Abstract
The posterior nasal nerve is the dominant source of the parasympathetic, sympathetic, and sensory fibers that innervate the nasal respiratory mucosa. Therefore, a posterior nasal neurectomy (PNN) is thought to induce denervation of the nasal mucosa and relieve the nasal symptoms of allergic rhinitis. However, the underlying mechanisms and therapeutic action of PNN remain unknown. To investigate the impact of PNN-induced denervation of the nasal mucosa on allergic rhinitis, we developed a rat model of PNN and examined the effects of PNN on allergic rhinitis in ovalbumin-sensitized rats. This rat model of PNN was characterized by the depletion of nerve fibers, choline acetyltransferase, and neuropeptides (eg, substance P, calcitonin gene-related peptide, vasoactive intestinal peptide, and neuropeptide Y) in the nasal respiratory mucosa. These animals exhibited nasal gland and goblet cell hypertrophy in the septal mucosa and atrophy of the submucosal gland in the lateral nasal wall, as well as reduced nasal secretion due to deficient acetylcholine synthesis. In an ovalbumin-sensitized model of allergic rhinitis, PNN also induced the depletion of nerve fibers, choline acetyltransferase, and neuropeptides in the nasal mucosa and suppressed nasal secretion. However, PNN did not affect mucosal thickening, eosinophil and mast cell infiltration, interleukin-4 and interferon-γ mRNA expression, and allergic symptoms (ie, sneezing and nasal scratching). These results suggest that the peripheral nerves and corresponding neuropeptides regulate nasal secretion, but not hypersensitivity, in allergic rhinitis, and that allergic rhinitis-related mucosal reactions occur in a highly denervated mucosa after PNN. Posterior nasal neurectomy may be a therapeutic option for the treatment of hyperrhinorrhea, but not allergic rhinitis hypersensitivity.
Similar content being viewed by others
Main
Allergic rhinitis is among the most common diseases; affecting 10–30% of people in industrialized countries.1, 2, 3 This condition presents with symptoms that reduce the quality of life such as rhinorrhea, sneezing, nasal obstruction, and nasal itching.4 Medical allergic rhinitis treatment is approached in a stepwise manner and includes agents such as antihistamines and nasal topical steroids.1, 2, 5 However, for patients with allergic rhinitis refractory to medication therapy; surgical interventions such as endoscopic posterior nasal neurectomy (PNN) have been attempted.
Endoscopic PNN, which involves the intranasal severing of the posterior nasal nerve, is a common surgical treatment for allergic rhinitis in Asia.2, 6, 7 The posterior nasal nerve, which is a peripheral branch of the vidian nerve, innervates the nasal cavity via the pterygopalatine ganglion, which comprises parasympathetic and sympathetic vidian nerve fibers and sensory nerve fibers from the trigeminal nerve. Therefore, PNN is expected to suppress nasal hypersecretion by blocking autonomic vidian nerve fibers, similar to vidian neurectomy (VN), as well as hypersensitivity by simultaneously blocking sensory nerve fibers.6, 7, 8, 9, 10 However, the effects of PNN on the suppression of sensitivity in the nasal mucosa remain controversial.11 Some previous reports have described the beneficial effects of PNN on rhinorrhea and sneezing,6, 7, 8, 9, 10 although other reports have failed to observe an effect of PNN on sneezing.11, 12 The histological changes underlying the effects of PNN have not been elucidated because of the limitations of human studies and the lack of animal models.
In the present study, we developed an animal model of PNN and examined the effect of PNN on the nasal mucosal structure and function. We also investigated the therapeutic effects of PNN on experimental allergic rhinitis to elucidate the effect of nasal mucosal denervation on allergic reactions. On the basis of previous human clinical studies, we hypothesized that PNN-induced nasal mucosal denervation would contribute to the suppression of allergic rhinitis reactions.
MATERIALS AND METHODS
Animals
Male Sprague–Dawley rats (8 weeks old; approximate weight, 200 g) were purchased from CLEA Japan (Tokyo, Japan). The rats were housed in a light-controlled room with a 12-h light/dark cycle and were allowed food and water ad libitum. All procedures were approved by the University of Tokyo Animal Care Committee (Tokyo, Japan) and conducted in accordance with the University of Tokyo guidelines for the handling and care of laboratory animals.
Rat Model of PNN
The effect of PNN was investigated in rats by cutting the left posterior nasal nerves at the pterygopalatine foramen (PNN side). The right posterior nasal nerve remained intact, unless otherwise specified. Rats not subjected to any surgical procedures were included as the controls.
The surgical approach to the pterygopalatine ganglion was conducted as previously described by Spencer et al.13 A longitudinal 1.5-cm incision was formed along the supraorbital ridge (Figure 1a1), and the skin and underlying tissue were scraped from the frontal bone. The periorbita was freed from the zygomatic arch, and the orbital content was retracted laterally. The nasociliary branch of the ophthalmic nerve and accompanying ethmoidal blood vessels entering the anterior ethmoidal foramen were identified in the shallow area and cut with a cautery (Figures 1a2 and a3). Under continued retraction, adherent periorbital tissue was freed from the frontal bone via blunt dissection until the maxillary nerve was visible in the pterygopalatine fossa (Figures 1a4 and a5). The pterygopalatine ganglion was ventromedial to the maxillary nerve, and its rostral end was identified along with the orbital vidian nerve branch running rostrally and the posterior nasal vidian nerve branch running medially to enter the pterygopalatine foramen (Figures 1a6 and a7). The posterior nasal nerve was cut with a cautery at the entrance of the pterygopalatine foramen. We cut the posterior nasal nerve as distally as possible at a minimum ablation output level to prevent thermal damage to the pterygopalatine ganglion. However, it is possible that damage did occur. An additional group of rats underwent selective neurectomy of the ophthalmic nasociliary branch alone to differentiate the effect of nasociliary neurectomy from that of PNN on the nasal mucosa.
(a1–a7) The posterior nasal neurectomy (PNN) method and experimental protocol. (a6) Diagram of our surgical approach to the posterior nasal nerve. This is a magnified view of the circle in (a4). The dotted double-headed arrow indicates the PNN location. (a7) The magnified view of the pterygopalatine fossa. The white arrow indicates the posterior nasal nerve; the white arrowheads indicate the pterygopalatine ganglion (PPG). (b) The protocol for ovalbumin (OVA) sensitization and PNN.
