Abstract
Intestinal dysbiosis has been reported in patients with colorectal cancer, and there is a high prevalence of Escherichia coli belonging to B2 phylogroup and producing a genotoxin, termed colibactin. Macrophages are one of the predominant tumor-infiltrating immune cells supporting key processes in tumor progression by producing protumoral factors such as cyclooxygenase-2 (COX-2). Here, we investigated whether B2 E. coli colonizing colon tumors could influence protumoral activities of macrophages. In contrast to commensal or nonpathogenic E. coli strains that were efficiently and rapidly degraded by macrophages at 24 h after infection, colon cancer-associated E. coli were able to resist killing by human THP-1 macrophages, to replicate intracellularly, and to persist inside host cells until at least 72 h after infection. Significant increases in COX-2 expression were observed in macrophages infected with colon cancer E. coli compared with macrophages infected with commensal and nonpathogenic E. coli strains or uninfected cells at 72 h after infection. Induction of COX-2 expression required live bacteria and was not due to colibactin production, as similar COX-2 levels were observed in macrophages infected with the wild-type colon cancer-associated E. coli 11G5 strain or a clbQ mutant unable to produce colibactin. Treatment of macrophages with ofloxacin, an antibiotic with intracellular tropism, efficiently decreased the number of intracellular bacteria and suppressed bacteria-induced COX-2 expression. This study provides new insights into the understanding of how tumor- infiltrating bacteria could influence cancer progression through their interaction with immune cells. Manipulation of microbes associated with tumors could have a deep influence on the secretion of protumoral molecules by infiltrating macrophages.
Similar content being viewed by others
Main
Colorectal cancer (CRC) is one of the most commonly diagnosed malignancies worldwide, making it the fourth most common cause of cancer deaths throughout the world.1 CRC is a heterogeneous disease, including at least three major forms: hereditary, sporadic, and colitis-associated CRC. A large body of evidence indicates that genetic mutations, epigenetic changes, chronic inflammation, diet, and lifestyle deeply affect CRC onset.2, 3 In addition to these factors, gut microbiota dysbiosis has been reported in CRC patients.4, 5, 6, 7, 8, 9 Recent pyrosequencing analysis of CRC-associated bacterial microbiota has revealed dysbiosis with, in particular, overrepresentation of Fusobacterium and Bacteroides.10, 11, 12, 13, 14 In addition, our group and others have shown that colonic adenomas, carcinomas, and the mucosa of CRC patients are abnormally colonized by Escherichia coli belonging to the B2 phylogroup, with a high prevalence of E. coli producing a genotoxin, termed colibactin, encoded by the pks genomic island.15, 16, 17, 18, 19, 20 It has been recently demonstrated that cells that survive infection with colibactin-producing E. coli display hallmarks of cellular senescence accompanied with production of reactive oxygen species and secretion of pro-inflammatory cytokines, chemokines, and proteases, inducing bystander genotoxic and oncogenic effects.21, 22
Macrophages are one of the predominant components of murine and human tumor-infiltrating cells. By integrating signals present in the tumor microenvironment, macrophages acquire a new transcriptional program leading to secretion of the molecules displaying protumoral activities and hence supporting the key processes in tumor progression, including proliferation and survival of cancer cells, angiogenesis, immunosuppression, invasion, and metastasis.23, 24 Among these molecules, prostaglandin E2 (PGE2) is one of the major actors that orchestrate the protumoral response of macrophages.25, 26 Elevated PGE2 biosynthesis in tumor results from upregulation of cyclooxygenase-2 (COX-2). Role of COX-2 in CRC is particularly supported by its elevated expression found in ∼50% of adenomas and 85% of adenocarcinomas,27 its association with worse survival among CRC patients,28 and the efficiency of nonsteroidal anti-inflammatory drugs (NSAIDs) and selective COX-2 inhibitors (COXIBs) to reduce the occurrence of sporadic CRC, and the number and size of adenomas in familial adenomatous polyposis patients and in APC knockout mice.29 COX-2 expression is regulated at both transcriptional and posttranscriptional levels and mitogen-activated proteins kinase (MAPK) regulation has been reported to play a key role in regulation of COX-2 expression.30, 31, 32
In this study, we hypothesized that B2 E. coli-colonizing colon cancer tumors could influence protumoral activities of macrophages. We showed that colon cancer-associated E. coli survive, replicate, and persist within human macrophages and that macrophages infected with colon cancer E. coli expressed COX-2 at least until 72 h after infection. We identified the p38 MAPK signaling pathway as a target to control the number of intracellular bacteria within macrophages and to limit expression of the protumoral factor COX-2.
MATERIALS AND METHODS
Bacterial Strains
B2 E. coli strains used in this study were isolated from the tumors of colon cancer patients as previously described.19, 33 Bacteria were grown routinely in Luria Bertani (LB) broth or on LB agar plates overnight at 37 °C.
Gentamicin Treatment and Heat Killing of Bacteria
Bacteria were suspended at DO=0.1 in PBS and were incubated for 30 min with gentamicin (Gm) at 5 mg/ml or incubated for 30 min at 65 °C before infection. Killing of bacteria was checked by plating on LB agar.
Construction of Isogenic Mutant
The 11G5ΔclbQ isogenic mutant was generated with a PCR product by using the method modified by Chaveroche et al.22, 34 The basic strategy was to replace a chromosomal sequence with a selectable antibiotic resistance gene, spectinomycin, generated by PCR.
