VH3-21 gene display highly restricted Vlambda2-14 gene use and homologous CDR3s: implicating recognition of a common antigen epitope. Blood 2003; 15: 4952–4957.
Ghiotto F, Fais F, Valetto A, Albesiano E, Hashimoto S, Dono M et al. Remarkably similar antigen receptors among a subset of patients with chronic lymphocytic leukemia. J Clin Invest 2004; 113: 1008–1016.
Widhopf II GF, Rassenti LZ, Toy TL, Gribben JG, Wierda WG, Kipps TJ . Chronic lymphocytic leukemia B cells of more than 1% of patients express virtually identical immunoglobulins. Blood 2004; 104: 2499–2504.
Messmer BT, Albesiano E, Efremov DG, Ghiotto F, Allen SL, Kolitz J et al. Multiple distinct sets of stereotyped antigen receptors indicate a role for antigen in promoting chronic lymphocytic leukemia. J Exp Med 2004; 200: 519–525.
Tobin G, Thunberg U, Karlsson K, Murray F, Laurell A, Willander K et al. Subsets with restricted immunoglobulin gene rearrangement features indicate a role for antigen selection in the development of chronic lymphocytic leukemia. Blood 2004; 104: 2879–2885.
Stamatopoulos K, Belessi C, Moreno C, Boudjograh M, Guida G, Smilevska T et al. Over 20% of patients with chronic lymphocytic leukemia carry stereotyped receptors: pathogenetic implications and clinical correlations. Blood 2007; 109: 259–270.
Thorselius M, Krober A, Murray F, Thunberg U, Tobin G, Bühler A et al. Strikingly homologous immunoglobulin gene rearrangements and poor outcome in VH3-21-utilizing chronic lymphocytic leukemia independent of geographical origin and mutational status. Blood 2006; 107: 2889–2894.
Murray F, Darzentas N, Hadzidimitriou A, Tobin G, Boudjogra M, Scielzo C et al. Stereotyped patterns of somatic hypermutation in subsets of patients with chronic lymphocytic leukemia: implications for the role of antigen selection in leukemogenesis. Blood 2008; 111: 1524–1533.
Landgren O, Gridley G, Check D, Caporaso NE, Morris Brown L . Acquired immune-related and inflammatory conditions and subsequent chronic lymphocytic leukaemia. Br J Haematol 2007; 139: 791–798.
Landgren O, Rapkin JS, Caporaso NE, Mellemkjaer L, Gridley G, Goldin LR et al. Respiratory tract infections and subsequent risk of chronic lymphocytic leukemia. Blood 2007; 109: 2198–2201.
Hatzi K, Catera R, Ferrarini M, Fischetti V, Herve M, Meffre E et al. B-cell chronic lymphocytic leukemia (B-CLL) cells express antibodies reactive with antigenic epitopes expressed on the surface of common bacteria. Blood 2006; 108: 25.
Lanemo Myhrinder A, Hellqvist E, Sidorova E, Söderberg A, Baxendale H, Dahle C et al. A new perspective: molecular motifs on oxidized-LDL, apoptotic cells, and bacteria are targets for chronic lymphocytic leukemia antibodies. Blood 2008; 111: 3838–3848.
Hallek M, Cheson B, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood 2008; 111: 5446–5456.
Lefranc MP, Giudicelli V, Kaas Q, Duprat E, Chastellan P, Coelho I et al. IMGT, the international ImMunoGeneTics information system. Nucleic Acids Res 2005; 33: D593–D597.
Giudicelli V, Chaume D, Lefranc MP . IMGT/V-QUEST, an integrated software program for immunoglobulin and T cell receptor V-J and V-D-J rearrangement analysis. Nucleic Acids Res 2004; 32: W435–W440.
Ghia P, Stamatopoulos K, Belessi C, Moreno C, Stilgenbauer S, Stevenson F et al. European Research Initiative on CLL. ERIC recommendations on IGHV gene mutational status analysis in chronic lymphocytic leukemia. Leukemia 2007; 21: 1–3.
Espy MJ, Uhl JR, Sloan LM, Buckwalter SP, Jones MF, Vetter EA et al. Real-time PCR in clinical microbiology: applications for routine laboratory testing. Clin Microbiol Rev 2006; 19: 165–256.
Hudnall SD, Chen T, Allison P, Tyring SK, Heath A . Herpesvirus prevalence and viral load in healthy blood donors by quantitative real-time polymerase chain reaction. Transfusion 2008; 48: 1180–1187.