The effect of posterior nasal neurectomy (PNN) on the nasal mucosa after 2 weeks. (a) Photomicrographs of representative coronal nasal cavity sections. (a ′) The magnified view of the areas indicated by the square in (a). (b–g, b′–g′) Hematoxylin and eosin (H&E) and protein gene product 9.5 (PGP 9.5), substance P (SP), calcitonin gene-related peptide (CGRP), vasoactive intestinal peptide (VIP), and neuropeptide Y (NPY) immunofluorescence analyses of the nasal respiratory mucosa from the PNN-treated sides (b–g) and untreated sides (b′–g′). Septal mucosal areas indicated by the squares in (a) are shown. (h–h′′′) Triple PGP 9.5 (h; red), choline acetyltransferase (ChAT) (h′; green) and 4′,6-diamidino-2-phenylindole (DAPI) (h′′; blue) immunofluorescence analysis. (i, i′) muscarinic acetylcholine receptor M3 (M3) immunofluorescence analyses of the nasal respiratory mucosa from the PNN-treated side (i) and untreated side (i′). (j, j′) PGP 9.5 immunofluorescence analysis at the anterior end of the nasal cavity. (k, k′) PGP 9.5 immunofluorescence analysis of the olfactory epithelium. (l, l′) PGP 9.5 immunofluorescence analysis of the nasal respiratory mucosa after selective nasociliary branch neurectomy of the ophthalmic nerve. The white arrowheads indicate the nerves that were PGP 9.5-positive (c and c′, h and h′′′, j and j′, k and k′, and l and l′), SP-positive (d, d′), CGRP-positive (e, e′), VIP-positive (f, f′), NPY-positive (g, g′), and ChAT-positive (h′) nerves. Scale bar, 100 μm.
Two weeks after unilateral PNN, nasal tissues were harvested for histological analyses (n=4 per group). Fresh nasal mucosa was also harvested separately from the PNN-treated and untreated sides (n=4/group) for quantitative real-time PCR (qPCR).
Protocol of Ovalbumin Sensitization and PNN in Ovalbumin-Sensitized Rats
A rat model of allergic rhinitis was used to investigate the effect of PNN on allergic rhinitis (Figure 1b). In brief, chicken egg white albumin (ovalbumin (OVA); Sigma-Aldrich, St. Louis, MO, USA) was diluted to 1000 μg/body in sterile normal saline with 20-mg/body aluminum hydroxide gel (Imject Alum; Pierce, Rockford, IL, USA), and administered three times via intraperitoneal injection on days 1, 8, and 15. On day 21, bilateral PNN was performed, followed by a daily intranasal challenge with OVA diluted in sterile normal saline (300 μg OVA/15 μl per nostril) on days 22–35. The control animals received phosphate-buffered saline (PBS) instead of OVA.
The animals were subdivided into three groups (n=4 per group): (1) PBS-treated PNN-untreated rats (PBS group), (2) OVA-sensitized PNN-untreated rats (OVA group), and (3) OVA-sensitized PNN-treated rats (OVA+PNN group). After the final intranasal OVA challenge on day 36, the allergic rhinitis phenotype was confirmed using a symptom score calculated from the total number of sneezing and nasal scratching during a 20-min period. On day 37 (24 h after the final antigen challenge), nasal tissues were harvested for histology and real-time qPCR.
Tissue Preparation and Immunohistochemistry
Rats were deeply anesthetized, subjected to perfusion fixation with saline and 10% neutral buffered formalin, and decapitated. Nasal cavities were locally irrigated with the same fixative. Trimmed heads were skinned and further fixed by immersion in the same fixative for 2 days, followed by decalcification in 10% ethylenediamine tetraacetic acid for 4 weeks. After decalcification, specimens were embedded in paraffin or OTC medium (Tissue-Tek OTC Compound; Sakura Finetek, Torrance, CA, USA). Serial coronal sections (4-μm thick for paraffin sections and 15-μm thick for frozen sections) were cut and mounted on MAS-coated slides (Matsunami Glass, Osaka, Japan).
Paraffin sections were deparaffinized, rehydrated, immersed in antigen retrieval solution (Target Retrieval Solution; Dako, Tokyo, Japan), and autoclaved at 121 °C for 20 min for antigen retrieval. Frozen sections were washed in PBS. All sections were incubated with blocking solution (Protein Block, Serum-Free; Dako) to reduce nonspecific antibody binding. For immunoperoxidase staining, sections were pretreated with 100% methanol containing 3% hydrogen peroxide to suppress endogenous peroxidase activity.
Paraffin sections were incubated with the following primary antibodies: rabbit anti-protein gene product 9.5 (PGP 9.5; Z5116, 1:1000 dilution; Dako), goat anti-choline acetyltransferase (ChAT; AB144p, 1:100; Millipore, Tokyo, Japan), mouse anti-major basic protein (MBP; CBL419, 1:50; Millipore), and mouse anti-mast cell tryptase (MCT; ab2378, 1:1000; Abcam, Tokyo, Japan). Sections for MBP immunostaining were incubated in 0.5 mg/ml proteinase (type XXIV; Sigma-Aldrich, Tokyo, Japan) in Tris-HCl (pH 7.6) at room temperature for 3 min for antigen retrieval. The numbers of MBP-positive eosinophils and MCT-positive mast cells in the lamina propria were counted microscopically in three different high-powered microscopic fields of the septal cartilage nasal respiratory mucosa. The following rabbit-derived primary antibodies were used for frozen sections: anti-substance P (anti-SP; ab133240, 1:1000 dilution; Abcam), anti-calcitonin gene-related peptide (anti-CGRP; C8198, 1:4000; Sigma-Aldrich), anti-vasoactive intestinal peptide (anti-VIP; BP882, 1:1000; Acris, San Diego, CA, USA), anti-neuropeptide Y (anti-NPY; ab30914, 1:4000; Abcam), and anti-muscarinic acetylcholine receptor M3 (anti-M3; ab87199, 1:500; Abcam).
For immunofluorescence staining, primary-stained sections were incubated with appropriate Alexa Fluor-conjugated secondary antibodies and mounted in Vectashield mounting medium with DAPI (Vector Laboratories, Burlingame, CA, USA). For immunoperoxidase staining, primary-stained sections were incubated with appropriate peroxidase-conjugated secondary antibodies and diaminobenzidine substrate.