Cell Culture
The human monocytic THP-1 cell line was maintained in an atmosphere containing 5% CO2 at 37 °C in the culture medium recommended by ATCC. THP-1 monocytes were differentiated into macrophages by treatment with 20 ng/ml phorbol myristate acetate (PMA) for 18 h. Primary bone marrow-derived macrophages (BMDMs) were obtained from wild-type and TLR-4 knockout BALB/c mice, extracted from tibia and femur, and grown as previously described.35
Antibodies and Reagents
For western blot analysis, rabbit anti-GAPDH monoclonal antibody, rabbit anti-ERK1/2 polyclonal antibody, rabbit anti-phospho ERK1/2 monoclonal antibody, rabbit anti-p38 polyclonal antibody, rabbit anti-phospoho p38 monoclonal antibody, rabbit anti-SAPK/JNK monoclonal antibody, rabbit anti-phospho SPAK/JNK monoclonal antibody, rabbit anti-caspase-3 monoclonal antibody, and rabbit anti-PARP1 monoclonal antibody were purchased from Cell Signaling. Goat anti-COX-2 polyclonal antibody was purchased from Santa Cruz Biotechnology. Inhibitor for SAPK/JNK (SP600125) signaling pathway was purchased from Cell Signaling, and inhibitor for p38 signaling pathway (SB203580) was purchased from Calbiochem. For macrophage survival assay, ofloxacin and gentamicin were purchased from Euromedex and PMA was purchased from Sigma. For immunofluorescence analysis, bacteria were labeled with goat anti-E. coli polyclonal antibody (AbD Serotec) and Alexa 488-labeled anti-goat antibody (Invitrogen). For TLR-4 neutralization, macrophages were treated with goat anti-TLR-4 antibody (R&D Systems). Actin cytoskeleton was stained using TRITC-labeled phalloidin (Sigma). Hoechst 33342 was purchased from Sigma.
Macrophage Survival Assay
The numbers of intracellular bacteria within macrophages were determined by the gentamicin protection assay.36 Briefly, THP-1 macrophages and BMDMs were infected for 20 min. Infected cells were then washed and incubated with culture medium containing gentamicin at 50 μg/ml for 40 min (1 h after infection) or 24 h (24 h after infection). When indicated, macrophages were treated for 1 h before infection with anti-TLR-4 antibody or an isotype antibody at 7.5 μg/ml, and infection was performed in the presence of the antibodies. When indicated, cells were treated with ofloxacin at 4 μg/ml in the gentamicin-containing medium at 6 h after infection. When indicated, the inhibitors of JNK (SP600125, 50 μM) and p38 (SB203580, 10 μM) signaling pathways were added in the gentamicin-containing medium at 1 h after infection.
Enzyme-Linked Immunosorbent Assays for PGE2 Quantification
The amount of PGE2 released in the culture supernatant was determined by enzyme-linked immunosorbent assay (Cayman Chemical). PGE2 concentration was assessed according to the manufacturer’s instructions.
XTT Cell Viability Assay
Cells were plated at a concentration of 2 × 104 cells/well in 96-well plates in 100 μl of cell culture medium and infected at a MOI of 10 as described above or incubated with staurosporin at 200 nM for 18 h. At 24, 48, or 72 h after infection, cell viability was evaluated using a XTT cell viability assay kit (Biotium) according to the manufacturer’s instructions.
Immunoblot Analysis
Whole-cell protein extracts were prepared by using lysis buffer (25 mM Tris pH 7.5; 1 mM EDTA; 5 mM MgCl2; 1% NP-40; 10% glycerol; 15 mM NaCl; 10 μl/ml sodium orthovanadate; and 1 mM PMSF). Proteins were separated on SDS/PAGE gels, transferred to nitrocellulose membrane, blocked for 2 h in Tris-buffered saline (TBS) solution containing 2% BSA, and probed overnight with primary antibodies and for 2 h with secondary HRP-coupled antibodies. GAPDH levels were used to normalize protein quantity. After membrane revelation using the ECL detection kit (Amersham), quantification was performed with ImageJ software.
Confocal Microscopy
Briefly, cells were fixed with 4% paraformaldehyde and immunostained overnight at 4 °C with the indicated specific primary antibodies. Cells were then incubated for 1 h with secondary antibodies. The slides were examined with a Zeiss LSM 510 Meta confocal microscope. Each confocal microscopy image is representative of at least three independent experiments.
Statistical Analysis
Data were expressed as means. Error bars represent s.e.m. Where appropriate, statistical analyses were done using ANOVA or Mann–Whitney using GraphPad Prism 6 software. A P-value of 0.05 was considered significant.