Ghia P, Guida G, Stella S, Gottardi D, Geuna M, Strola G et al. The pattern of CD38 expression defines a distinct subset of chronic lymphocytic leukemia (CLL) patients at risk of disease progression. Blood 2003; 101: 1262–1269.
Athanasiadou A, Stamatopoulos K, Gaitatzi M, Stavroyianni N, Fassas A, Anagnostopoulos A . Recurrent cytogenetic findings in subsets of patients with chronic lymphocytic leukemia expressing IgG-switched stereotyped immunoglobulins. Haematologica 2008; 93: 473–474.
Pascual V, Victor K, Spellerberg M, Hamblin TJ, Stevenson FK, Capra JD . VH restriction among human cold agglutinins: the VH4-21 gene segment is required to encode anti-I and anti-i specificities. J Immunol 1992; 149: 2337–2344.
McClain T, Harley JB, James JA . The role of Epstein–Barr virus in systemic lupus erythematosus. Front Biosci 2001; 6: 137–147.
Poole BD, Scofield RH, Harley JB, James JA . Epstein–Barr virus and molecular mimicry in systemic lupus erythematosus. Autoimmunity 2006; 39: 63–70.
Bhat NM, Bieber MM, Spellerberg MB, Stevenson FK, Teng NN . Recognition of auto- and exoantigens by V4-34 gene encoded antibodies. Scand J Immunol 2000; 51: 134–140.
Milner EC, Anolik J, Cappione A, Sanz I . Human innate B cells: a link between host defense and autoimmunity? Springer Semin Immunopathol 2005; 26: 433–452.
Chaganti S, Ma CS, Bell AI, Croom-Carter D, Hislop AD, Tangye SG et al. Epstein–Barr virus persistence in the absence of conventional memory B cells: IgM+IgD+CD27+ B cells harbor the virus in X-linked lymphoproliferative disease patients. Blood 2008; 112: 672–679.
Krishnan MR, Jou NT, Marion TN . Correlation between the amino acid position of arginine in VH-CDR3 and specificity for native DNA among autoimmune antibodies. J Immunol 1996; 157: 2430–2439.
Jang YJ, Stollar BD . Anti-DNA antibodies: aspects of structure and pathogenicity. Cell Mol Life Sci 2003; 60: 309–320.
Li Y, Li H, Ni D, Weigert M . Anti-DNA B cells in MRL/lpr mice show altered differentiation and editing pattern. J Exp Med 2002; 196: 1543–1552.
Li H, Jiang Y, Prak EL, Radic M, Weigert M . Editors and editing of anti-DNA receptors. Immunity 2001; 15: 947–957.
Olsen LR, Dessen A, Gupta D, Sabesan S, Sacchettini JC, Brewer CF . X-ray crystallographic studies of unique cross-linked lattices between four isomeric biantennary oligosaccharides and soybean agglutinin. Biochemistry 1997; 36: 15073–15080.
Rahman A, Isenberg DA . Systemic lupus erythematosus. N Engl J Med 2008; 358: 929–939.
Khan N, Shariff N, Cobbold M, Bruton R, Ainsworth JA, Sinclair AJ et al. Cytomegalovirus seropositivity drives the CD8 T cell repertoire toward greater clonality in healthy elderly individuals. J Immunol 2002; 169: 1984–1992.
Nascimbeni M, Shin EC, Chiriboga L, Kleiner DE, Rehermann B . Peripheral CD4(+)CD8(+) T cells are differentiated effector memory cells with antiviral functions. Blood 2004; 104: 478–486.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kostareli, E., Hadzidimitriou, A., Stavroyianni, N. et al. Molecular evidence for EBV and CMV persistence in a subset of patients with chronic lymphocytic leukemia expressing stereotyped IGHV4-34 B-cell receptors. Leukemia 23, 919–924 (2009). https://doi.org/10.1038/leu.2008.379
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2008.379
Keywords
This article is cited by
-
Genome-wide association study identifies risk loci for progressive chronic lymphocytic leukemia
Nature Communications (2021)
-
Aberrant Epstein-Barr virus antibody patterns and chronic lymphocytic leukemia in a Spanish multicentric case-control study
Infectious Agents and Cancer (2015)
-
New insights into the pathobiology of chronic lymphocytic leukemia
Journal of Hematopathology (2011)
-
A different ontogenesis for chronic lymphocytic leukemia cases carrying stereotyped antigen receptors: molecular and computational evidence
Leukemia (2010)
-
Intraclonal diversification of immunoglobulin light chains in a subset of chronic lymphocytic leukemia alludes to antigen-driven clonal evolution
Leukemia (2010)