Histological and Morphometric Analysis
The histological analysis included the respiratory mucosa of the septum and the lateral nasal wall in coronal sections at the level of the incisive papilla of the hard palate.14 The former was primarily used for quantitative analyses to control interindividual variability in three-dimensional complexed structures of the lateral nasal wall. Serial sections were stained with hematoxylin and eosin to observe the mucosal morphology, with periodic acid–Schiff (PAS) to detect neutral mucins in the nasal glands, and with Alcian blue (pH=2.5) to label sulfated acid mucins in the goblet cells. The PNN-treated (ie, left) side and PNN-untreated (ie, right) side were compared using a digital microscope camera (Keyence BZ-9000; Figures 2a and a′). To visualize the extent of the mucosal area innervated by the posterior nasal nerve, the nasal tissues of additional PNN-treated rats were serially cut from the nostril through the choana, and 10 sections at equal intervals were histologically analyzed (n=2). To compare the amount of mucus in the respiratory epithelium, we selected three high-magnification microscopic fields along the respiratory mucosa of the nasal septum (ie, the upper, middle, and bottom parts of the nasal septum) and measured the cross-sectional areas of Alcian blue-positive mucus and goblet cells using image analysis software (Micro Analyzer Ver. 1.1; Nippon Poladigital, Tokyo, Japan). The area of Alcian blue-positive mucus per unit mucosa was calculated over the basal lamina.
Quantification of Nerve Fiber Density
The density of nerve fibers innervated in the mucosa was quantified using NIS Elements AR Software (Nikon, Melville, NY, USA). The image RGB threshold was set to detect PGP 9.5 immunostaining in the image. After a set threshold was applied, the area distribution of PGP 9.5-positive fibers per unit area of nasal epithelium was calculated in three different microscopic fields of the septal nasal mucosa. The relative ratio of PGP 9.5-positive fiber density to the control group was measured.
In Vivo Measurement of Nasal Secretion
The filter paper technique described by Petersson et al15 was used with modifications. Rats were anesthetized and placed supine while breathing spontaneously through a tracheal cannula. Strips of filter paper shaped to feature a narrower strip on one end (15 × 5 and 15 × 1 mm at the wide and narrow ends, respectively; No26-Wa, ADVANTEC, Tokyo, Japan) were weighed, and the narrow ends were subsequently inserted lengthwise throughout both nasal cavities for 10 min. After removal, the strips were reweighed, and changes in weight (ie, the weight of the nasal secretions) were calculated per nostril (n=4/group). Nasal secretions were collected and measured 2 weeks after unilateral PNN, and on day 36 of the OVA sensitization protocol.
Effect of a Cholinergic Reagent on Nasal Secretion
In the first experiment, the nonselective muscarinic acetylcholine agonist pilocarpine (0.1 mg/kg; Wako Pure Chemical Industries, Osaka, Japan) or reversible acetylcholinesterase inhibitor neostigmine bromide (0.1 mg/kg; Wako Pure Chemical Industries) was administered intraperitoneally to the rats 2 weeks after unilateral PNN. Nasal secretions were measured using the previously described filter paper technique after the administration of each reagent (n=4).
In the second experiment, pilocarpine (0.1 mg/kg) was administered intraperitoneally to the OVA-sensitized rats with/without PNN treatment and to the control rats (ie, OVA unsensitized; n=4).
The Effect of Histamine on Allergic Symptoms in OVA+PNN Rats
In the first experiment, histamine dihydrochloride (150 μg/15 μl per nostril; Wako Pure Chemical Industries) was administered intranasally to normal or bilateral PNN-treated rats. Chlorpheniramine maleate (1 mg/kg; Wako Pure Chemical Industries), a histamine receptor 1 blocker, was administered intraperitoneally 60 min before intranasal histamine provocation, based on a previously reported procedure with modifications.16 The control group received PBS instead of histamine. The animals were subdivided into four groups (n=4 for each group): (1) control group (PBS provocation, PNN untreated), (2) histamine provocation rat group (PNN untreated), (3) PNN-treated and histamine provocation rat group, and (4) PNN-treated and histamine provocation with chlorpheniramine maleate administration rat group. Symptom scores were calculated from the total number of nasal sneezing and scratching events during the 20-min period after the provocation.
In the second experiment, histamine dihydrochloride (150 μg/15 μl per nostril; Wako Pure Chemical Industries) or PBS was also administered intranasally to the following four groups with/without OVA sensitization, and the amount of nasal secretion was measured (n=4): (1) control rat group (ie, OVA unsensitized, PNN treated), (2) PNN rat group (ie, OVA unsensitized), (3) OVA rat group (ie, PNN untreated), and (4) PNN+OVA rat group. In the PNN and the PNN+OVA groups, histamine was intranasally administered on the left PNN-treated side, and nasal secretion was measured on the left side.
The Effect of Histamine on Contralateral Nasal Secretion
Histamine dihydrochloride (150 μg/15 μl per nostril; Wako Pure Chemical Industries) was administered intranasally on one side in the control rats (ie, no PNN), on the PNN side of the unilateral PNN-treated rats, and on the untreated side of unilateral PNN-treated rats. The contralateral nasal secretion was then measured using the aforementioned filter paper technique (n=4).
Quantitative Real-time PCR
Total RNA was isolated from the septal nasal mucosa using the Nucleo Spin RNA kit (Takara Biotechnology, Shiga, Japan), and first-strand cDNA was reverse transcribed using PrimeScript RT Master Mix (Takara Biotechnology), based on the manufacturer’s instructions. qPCR (SYBR Green Assay; Applied Biosystems, Foster City, CA, USA) was performed using SYBR Premix Ex Taq II (Takara Biotechnology) and an ABI prism 7500 Sequence Detector system (Thermo Fisher Scientific K.K., Kanagawa, Japan).
The following primer sequences were used: mucin 5ac (Muc5ac) forward: 5′-CTCCGTCTTAGTCAATAACCACC-3′, Muc5ac reverse: 5′-GGAACTCGTTGGATTTTGGACTG-3′; mucin 5b (Muc5b) forward: 5′- GGCCTCTGGCAAGAAGATGT-3′, Muc5b reverse: 5′- GTTCTCTGCCCGACACTCAA-3′; interleukin-4 (Il4) forward: 5′-CAGGGTGCTTCGCAAATTTT-3′, Il4 reverse: 5′- CTCAGTTCACCGAGAACCCC-3′; interferon gamma (Ifng) forward: 5′- TCTGGAGGAACTGGCAAAAG-3′, Ifng reverse: 5′- GTGCTGGATCTGTGGGTT;G-3′; and glyceraldehyde 3-phosphate dehydrogenase (Gapdh; housekeeping) forward: 5′-CCTCAAGATTGTCAGCAAT-3′, Gapdh reverse: 5′-CCATCCACAGTCTTCTGAGT-3′. The gene expression levels were calculated as the difference between the cycle threshold (Ct) value of the target gene and the Ct value of GAPDH (ΔCt) using the comparative threshold cycle (2−ΔΔCT) method (n=4 per group).