RESULTS
Colon Cancer-Associated E. coli Strains Survive, Replicate, and Persist within Human Macrophages
The ability of 19 strains of colon cancer-associated E. coli belonging to B2 phylogroup to resist killing by macrophage was assessed in human monocyte-derived THP-1 macrophages. The numbers of intracellular bacteria were determined at 1 and 24 h after infection (Figure 1a and b). No statistically significant difference was observed in the numbers of intracellular B2 E. coli at 1 h after infection, indicating similar internalization rates of bacteria within macrophages (P=0.97; Figure 1a). In contrast to the commensal E. coli ED1a and Nissle 1917 strains or the nonpathogenic E. coli K-12 C600 strain, which were efficiently killed by macrophages, 16/19 (84%) colon cancer-associated E. coli strains were able to survive and/or replicate within macrophages with percentages of intracellular bacteria at 24 h compared with 1 h after infection, considered as 100%, ranging from 137.30±7.67% to 746.90±334.70% (Figures 1b and 3a ). This result was confirmed by confocal microscopic examination of infected macrophages. At 24 h after infection, high numbers of intracellular bacteria were observed within macrophages infected with the E. coli 11G5, 10D12, and 16C1 strains, whereas only few bacteria were observed within E. coli ED1a strain-infected cells (Figure 1c). Analysis of E. coli 11G5, 10D12, and 16C1 strain-infected macrophages by transmission electron microscopy (TEM) revealed the existence of two types of bacteria-containing compartments, one containing only a few bacteria and another containing numerous bacteria (Figure 2). Survival of colon cancer-associated E. coli within THP-1 macrophages did not induce apoptosis as revealed by absence of cleaved Caspase-3 and PARP-1 in infected macrophages at 24 h after infection (Figure 1d). Cleaved Caspase-3 and PARP-1 were detected in macrophages incubated with staurosporin, an inducer of apoptosis (Figure 1d).
Ability of colon cancer-associated E. coli to survive within macrophages. Human THP-1 macrophages were infected at a MOI of 100 with E. coli strains isolated from tumors of CRC patients or the nonpathogenic B2 E. coli ED1a strain. (a) The number of bacteria internalized within macrophages was determined at 1 h after infection. Results were expressed as numbers of colony-forming units (CFUs) per well. (b) The number of intracellular bacteria within macrophages was determined at 24 h after infection. Results were expressed as the number of intracellular bacteria at 24 h after infection relative to that obtained at 1 h after infection, taken as 100%. For all experiments, data are means±s.e.m. of three independent experiments. (c) Confocal microscopic examination of cells infected with the nonpathogenic E. coli ED1a strain or the colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains at 24 h after infection. The actin cytoskeleton and nucleus of cells were stained using TRITC-labeled phalloidin and Hoescht, respectively. (d) Cells were infected with the colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains and the nonpathogenic E. coli ED1a strain. Caspase-3 and PARP-1 cleavage were analyzed by western blot at 24 h after infection. As a positive control for apoptosis, cells were treated for 3 h with staurosporin at 200 nM.
Transmission electronic microscopic examination of colon cancer-associated E. coli-containing vacuoles. THP-1 macrophages were infected at a MOI of 100 with the colon cancer-associated E. coli 11G5 (a), 10D12 (b), and 16C1 (c) strains, and infected macrophages were analyzed by TEM at 24 h after infection. TEM examination revealed two kinds of vacuoles, one containing a few bacteria (left panels) and another containing numerous bacteria (right panels). Bars=2 μm.
Determination of intracellular CFU number in THP-1 macrophages and TEM examination of infected macrophages at longer time after infection revealed that the colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains persist within macrophages until at least 72 h after infection (Figure 3a and b). Persistence within THP-1 macrophages at longer time after infection was also observed for the Crohn’s disease-associated adherent-invasive E. coli (AIEC) reference strain LF82, which has been already described to persist in other macrophage cell lines.37 No statistical difference in cell viability was observed between uninfected and infected macrophages by using XTT assay (Figure 3c), indicating that intracellular persistence of the bacteria does not induce host cell death.
Intramacrophagic persistence of E. coli strains isolated from colon cancer patients. THP-1 macrophages were infected at a MOI of 10 with the colon cancer-associated E. coli 11G5, 10D12, or 16C1 strains, the Crohn’s disease-associated E. coli reference strain LF82, the commensal E. coli ED1a and Nissle 1917 strains, or the laboratory E. coli K-12 C600 strain. (a) The numbers of bacteria internalized within macrophages were determined at 1, 24, 48, and 72 h after infection. Results were expressed as numbers of colony-forming units (CFUs) per well. (b) Infected macrophages were analyzed by TEM at 72 h after infection. Bars=2 μm. (c) Viability of uninfected and infected cells was assessed at 24, 48, and 72 h after infection using a XTT cell viability assay kit. As a positive control for cell death, cells were treated for 18 h with staurosporin (STS) at 200 nM.
Colon Cancer-Associated E. coli Bacteria Induce COX-2 Expression in Human Macrophages
We examined whether colon cancer-associated E. coli strains are able to modulate COX-2 expression and, as a consequence, PGE2 secretion. For this, we focused on three colon cancer-associated E. coli strains displaying strong ability to survive within macrophages: 11G5, 10D12, and 16C1. As shown in Figure 4a and b, these strains induced COX-2 expression and PGE2 secretion in THP-1 macrophages. In addition, we showed that macrophages treated with gentamicin- and heat-killed colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains produced significantly less amount of COX-2 than macrophages infected with live bacteria (P<0.05; Figure 4c), indicating that live bacteria are required to induce COX-2 expression.