Statistical Analysis
All statistical analyses were performed with Statmate IV software (ATMS, Tokyo, Japan). Dual comparisons were made with the Student’s t-test. For multiple comparisons, parametrically distributed data were compared via an analysis of variance with post hoc Tukey’s tests. Nonparametrically distributed data were compared using Kruskal–Wallis tests with post hoc Dunn’s tests. The level of significance was set at P<0.05.
RESULTS
Effect of PNN on Innervation of the Nasal Respiratory Mucosa
To investigate the effect of PNN on the nasal mucosa, we developed a rat model of PNN by severing the posterior nasal nerve via a periorbital approach. A histological comparison of the untreated and PNN sides revealed no apparent effects of this surgery on the overall nasal epithelial morphology with respect to thickness (Figures 2a and a′) and cellular infiltration (Figures 2b and b′).
The effect of PNN on the distribution of sensory, sympathetic, and parasympathetic nerves over the nasal respiratory mucosa was investigated via immunostaining for neuronal markers. Immunoreactivity against the pan-neuronal marker PGP 9.5 (Figures 2c, c′ and h), sensory neuronal markers SP (Figures 2d and d′) and CGRP (Figures 2e and e′), parasympathetic marker VIP (Figure 2f and f′), sympathetic nerve marker NPY (Figures 2g and g′), and cholinergic nerve marker ChAT (Figures 2h′ and h′′′) mostly disappeared from the nasal mucosa of the PNN-treated side, compared with the untreated side. These data demonstrate that PNN successfully denervated sensory, sympathetic, and parasympathetic nerves in the nasal mucosa.
Immunoreactivity against the muscarinic receptor M3 was comparable on the PNN-treated and untreated sides (Figures 2i and i′), suggesting that PNN did not affect cholinergic receptor expression. An analysis of PGP 9.5 distribution throughout the nasal cavity revealed the absence of this marker in most areas of the PNN-treated nasal respiratory mucosa, although its expression remained in the anterior end of the nasal cavity (Figures 2j and j′). In the olfactory mucosa, broad epithelial PGP 9.5 distribution was visible on the PNN-treated and -untreated sides (Figures 2k and k′). Selective neurectomy of the ophthalmic nasociliary branch did not have any apparent effects on the distribution of PGP 9.5 immunoreactivity throughout the nasal mucosa (Figures 2l and l′). These data collectively confirmed that our PNN model induced denervation of sensory, sympathetic, and parasympathetic fibers throughout the nasal respiratory mucosa, except for the anterior end and olfactory mucosa of the nasal cavity.
Posterior Nasal Neurectomy Induced Nasal Gland and Goblet Cell Hypertrophy of the Nasal Septum and Atrophy of the Gland in the Lateral Nasal Wall
The effect of PNN on nasal secretions was first determined by examining the characteristics of the nasal glands and goblet cells. Posterior nasal neurectomy induced hypertrophic and metaplastic changes in the septal nasal glands (Figures 3a and b), whereas the submucosal glands in the lateral nasal wall on the PNN-treated side were mildly atrophied, compared with those on the untreated side (Figure 3c). PAS staining for neutral mucins was considerably more intense on the septal glands of the PNN-treated side (Figure 3d), whereas Alcian blue staining of sulfated acid mucins was negative on the glands (Figure 3e). There was a nearly continuous layer of Alcian blue-positive goblet cells along the septal respiratory mucosa on the PNN-treated side, but only a few diffusely positive goblet cells on the untreated side (Figure 3e). Quantitative morphometric analysis confirmed that the number of Alcian blue-positive cells in the nasal epithelium was significantly greater on the PNN-treated side (P<0.05; Figure 3f). qPCR revealed significantly higher Muc5ac mRNA expression in the nasal mucosa on the PNN-treated side than on the untreated side or in the controls (P<0.05; Figure 3g), whereas the Muc5b mRNA expression level was not different between these groups (data not shown). These results suggest that PNN promotes mucin production in the nasal septum through nasal gland hypertrophy and goblet cell hyperplasia in the denervated nasal mucosa, whereas PNN induces atrophy of the submucosal glands in the lateral nasal wall.
Histological changes in the nasal glands and goblet cells 2 weeks after the posterior nasal neurectomy (PNN). (a) Photomicrographs of representative coronal nasal cavity sections. (b, d, e) The magnified views of the septal mucosa indicated by the squares in (a). (c, c′) The magnified views of the nasal glands in the lateral nasal wall indicated by the squares in (a). The black arrows indicate the nasal glands in the lateral nasal wall. (a–c) Hematoxylin and eosin staining. (d) Periodic acid–Schiff staining. (e) Alcian blue staining. The magnified views of the areas indicated by the squares in the upper panels (b, d, e) are shown in the lower panels. Scale bar, 100 μm. (f) Quantitative analysis of Alcian blue-positive areas in the nasal epithelium. The data are shown as the mean±s.e.m. (n=4). * P<0.05 (unpaired two-tailed Student t-test). (g) Mucin 5ac (Muc5ac) mRNA expression in the nasal respiratory mucosa. The data are shown as the mean±s.e.m. (n=4). *P<0.05 (Dunn’s test).
The Effect of PNN on Nasal Secretion
Crust formation was always seen in the nasal vestibule of the PNN-treated side up to a few months after PNN (Figure 4a); therefore, the effect of PNN on nasal secretion was quantified using a modified filter paper technique.15 The secretion amounts in the control animals and the untreated sides of animals subjected to PNN were comparable. By contrast, the nasal secretion amounts on the PNN-treated side were less than one-half of the amount on the untreated side at 2 weeks after PNN (Figure 4b).
The effect of posterior nasal neurectomy (PNN) on nasal secretion. (a) Macroscopic photograph of the nasal vestibule of a rat 2 weeks after PNN. The black arrow indicates crust formation in the nasal vestibule on the PNN-treated side. (b) Changes in nasal secretion after PNN measured using the filter paper technique. Data are shown as the mean±s.e.m. (n=4). *P<0.05 and **P <0.01 (Tukey’s test). (c) Changes in nasal secretion after the administration of the cholinergic agonist pilocarpine. The control bar represents the amount of nasal secretion in a normal rat without pilocarpine administration. The data are shown as the mean±s.e.m. (n=4). *P<0.05 (Tukey’s test). (d) Changes in nasal secretion after the administration of the cholinesterase inhibitor neostigmine bromide. The control bar represents the amount of nasal secretion in a normal rat without neostigmine bromide administration. The data are shown as the mean±s.e.m. (n=4). **P<0.01 (Tukey’s test).
Because PNN did not affect the expression of M3 (Figures 2i and i′), which is known to stimulate airway secretion,17 we tested the effects of cholinergic agents on nasal secretion to investigate the mechanism by which PNN reduced nasal secretion. The intraperitoneal administration of the cholinergic agonist pilocarpine stimulated nasal secretion on the PNN-treated and the untreated sides (Figure 4c). By contrast, the intraperitoneal administration of the cholinesterase inhibitor neostigmine bromide stimulated nasal secretion only on the untreated side (Figure 4d). Together with the M3 and ChAT expression patterns after PNN, this finding suggests that PNN abrogates acetylcholine synthesis, leading to decreased nasal secretion, but does not affect acetylcholine receptor function and expression.
The Effect of PNN on Mucosal Histology in OVA-Sensitized Rats
To test our hypothesis that mucosa denervation by PNN contributes to the suppression of allergic rhinitis-related symptoms, we generated a rat model of allergic rhinitis through OVA sensitization and subjected these rats to bilateral PNN (ie, OVA+PNN group; Figure 1c). We first examined PNN-induced morphological changes in the nasal mucosa. The OVA-sensitized rats without PNN (ie, OVA group) exhibited mucosal thickening in the nasal epithelium and in the subepithelium (Figures 5a and a′) with strong eosinophil and mast cell infiltration in the lamina propria of the respiratory mucosa (Figures 5b and b′), compared with PBS-treated rats (ie, PBS group). In addition, the OVA group exhibited dense immunoreactivity for PGP 9.5 (Figure 5d′), SP, CGRP, VIP, and NPY in the mucosa. Quantitative analysis revealed that OVA sensitization increased PGP 9.5-positive nerve fiber density in the mucosa (Figure 5e). In the comparison between the OVA and OVA+PNN groups, PNN did not affect thickening of the nasal epithelium and subepithelium (Figure 5a′′) or eosinophil infiltration (Figures 5b′′ and f) and mast cell infiltration (Figures 5c′′ and g) into the nasal mucosa. On the other hand, PNN remarkably reduced PGP 9.5 (Figure 5d′′), SP, CGRP, VIP, NPY, and ChAT immunoreactivity, confirming that PNN induced denervation and neuropeptide loss in the OVA allergic rhinitis model. These results indicated that immune responses such as mucosal thickening and eosinophil or mast cell infiltration could occur even in denervated nasal mucosa without neuropeptides.
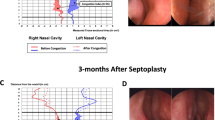
The effect of posterior nasal neurectomy (PNN) on allergic reactions in the nasal respiratory mucosa. (a–d) Nasal respiratory mucosal sections from phosphate-buffered saline (PBS)-treated, PNN-untreated rats (ie, the PBS group). (a′–d′), Sections from ovalbumin (OVA)-sensitized, PNN-untreated rats (ie, OVA group). (a′′–d′′) Sections from OVA-sensitized PNN-treated rats (ie, OVA+PNN group). The sections were stained with hematoxylin and eosin (a–a′′) or immunostained for major basic protein (MBP; b–b′′), mast cell tryptase (MCT; c–c′′), and PGP 9.5 (d–d′′). The black arrowheads indicate (b–b′′) MBP-positive or (c–c′′) MCT-positive cells. (d–d′′) The white arrowheads indicate PGP 9.5-positive nerves. Scale bar, 100 μm. (e) The relative ratio of PGP 9.5-positive nerves. *P<0.05 and **P<0.01 (Tukey’s test). (f, g) The number of (f) MBP-positive and (g) MCT-positive cells. The data are shown as the mean±s.e.m. (n=4). *P<0.05 and **P<0.01 (Dunn’s test). HPF, high-power field. (h) Changes in nasal secretion. The data are shown as the mean±s.e.m. (n=4). *P<0.05 (Tukey’s test). (i, j) Comparison of the symptom scores and the incidence of (i) sneezing and (j) scratching. The data are shown as the mean±s.e.m. (n=4). *P<0.05 and **P<0.01 (Tukey’s test). (k, l) Changes in (k) interleukin-4 (Il4) and (l) interferon gamma (Ifng) mRNA expression. The data are expressed as fold changes relative to housekeeping gene expression and are shown as the mean±s.e.m. (n=4). *P<0.05 (Dunn’s test).
The Effect of PNN on Allergic Symptoms and Cytokine Reactions in OVA-Sensitized Rats
We further examined the effects of PNN on nasal secretion, symptom scores, and inflammatory mediator mRNA expression patterns in our rat model of allergic rhinitis. The nasal secretion amount was nearly two-fold greater in OVA-sensitized without PNN rats than in PBS-treated rats or in the controls (ie, PBS provocation for OVA-sensitized rats; Figure 5h), whereas PNN decreased the elevated nasal secretion in OVA-sensitized rats to the control level. However, PNN did not affect the elevated symptom scores (eg, sneezing and scratching) in OVA-sensitized rats (Figures 5i and j). Furthermore, PNN did not alter the upregulated Il4 and downregulated Ifng expression observed in OVA-sensitized rats (Figures 5k and l). These results suggest that during allergic provocation, PNN reduces nasal secretion but does not affect mucosal sensitization-based allergic symptoms or cytokine expression in the mucosa.
Histamine and Cholinergic Agent for PNN and OVA Sensitization
We tested if PNN influences the histamine reactivity and subsequent neural reflex in the nasal mucosa. The control and PNN-treated rats exhibited similar frequencies of sneezing (Figure 6a) and scratching (Figure 6b) in response to histamine provocation. Intraperitoneal administration of the histamine receptor 1 blocker chlorpheniramine maleate partially suppressed sneezing and scratching in PNN-treated rats.