COX-2 expression and PGE2 secretion by colon cancer-associated E. coli-infected macrophages. THP-1 macrophages were infected with the colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains. (a) COX-2 expression was analyzed by western blot at 24 h after infection. Quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. (b) Levels of PGE2 secreted in cell supernatants were quantified by ELISA. (c) COX-2 expression was analyzed at 24 h after infection in macrophages infected with living or dead (gentamicin (Gm) or heat killed) bacteria by western blot. Quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. (d) Bone marrow-derived macrophages were prepared from wild-type and TLR-4 knockout mice and infected with the colon cancer-associated E. coli 11G5 strain. COX-2 expression was analyzed by western blot at 24 h after infection. Quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. (e) Human THP-1 macrophages were treated before infection with anti-TLR4 antibody or with an isotype control antibody. Infection with the E. coli 11G5 strain was performed in the presence of the antibodies. COX-2 expression was analyzed by western blot at 24 h after infection. Quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. For all experiments, data are means±s.e.m. of three independent experiments.
The TLR4-dependent signaling pathways have been involved in induction of COX-2 expression by the uropathogenic E. coli J96 strain.38 We investigated whether induced COX-2 expression by colon cancer-associated E. coli results from extracellular activation of TLR4 signaling and/or from stimulation by intracellular bacteria. Macrophages prepared from wild-type mice and TLR4 knockout mice and infected with the colon cancer-associated E. coli 11G5 strain expressed similar levels of COX-2 (P=0.33; Figure 4d). In addition, no significant modification of COX-2 expression was observed in 11G5-infected THP-1 macrophages treated with TLR4-neutralizing antibodies compared with those treated with isotype control antibodies (Figure 4e), indicating that the E. coli 11G5 strain induces COX-2 expression in a TLR4-independent manner.
Macrophages Infected with Colon Cancer-Associated E. coli Express COX-2 for Several Days
By infecting cells with the colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains at different MOIs, we showed that the level of COX-2 expression was statistically correlated with the load of intracellular bacteria in THP-1 macrophages at 24 h after infection (11G5, r=0.9333; 10D12, r=0.9167; and 16C1, r=0.9833), suggesting a link between intracellular bacteria and COX-2 expression by infected macrophages (Figure 5a–c). Interestingly, at 72 h after infection, we observed that macrophages infected with colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains expressed significant increased COX-2 levels compared with uninfected cells and macrophages infected with the commensal E. coli ED1a and Nissle 1917 strains and the nonpathogenic E. coli K-12 C600 strain (Figure 5d). COX-2 levels in macrophages infected with commensal or laboratory E. coli strains, which are killed by macrophages as early as 24 h after infection, were similar to that of uninfected macrophages (Figure 5d). In order to investigate whether the ability of intracellular bacteria to induce COX-2 was unique to colon cancer-associated E. coli, we analyzed COX-2 expression in THP-1 macrophages infected with the AIEC reference strain LF82 that persist within macrophages at 72 h after infection (Figure 3a). Results showed that at 72 h after infection, THP-1 macrophages infected with LF82 bacteria expressed levels of COX-2 significantly increased compared with uninfected and macrophages infected with commensal and laboratory E. coli strains, and similar to those of macrophages infected with colon cancer-associated E. coli strains (Figure 5d).
COX-2 expression in infected macrophages is correlated with the presence of intracellular bacteria. THP-1 macrophages were infected with the colon cancer-associated E. coli 11G5, 10D12, or 16C1 strains, the Crohn’s disease-associated E. coli reference strain LF82, the commensal E. coli ED1a and Nissle 1917 strains, or the laboratory E. coli K-12 C600 strain. (a, b) THP-1 macrophages were infected at MOIs of 10, 25, or 100. (a) The number of intracellular bacteria within macrophages was determined at 24 h after infection. (b) COX-2 expression was analyzed at 24 h after infection, and quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. (c) Correlation between the number of intracellular bacteria and the ratio of COX2/GAPDH levels determined by Spearman’s test. (d) THP-1 macrophages were infected at a MOI of 10. COX-2 expression was analyzed at 72 h after infection, and quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. (e, f) Infected macrophages were treated with ofloxacin at 6 h after infection and until 24 h after infection. (e) The numbers of intracellular bacteria were determined at 1, 6, and 24 h after infection. Results were expressed as CFUs per well. (f) COX-2 expression was analyzed at 24 h after infection, and quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. For all experiments, data are means±s.e.m. of three independent experiments.
We analyzed whether the induction of COX-2 expression by these strains could be suppressed by pharmacologically reducing the intracellular bacterial load in infected macrophages. Human THP-1 macrophages were treated at 6 h after infection with ofloxacin, a fluoroquinolone antibiotic able to penetrate eukaryotic cells and thus to target intracellular bacteria. Decrease in intracellular bacterial load by ofloxacin treatment was associated with significant reduction of COX-2 expression (P=0.05; Figure 5e and f). Ofloxacin treatment did not modify COX-2 expression induced by LPS stimulation in THP-1 cells (Supplementary Figure S1). Altogether, these results demonstrated that THP-1 macrophages infected with colon cancer-associated E. coli express COX-2 for several days and that antibiotic treatment targeting intracellular bacteria could efficiently suppress COX-2 expression.