Histamine provocation and posterior nasal neurectomy (PNN). (a, b) Symptom scores were determined from the incidence of (a) sneezing and (b) scratching after histamine provocation and chlorpheniramine maleate administration. The data are shown as the mean±s.e.m. (n=4). *P<0.05 and **P<0.01 (Tukey’s test). (c) The amount of nasal secretion with contralateral nasal provocation of histamine. The data are shown as the mean±s.e.m. (n=4). *P<0.05 and **P<0.01 (Tukey’s test). (d) The amount of nasal secretion after histamine provocation. The data are shown as the mean±s.e.m. (n=4). *P<0.05 and **P<0.01 (Tukey’s test). (e) The amount of nasal secretion with a cholinergic agent. The data are shown as the mean±s.e.m. (n=4; Tukey’s test).
To further test if the residual secretory pathway and histamine hyperresponsiveness exist after PNN, we compared the amount of nasal secretion by histamine provocation among the following four groups with/without OVA sensitization: control rats (ie, OVA unsensitized, PNN untreated), PNN rats (ie, OVA unsensitized), OVA rats (ie, PNN untreated), and PNN+OVA rats. In all groups, the amount of nasal secretion after histamine provocation was greater than the amount after PBS provocation. There was no difference in the amount of secretion after histamine provocation between the control and OVA groups, or between the PNN and PNN+OVA groups. The results suggested that in our rat model, OVA sensitization did not induce histamine hyperresponsiveness, and histamine-induced nasal hypersecretion was not suppressed by PNN.
These two experiments suggested that a histamine-responsive neural reflex pathway remains even after PNN. To test this possibility, we performed histamine provocation on the PNN side in unilateral PNN-treated rats and measured the amount of contralateral nasal secretion. The nasal secretion was increased after contralateral histamine provocation in the unilateral PNN-treated rats and in the control rats (Figure 6c). By contrast, when histamine provocation was performed on the PNN-untreated side, the nasal secretion in the contralateral PNN side was also increased (Figure 6c). These results indicate the existence of a residual afferent and efferent secretory pathway.
To test if OVA sensitization and PNN affects cholinergic sensitivity, we examined the amount of nasal secretion after the administration of pilocarpine in OVA-sensitized rats with/without PNN. The amount of secretion was increased in the OVA-sensitized rats with/without PNN. There was no difference in the amount of secretion between the OVA-sensitized and OVA-unsensitized groups. This result suggested that OVA sensitization with/without PNN did not affect cholinergic sensitivity.
DISCUSSION
Having established a rat model of PNN, the major findings of this study are as follows: PNN induces sensory, sympathetic, and parasympathetic denervation in the nasal respiratory mucosa; reduces nasal secretion consequent to deficient acetylcholine synthesis in cholinergic nerve fibers; and effectively suppresses nasal secretion, but not other allergic symptoms and reactions such as the frequency of sneezing and scratching, eosinophil/mast cell infiltration in the mucosa, cytokine expression, and reactivity to histamine in an allergic rhinitis rat model.
It is notable that our rat PNN model induced sensory, sympathetic, and parasympathetic denervation throughout most of the nasal respiratory mucosa. A previous study used retrograde neuronal tracers to demonstrate that the rat nasal respiratory mucosa receives sympathetic fibers from the superior cervical ganglion, parasympathetic fibers from the pterygopalatine and otic ganglia, and sensory innervation from the trigeminal ganglion.18, 19 The study by Grote et al,20 which is apparently the only previously published study regarding posterior nasal nerve transection, demonstrated that the posterior nasal nerve constitutes the main pathway through which postganglionic sympathetic and parasympathetic fibers approach the nose. These data support our findings that PNN could successfully denervate sensory, sympathetic, and parasympathetic nerves in the nasal respiratory mucosa.
PNN-induced submucosal nasal gland and goblet cell hyperplasia and upregulated Muc5ac expression in the nasal septum. The glands were intensely stained with PAS but not by Alcian blue, suggesting the accumulation of neutral mucin. We further performed immunostaining for MUC5AC and MUC5B. However, we could not obtain reliable results because of high nonspecific staining (data not shown). We also performed qPCR of both Muc5ac and Muc5b, and found the difference in mRNA level only in Muc5ac. Therefore, the detailed component of mucin remains unclear. Our results are consistent with those of Norlander et al,21 who surgically denervated the nasal mucosa in rabbits through an unselective regional sectioning of sensory and parasympathetic nerves and observed enlarged mucosal glands containing increased numbers of zymogen granules, along with compressed cell nuclei and mitochondrial displacement.21 This finding by Norlander and colleagues21 suggested that surgical denervation of the nasal mucosa might cause an imbalance between mucin synthesis and secretory capacity. On the other hand, in our rat model, the submucosal glands in the lateral nasal wall were mildly atrophied on the PNN-treated side, compared with the untreated side. Similar findings have been reported in a study of selective parasympathetic denervation of the submandibular gland in rabbits.22 It remains unclear why the nasal glands in the septum and the lateral nasal wall showed different responses to PNN. One possibility is that the nasal septum is innervated by multiple parasympathetic inputs that are not affected by PNN. Airway inflammation, which evokes increases in goblet cell numbers and in mucin production,23 might be associated with the goblet cell hyperplasia and upregulated Muc5ac expression observed after PNN.
PNN induced the depletion of ChAT immunoreactivity in the nasal mucosa, which indicated denervation of the cholinergic fibers. By contrast, PNN did not affect the expression of the acetylcholine receptor M3, which has an important role in nasal gland secretion.17, 24, 25 These results suggest that the PNN-induced decrease in nasal secretion is likely caused by an attenuated release of acetylcholine from cholinergic fibers rather than by direct changes in the target secretory glands. The administration of the cholinergic agent agonist pilocarpine increased nasal secretion on the PNN-treated and -untreated sides, whereas the administration of the cholinesterase inhibitor neostigmine bromide increased nasal secretion only on the untreated side. These results further support the hypothesis that acetylcholine receptors in the nasal glands function normally, even after PNN.
In humans, PNN effectively treats rhinorrhea, sneezing, and nasal obstruction associated with allergic rhinitis, and it suppresses local inflammatory cell infiltration and related cytokine production in the nasal mucosa.9 We therefore initially hypothesized that PNN would reduce at least some aspects of the allergic reaction. In our OVA-sensitized allergic rhinitis model, PNN unexpectedly suppressed nasal secretion but no other allergic symptoms and reactions such as sneezing, scratching, eosinophil and mast cell infiltration, mucosal, cytokine expression, and reactivity to histamine. These results indicate that the posterior nasal nerve does not have an essential role in the orchestration of the allergic reaction, and that a histamine-mediated allergic reaction occurs, even after PNN.
Our histamine and pilocarpine experiments on nasal secretion did not demonstrate OVA sensitization-induced hyperresponsiveness to these agents. It is noteworthy that PNN did not suppress histamine-induced allergic symptoms and nasal hypersecretion. Furthermore, the contralateral histamine provocation experiment suggested residual histamine responsiveness for afferent and efferent secretory pathways. The most likely explanation for these findings is that a minor sensory and parasympathetic efferent pathway exists that does not pass the posterior nasal nerve. Our analysis showed that PGP 9.5 immunoreactivity remained in the anterior end of the nasal cavity after PNN. Sensory fibers innervated in the nasal mucosa passes through the posterior nasal nerve and the nasopalatine and ethmoid nerves. Recent human studies have also demonstrated that autonomic innervation from the pterygopalatine ganglion is provided by the posterior nasal nerve and by other multiple pathways such as the accessory posterolateral nerve.26, 27 These neural components may be involved in histamine-mediated allergic symptoms and nasal secretion after PNN. If this is the situation, then it follows that the effect of histamine at the dose we used is stronger than that of OVA provocation because nasal hypersecretion by OVA provocation was suppressed by PNN. These results are inconsistent with a VN study by Konno et al28 in which nasal secretion induced by histamine provocation was decreased after VN. The reason for this discrepancy may be species differences between humans and rats.
Recent studies have reported an interaction between the nervous system and immune system.29, 30, 31, 32 For example, hyperinnervation with increased expression of neuropeptides is correlated with allergic inflammation in the nasal mucosa of allergic rhinitis.33 Furthermore, experimental studies of the human nasal mucosa showed that SP increases allergen-induced eosinophil accumulation,34 and that SP upregulates mRNA for proinflammatory cytokines such as interleukin1 beta, which is an additional stimulus in allergic inflammation.35 However, our results did not support the hypothesis that hyperinnervation and the increased expression of neuropeptides directly induce the allergic inflammation; and neither increased eosinophil and mast cell infiltration nor increased expression of inflammatory cytokines were suppressed by PNN, despite considerable denervation and greatly reduced neuropeptide in the nasal mucosa after PNN. Further experimental studies are necessary to address the issue of the interaction between the nervous system and allergic inflammation in allergic rhinitis.
It is important to recognize the limitations of this study. First, it is possible that interspecies differences (ie, human vs rat) in posterior nasal nerve innervation and the surgical PNN procedure may have caused a discrepancy between our results and those of human studies in which PNN was reported to effectively treat hypersensitivity. However, the improvements in sneezing reported in humans subjected to PNN might also have been enhanced by other concurrent surgeries such as septoplasty and turbinectomy.36 Second, we chose the septal respiratory mucosa as the main area for quantitative analysis to take its advantage of its flat shape and because interindividual structural variability is small. However, the septal mucosa is generally not the site of clinical allergic rhinitis pathophysiology and is innervated by multiple parasympathetic inputs aside from the PNN. The results of measuring allergic symptoms such as sneezing, scratching, and nasal secretion should reflect the allergic reaction of the nasal septum and the whole nasal cavity.
In summary, our study revealed the effect of mucosal denervation by PNN on the pathophysiology of allergic rhinitis. We developed a rat model of PNN in which we could induce sensory, sympathetic, and parasympathetic denervation in the nasal respiratory mucosa. In an allergic rhinitis rat model, PNN effectively suppressed nasal secretion but had no effect on nasal hypersensitivity. Allergic rhinitis-related mucosal reactions may occur in a denervated mucosa, despite the absence of nerve fibers and neuropeptides. Our data accordingly suggested that the peripheral nerve of nasal cavity might not be primarily responsible for the regulation of allergic reactions. Furthermore, our rat model would be a useful tool with which to study the role of the nasal nervous system and the pathophysiology of neuroimmune interactions in allergic rhinitis.
References
Bousquet J, Khaltaev N, Cruz AA et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy 2008;63:8–160.
Okubo K, Kurono Y, Fujieda S et al. Japanese guideline for allergic rhinitis. Allergol Int 2014;63:357–375.
Singh K, Axelrod S, Bielory L . The epidemiology of ocular and nasal allergy in the United States, 1988–1994. J Allergy Clin Immunol 2010;126:e6.
Meltzer EO, Nathan R, Derebery J et al. Sleep, quality of life, and productivity impact of nasal symptoms in the United States: findings from the Burden of Rhinitis in America survey. Allergy Asthma Proc 2009;30:244–254.
Seidman MD, Gurgel RK, Lin SY et al. Clinical practice guideline: allergic rhinitis. Otolaryngol Head Neck Surg 2015;152:S1–S43.
Konno A . Historical, pathophysiological, and therapeutic aspects of vidian neurectomy. Curr Allergy Asthma Rep 2010;10:105–112.
Kanaya T, Kikawada T . Endoscopic posterior nasal neurectomy: an alternative to vidian neurectomy. Clin Exp Allergy Rev 2009;9:24–27.
Kobayashi T, Hyodo M, Nakamura K et al. Resection of peripheral branches of the posterior nasal nerve compared to conventional posterior neurectomy in severe allergic rhinitis. Auris Nasus Larynx 2012;39:593–596.
Ogawa T, Takeno S, Ishino T et al. Submucous turbinectomy combined with posterior nasal neurectomy in the management of severe allergic rhinitis: clinical outcomes and local cytokine changes. Auris Nasus Larynx 2007;34:319–326.
Ikeda K, Yokoi H, Saito T et al. Effect of resection of the posterior nasal nerve on functional and morphological changes in the inferior turbinate mucosa. Acta Otolaryngol 2008;128:1337–1341.
Halderman A, Sindwani R . Surgical management of vasomotor rhinitis: a systematic review. Am J Rhinol Allergy 2015;29:128–134.
Albu S, Trombitas V, Nagy A . Endoscopic microdebrider-assisted inferior turbinoplasty with and without posterior nasal neurectomy. Auris Nasus Larynx 2014;41:273–277.