Colibactin Is Not Involved in the Induction of COX-2 Expression by Colon Cancer-Associated E. coli
As the E. coli 11G5, 10D12, and 16C1 strains harbor the pks genomic island encoding colibactin and as colibactin-producing E. coli have been shown to induce inflammation and oxidative stress as a consequence of senescence promotion,21, 22, 33 we generated an E. coli 11G5 mutant strain unable to produce colibactin, by deleting clbQ, and analyzed its ability to survive within macrophages and to induce COX-2 expression. Similar levels of intracellular wild-type 11G5 and 11G5ΔclbQ bacteria were observed in THP-1 macrophages at 1 and 24 h after infection (P=0.75; Figure 6a). In addition, deletion of clbQ did not significantly modify the level of COX-2 expression induced by 11G5 bacteria (P=0.50; Figure 6b). These results indicate that the ability of the E. coli 11G5 strain to resist killing by macrophage and to promote COX-2 expression is independent of colibactin production.
Colibactin is not involved in colon cancer-associated E. coli-induced COX-2 expression. THP-1 macrophages were infected with the E. coli 11G5 and 11G5ΔclbQ strains. (a) The numbers of bacteria internalized within macrophages were determined at 1 and 24 h after infection. Results were expressed as CFUs per well. (b) COX-2 expression was analyzed at 24 h after infection, and quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. For all experiments, data are means±s.e.m. of three independent experiments.
Intracellular Number of Colon Cancer-Associated E. coli and Bacteria-Induced COX-2 Expression Are Controlled by p38 MAPK
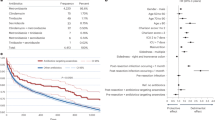
MAPK signaling pathways have been involved in transcriptional regulation of COX-2 expression.39 The colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains induced phosphorylation of JNK and p38 MAPKs, indicating activation of these signaling pathways (Figure 7a). No activation of ERK signaling pathway was observed (Figure 7a). To determine the contribution of JNK and p38 MAPK signaling pathway in the bacteria-induced COX-2 expression and in the intracellular persistence of colon cancer-associated E. coli, THP-1 macrophages were incubated with specific inhibitors of JNK (SP600125) and p38 (SB203580) after the infection period. These treatments had no effect on cell viability (Supplementary Figure S2). COX-2 expression was decreased in macrophages treated with specific inhibitors of p38 and JNK signaling pathways and infected with the 11G5, 10D12, and 16C1 strains (Figure 7b). Interestingly, significant decrease in the number of intracellular colon cancer-associated bacteria was observed at 24 h after infection only when p38, but not JNK, signaling pathway was inhibited (Figure 7c). Altogether, these results indicate that the p38 MAPK signaling pathway controls both numbers of intracellular bacteria and expression of the protumoral factor COX-2 in THP-1 macrophages infected with colon cancer-associated E. coli.
Role of MAPKs in the control of number of intracellular colon cancer-associated E. coli and in COX-2 induction in infected macrophages. THP-1 macrophages were infected with the colon cancer-associated E. coli 11G5, 10D12, or 16C1 strains. (a) Activation of JNK and p38 MAPK signaling pathways was analyzed by western blot using specific antibodies directed against phosphorylated and total proteins. (b, c) Infected macrophages were treated with specific inhibitors of JNK (SP600125) and p38 (SB203580) signaling pathways at 1 h after infection. (b) COX-2 expression was analyzed at 24 h after infection, and quantification of COX-2 expression relative to GAPDH was displayed below the representative immunoblot. (c) The numbers of intracellular bacteria were determined at 24 h after infection. Results are expressed as CFUs per well. For all experiments, data are means±s.e.m. of three independent experiments.
DISCUSSION
Macrophages are one of the most predominant tumor-infiltrating cell types and their role in cancer progression has been firmly established. By secreting a variety of factors including COX-2/PGE2, macrophages promote key steps of carcinogenesis. Acquisition of protumoral function by macrophages is directly influenced by tumor microenvironment. As several independent studies have reported high colonization by E. coli of adenomas and carcinomas in colon cancer patients,15, 16, 17, 18, 19 we have analyzed the effect of such a microbial environmental factor on COX-2 expression in human macrophages.