Spencer SE, Sawyer WB, Wada H et al. CNS projections to the pterygopalatine parasympathetic preganglionic neurons in the rat: a retrograde transneuronal viral cell body labeling study. Brain Res 1990;534:149–169.
Shimizu T, Takahashi Y, Kawaguchi S et al. Hypertrophic and metaplastic changes of goblet cells in rat nasal epithelium induced by endotoxin. Am J Respir Crit Care Med 1996;153:1412–1418.
Petersson G, Malm L, Rosengren E et al. Hyperosmolarity but not histamine evokes secretion of nasal fluid in the rat. Eur J Pharmacol 1989;161:37–43.
Shimizu T, Shimizu S, Hattori R et al. A mechanism of antigen-induced goblet cell degranulation in the nasal epithelium of sensitized rats. J Allergy Clin Immunol 2003;112:119–125.
Belmonte KE . Cholinergic pathways in the lungs and anticholinergic therapy for chronic obstructive pulmonary disease. Proc Am Thorac Soc 2005;2:297–304.
Grunditz T, Uddman R, Sundler F . Origin and peptide content of nerve fibers in the nasal mucosa of rats. Anat Embryol (Berl) 1994;189:327–337.
Anton F, Peppel P . Central projections of trigeminal primary afferents innervating the nasal mucosa: a horseradish peroxidase study in the rat. Neuroscience 1991;41:617–628.
Grote JJ, Juijpers W, Huygen PL . Selective denervation of the autonomic nerve supply of the nasal mucosa. Acta Otolaryngol 1975;79:124–132.
Norlander T, Bolger WE, Stierna P et al. A comparison of morphological effects on the rabbit nasal and sinus mucosa after surgical denervation and topical capsaicin application. Eur Arch Otorhinolaryngol 1996;253:205–213.
Kyriacou K, Garrett JR . Morphological changes in the rabbit submandibular gland after parasympathetic or sympathetic denervation. Arch Oral Biol 1988;33:281–290.
Curran DR, Cohn L . Advances in mucous cell metaplasia: a plug for mucus as a therapeutic focus in chronic airway disease. Am J Respir Cell Mol Biol 2010;42:268–275.
Nakaya M, Yuasa T, Usui N . Immunohistochemical localization of subtypes of muscarinic receptors in human inferior turbinate mucosa. Ann Otol Rhinol Laryngol 2002;111:593–597.
Baraniuk JN . Neurogenic mechanisms in rhinosinusitis. Curr Allergy Asthma Rep 2001;1:252–261.
Bleier BS, Feldman R, Sadow PM et al. The accessory posterolateral nerve: an immunohistological analysis. Am J Rhinol Allergy 2012;26:271–273.
Bleier BS, Schlosser RJ . Endoscopic anatomy of the postganglionic pterygopalatine innervation of the posterolateral nasal mucosa. Int Forum Allergy Rhinol 2011;1:113–117.
Konno A, Terata N, Okamoto Y et al. The role of chemical mediators and mucosal hyperreactivity in nasal hypersecretion in nasal allergy. J Allergy Clin Immunol 1987;79:620–627.
Van Gerven L, Boeckxstaens G, Hellings PW . Up-date on neuro-immune mechanisms involved in allergic and non-allergic rhinitis. Rhinology 2012;50:227–235.
Undem BJ, Taylor-Clark T . Mechanisms underlying the neuronal-based symptoms of allergy. J Allergy Clin Immunol 2014;133:1521–1534.
Sarin S, Undem B, Sanico A et al. The role of the nervous system in rhinitis. J Allergy Clin Immunol 2006;118:999–1014.
Chiu IM, von Hehn CA, Woolf CJ . Neurogenic inflammation and the peripheral nervous system in host defense and immunopathology. Nat Neurosci 2012;15:1063–1067.
Knipping S, Holzhausen HJ, Riederer A et al. Allergic and idiopathic rhinitis: an ultrastructural study. Eur Arch Otorhinolaryngol 2009;266:1249–1256.
Fajac I, Braunstein G, Ickovic MR et al. Selective recruitment of eosinophils by substance P after repeated allergen exposure in allergic rhinitis. Allergy 1995;50:970–975.
Okamoto Y, Shirotori K, Kudo K et al. Cytokine expression after the topical administration of substance P to human nasal mucosa. The role of substance P in nasal allergy. J Immunol 1993;151:4391–4398.
Mori S, Fujieda S, Igarashi M et al. Submucous turbinectomy decreases not only nasal stiffness but also sneezing and rhinorrhea in patients with perennial allergic rhinitis. Clin Exp Allergy 1999;29:1542–1548.
Acknowledgements
We thank Koichi Miyazawa for animal care, and Atsuko Tsuyuzaki for her technical assistance. This work was supported by Grant-in-Aid for Scientific Research (grant number 25893055 and 15K20185) from the Japan Society for the Promotion of Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
In this study, the authors developed a rat model of posterior nasal neurectomy, which is characterized by the depletion of nerve fibers, choline acetyltransferase, and neuropeptides in the nasal respiratory mucosa. Denervation of the nasal mucosa induced by posterior nasal neurectomy suppresses nasal secretion, not hypersensitivity, in an allergic rhinitis model.
Rights and permissions
About this article
Cite this article
Nishijima, H., Kondo, K., Toma-Hirano, M. et al. Denervation of nasal mucosa induced by posterior nasal neurectomy suppresses nasal secretion, not hypersensitivity, in an allergic rhinitis rat model. Lab Invest 96, 981–993 (2016). https://doi.org/10.1038/labinvest.2016.72
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2016.72
This article is cited by
-
Effect of Silver Nitrate Cauterisation of Nasal Mucosa on Quality-of-Life and Histology in Patients with Intractable Chronic Rhinitis
Indian Journal of Otolaryngology and Head & Neck Surgery (2022)
-
Long-Term Effects of Combined Submucous Turbinectomy and Posterior Nasal Neurectomy in Patients with Allergic Rhinitis
SN Comprehensive Clinical Medicine (2019)
-
Glycogen depletion can increase the specificity of mucin detection in airway tissues
BMC Research Notes (2018)
-
Concentration-dependent effects of PM2.5 mass on expressions of adhesion molecules and inflammatory cytokines in nasal mucosa of rats with allergic rhinitis
European Archives of Oto-Rhino-Laryngology (2017)