Phagocytic uptake of pathogens by macrophages results in the formation of vacuoles that rapidly evolve into bactericidal organelles termed phagolysosomes through interactions with vesicles of the endosomal system. Pathogens often use phagocytic cells, in particular macrophages, to gain access to an intracellular niche where they can survive and replicate.40, 41, 42 Shortly after internalization, many intracellular pathogens hijack the intracellular defense mechanisms to either subvert or delay the maturation process (eg, Mycobacterium tuberculosis, Salmonella enterica Typhimurium, Brucella abortus, and Legionella pneumophila), or to escape from their vacuoles (eg, Shigella flexneri and Listeria monocytogenes) and induce macrophage apoptosis.41, 43 In this study, we showed that the great majority of B2 E. coli strains isolated from colon cancer patients are able to survive, replicate, and persist within human macrophages for several days and do not induce host cell death. Interestingly, we demonstrated that the p38 MAPK signaling pathway is involved in the control of intracellular bacteria. Indeed, specific inhibition of p38 signaling pathway, but not that of JNK, induced a decrease in the number of intracellular colon cancer-associated E. coli. It could be speculated that colon cancer-associated E. coli hijack the p38 MAPK signaling pathway to create an intracellular niche where they can survive and replicate. MAPKs are involved in membrane trafficking, and thus control key steps of phagolysosome biogenesis44, 45, 46 and regulate autophagy pathway.47, 48 Some intracellular pathogens hijack MAPK signaling pathways in favor of their survival. For example, intracellular replication of Mycobacterium avium is enhanced by p38 activation, whereas ERK activation has the opposite effect.49 Activation of p38 plays a role in EEA1 exclusion, an early endosomal protein, from M. tuberculosis phagosomes and in inhibiting the maturation of mycobacterial phagosomes.44 Dependence of the survival of Brucella melitensis on p38 and JNK activation has also been reported.50
In macrophages infected with colon cancer-associated E. coli, two kinds of vacuoles were observed, one containing a few bacteria and another containing numerous bacteria. Heterogeneity of intracellular bacterial population has already been reported for Salmonella.35, 51 Indeed, upon entry into macrophages, some Salmonella do not replicate and enter a dormant-like state. It is speculated that these living nonreplicating bacteria could represent a reservoir of persistent bacteria. Besides, some intracellular pathogens have adapted to resist the harsh conditions in the phagolysosomes (eg, Crohn’s disease-associated E. coli),52 and may require lysosomal or autophagosomal interactions to facilitate the delivery of nutrients ensuring their intracellular survival and growth (eg, Brucella abortus and Yersinia).53, 54
COX-2 expression is low and undetectable in normal cells and is induced in response to various stimuli.39 Elevated COX-2 expression is found in most colon cancer tissues and is associated with worse survival among CRC patients.29 We reported here that infection of human macrophages with colon cancer-associated E. coli strains induces COX-2 expression for several days and that targeting intracellular bacteria by using antibiotic allows to reduce COX-2 level. This suggests that intracellular colon cancer-associated E. coli sustain COX-2 expression. However, induction of COX-2 expression by intracellular bacteria is not a unique feature of colon cancer-associated E. coli but rather a property shared by pathogenic E. coli able to persist intracellularly, as we observed that AIEC LF82 persistence in THP-1 macrophages was also associated with COX-2 expression.
Colon cancer-associated E. coli need to be alive to induce COX-2 expression, and the induced COX-2 expression level was correlated with the intracellular bacterial number. Induction of COX-2 expression by other pathogens associated with gastrointestinal cancer has been reported. For example, Helicobacter pylori, a persistent colonizer of the human stomach classified as carcinogen class I, and Bacteroides fragilis, a human anaerobic enterotoxinogen bacteria with oncogenic capabilities, induce COX-2 expression through production of toxins.55, 56 In addition, tumors of ApcMin/+ mice infected with Fusobacterium nucleatum and human fusobacteria-positive colorectal carcinomas highly expressed COX-2.12 Induction of COX-2 expression by pathogenic E. coli has also been reported. Uropathogenic E. coli stimulate COX-2 expression through activation of the pathogen recognition receptor TLR4 by type 1 pili expressed by bacteria.38 We reported here that induction of COX-2 expression by colon cancer-associated E. coli does not require TLR4 as similar COX-2 levels were observed in TLR4-/- and wild-type infected macrophages. Cytotoxic necrotizing factor 1 (CNF), a toxin produced by some isolates of E. coli that cause extraintestinal infections, stimulates COX-2 expression via a RhoA-dependent signaling pathway.57 PCR analysis of the colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains revealed that they do not possess genes encoding CNF. However, these strains harbor the pks genomic island encoding colibactin, a genotoxin that has been associated with protumoral properties of E. coli strains isolated from patients with colon cancer.18 Colibactin triggers senescence in host cells, and this is notably accompanied by production of reactive oxygen species and secretion of proinflammatory cytokines and chemokines.21, 22 Deletion of clbQ gene, which impaired colibactin synthesis, had no effect on induction of COX-2 expression by the colon cancer-associated E. coli 11G5, 10D12, and 16C1 strains in macrophages, indicating that B2 E. coli strains associated with colon cancer can promote protumoral response independently of colibactin production.
Increased levels of COX-2 in macrophages have been reported in human CRC and mouse models of CRC.39, 58, 59, 60, 61 COX-2 expression is regulated at both the transcriptional and posttranscriptional levels, and the signaling pathways involved in COX-2 transcriptional regulation include NF-κB, PI3K/AKT, GSK/β-catenin, and MAPKs.29 High expression of active MAPKs has been observed in the stroma of human colonic adenomatous polyps.61 Involvement of MAPK signaling pathways in induction of COX-2 expression by colon cancer-associated E. coli was revealed by decrease in COX-2 level upon selective inhibition of these signaling pathways. Involvement of pro-inflammatory signaling pathways in COX-2 transcriptional induction by pathogens has been previously reported. Stimulation of COX-2 expression by H. pylori involves activation of p38 MAPK and PKC/c-Src/NF-κB signaling pathways in human gastric cancer cells.56, 62 B. fragilis enterotoxin increases COX-2 expression in a NF-κB-dependent manner in human intestinal epithelial cells.55 In addition, ERK, JNK, and p38 MAPKs are critical for uropathogenic E. coli-induced COX-2 expression in bladder epithelial cells.38
In conclusion, colon cancer-associated E. coli strains belonging to B2 phylogroup are able to resist killing by macrophages and to persist several days after infection, and the presence of intracellular bacteria stimulates COX-2 expression. We identified the p38 MAPK signaling pathway as a target to control the number of intracellular colon cancer-associated E. coli within macrophages and to limit expression of COX-2 induced by these bacteria. Antibiotic treatment, allowing intracellular bacterial clearance, suppressed COX2 expression, suggesting that manipulation of microbes associated with tumors could have a deep influence on the secretion of protumoral molecules by infiltrated macrophages.
References
Ferlay J, Shin HR, Bray F et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2012;127:2893–2917.
Huxley RR, Ansary-Moghaddam A, Clifton P et al. The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of the epidemiological evidence. Int J Cancer 2009;125:171–180.
Rasool S, Kadla SA, Rasool V et al. A comparative overview of general risk factors associated with the incidence of colorectal cancer. Tumour Biol 2013;34:2469–2476.
Dejea C, Wick E, Sears CL . Bacterial oncogenesis in the colon. Future Microbiol 2013;8:445–460.
Zackular JP, Baxter NT, Iverson KD et al. The gut microbiome modulates colon tumorigenesis. MBio 2013;4:e00692–13.
Zhu Q, Gao R, Wu W et al. The role of gut microbiota in the pathogenesis of colorectal cancer. Tumour Biol 2013;34:1285–1300.
Irrazabal T, Belcheva A, Girardin SE et al. The multifaceted role of the intestinal microbiota in colon cancer. Mol Cell 2014;54:309–320.
Sears CL, Garrett WS . Microbes, microbiota, and colon cancer. Cell Host Microbe 2014;15:317–328.
Sobhani I, Tap J, Roudot-Thoraval F et al. Microbial dysbiosis in colorectal cancer (CRC) patients. PLoS One 2011;6:e16393.
Wu S, Rhee KJ, Albesiano E et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat Med 2009;15:1016–1022.
Kostic AD, Gevers D, Pedamallu CS et al. Genomic analysis identifies association of Fusobacterium with colorectal carcinoma. Genome Res 2012;22:292–298.
Kostic AD, Chun E, Robertson L et al. Fusobacterium nucleatum potentiates intestinal tumorigenesis and modulates the tumor-immune microenvironment. Cell Host Microbe 2013;14:207–215.
Castellarin M, Warren RL, Freeman JD et al. Fusobacterium nucleatum infection is prevalent in human colorectal carcinoma. Genome Res 2012;22:299–306.
Toprak NU, Yagci A, Gulluoglu BM et al. A possible role of Bacteroides fragilis enterotoxin in the aetiology of colorectal cancer. Clin Microbiol Infect 2006;12:782–786.
Maddocks OD, Short AJ, Donnenberg MS et al. Attaching and effacing Escherichia coli downregulate DNA mismatch repair protein in vitro and are associated with colorectal adenocarcinomas in humans. PLoS One 2009;4:e5517.
Martin HM, Campbell BJ, Hart CA et al. Enhanced Escherichia coli adherence and invasion in Crohn’s disease and colon cancer. Gastroenterology 2004;127:80–93.
Swidsinski A, Khilkin M, Kerjaschki D et al. Association between intraepithelial Escherichia coli and colorectal cancer. Gastroenterology 1998;115:281–286.
Arthur JC, Perez-Chanona E, Muhlbauer M et al. Intestinal inflammation targets cancer-inducing activity of the microbiota. Science 2012;338:120–123.
Buc E, Dubois D, Sauvanet P et al. High prevalence of mucosa-associated E. coli producing cyclomodulin and genotoxin in colon cancer. PLoS One 2013;8:e56964.
Nougayrede JP, Homburg S, Taieb F et al. Escherichia coli induces DNA double-strand breaks in eukaryotic cells. Science 2006;313:848–851.
Secher T, Samba-Louaka A, Oswald E et al. Escherichia coli producing colibactin triggers premature and transmissible senescence in mammalian cells. PLoS One 2013;8:e77157.
Cougnoux A, Dalmasso G, Martinez R et al. Bacterial genotoxin colibactin promotes colon tumour growth by inducing a senescence-associated secretory phenotype. Gut [Internet] 2014;63:1932–1942.
Qian BZ, Pollard JW . Macrophage diversity enhances tumor progression and metastasis. Cell 2010;141:39–51.
Sica A, Larghi P, Mancino A et al. Macrophage polarization in tumour progression. Semin Cancer Biol 2008;18:349–355.
Wu WK, Sung JJ, Lee CW et al. Cyclooxygenase-2 in tumorigenesis of gastrointestinal cancers: an update on the molecular mechanisms. Cancer Lett 2010;295:7–16.
Wang D, DuBois RN . Pro-inflammatory prostaglandins and progression of colorectal cancer. Cancer Lett 2008;267:197–203.
Eberhart CE, Coffey RJ, Radhika A et al. Up-regulation of cyclooxygenase 2 gene expression in human colorectal adenomas and adenocarcinomas. Gastroenterology 1994;107:1183–1188.
Ogino S, Kirkner GJ, Nosho K et al. Cyclooxygenase-2 expression is an independent predictor of poor prognosis in colon cancer. Clin Cancer Res 2008;14:8221–8227.
Wang D, Dubois RN . The role of COX-2 in intestinal inflammation and colorectal cancer. Oncogene 2010;29:781–788.
Dixon DA, Blanco FF, Bruno A et al. Mechanistic aspects of COX-2 expression in colorectal neoplasia. Recent Results Cancer Res 2013;191:7–37.
Young LE, Dixon DA . Posttranscriptional regulation of cyclooxygenase 2 expression in colorectal cancer. Curr Colorectal Cancer Rep 2010;6:60–67.
Chun KS, Surh YJ . Signal transduction pathways regulating cyclooxygenase-2 expression: potential molecular targets for chemoprevention. Biochem Pharmacol 2004;68:1089–1100.
Raisch J, Buc E, Bonnet M et al. Colon cancer-associated B2 Escherichia coli colonize gut mucosa and promote cell proliferation. World J Gastroenterol 2014;20:6560–6572.
Chaveroche MK, Ghigo JM, d’ Enfert C . A rapid method for efficient gene replacement in the filamentous fungus Aspergillus nidulans. Nucleic Acids Res 2000;28:E97.
Helaine S, Thompson JA, Watson KG et al. Dynamics of intracellular bacterial replication at the single cell level. Proc Natl Acad Sci USA 2010;107:3746–3751.
Bringer MA, Barnich N, Glasser AL et al. HtrA stress protein is involved in intramacrophagic replication of adherent and invasive Escherichia coli strain LF82 isolated from a patient with Crohn’s disease. Infect Immun 2005;73:712–721.
Glasser AL, Boudeau J, Barnich N et al. Adherent invasive Escherichia coli strains from patients with Crohn’s disease survive and replicate within macrophages without inducing host cell death. Infect Immun 2001;69:5529–5537.
Chen TC, Tsai JP, Huang HJ et al. Regulation of cyclooxygenase-2 expression in human bladder epithelial cells infected with type I fimbriated uropathogenic E. coli. Cell Microbiol 2011;13:1703–1713.
Brown JR, DuBois RN . COX-2: a molecular target for colorectal cancer prevention. J Clin Oncol 2005;23:2840–2855.
Thi EP, Lambertz U, Reiner NE . Sleeping with the enemy: how intracellular pathogens cope with a macrophage lifestyle. PLoS Pathog 2012;8:e1002551.
Kumar Y, Valdivia RH . Leading a sheltered life: intracellular pathogens and maintenance of vacuolar compartments. Cell Host Microbe 2009;5:593–601.
Stein MP, Muller MP, Wandinger-Ness A . Bacterial pathogens commandeer Rab GTPases to establish intracellular niches. Traffic 2012;13:1565–1588.
Friedrich N, Hagedorn M, Soldati-Favre D et al. Prison break: pathogens’ strategies to egress from host cells. Microbiol Mol Biol Rev 2012;76:707–720.
Fratti RA, Chua J, Deretic V . Induction of p38 mitogen-activated protein kinase reduces early endosome autoantigen 1 (EEA1) recruitment to phagosomal membranes. J Biol Chem 2003;278:46961–46967.
Cavalli V, Vilbois F, Corti M et al. The stress-induced MAP kinase p38 regulates endocytic trafficking via the GDI:Rab5 complex. Mol Cell 2001;7:421–432.
Marjuki H, Gornitzky A, Marathe BM et al. Influenza A virus-induced early activation of ERK and PI3K mediates V-ATPase-dependent intracellular pH change required for fusion. Cell Microbiol 2011;13:587–601.
Webber JL, Tooze SA . Coordinated regulation of autophagy by p38alpha MAPK through mAtg9 and p38IP. EMBO J 2010;29:27–40.
Corcelle E, Djerbi N, Mari M et al. Control of the autophagy maturation step by the MAPK ERK and p38: lessons from environmental carcinogens. Autophagy 2007;3:57–59.
Klug K, Ehlers S, Uhlig S et al. Mitogen-activated protein kinases p38 and ERK1/2 regulated control of Mycobacterium avium replication in primary murine macrophages is independent of tumor necrosis factor-alpha and interleukin-10. Innate Immun 2011;17:470–485.
Dimitrakopoulos O, Liopeta K, Dimitracopoulos G et al. Replication of Brucella melitensis inside primary human monocytes depends on mitogen activated protein kinase signaling. Microbes Infect 2013;15:450–460.
Helaine S, Cheverton AM, Watson KG et al. Internalization of Salmonella by macrophages induces formation of nonreplicating persisters. Science 2014;343:204–208.
Bringer MA, Glasser AL, Tung CH et al. The Crohn’s disease-associated adherent-invasive Escherichia coli strain LF82 replicates in mature phagolysosomes within J774 macrophages. Cell Microbiol 2006;8:471–484.
Moreau K, Lacas-Gervais S, Fujita N et al. Autophagosomes can support Yersinia pseudotuberculosis replication in macrophages. Cell Microbiol 2010;12:1108–1123.
Starr T, Child R, Wehrly TD et al. Selective subversion of autophagy complexes facilitates completion of the Brucella intracellular cycle. Cell Host Microbe 2012;11:33–45.
Kim JM, Lee JY, Yoon YM et al. Bacteroides fragilis enterotoxin induces cyclooxygenase-2 and fluid secretion in intestinal epithelial cells through NF-kappaB activation. Eur J Immunol 2006;36:2446–2456.
Hisatsune J, Yamasaki E, Nakayama M et al. Helicobacter pylori VacA enhances prostaglandin E2 production through induction of cyclooxygenase 2 expression via a p38 mitogen-activated protein kinase/activating transcription factor 2 cascade in AZ-521 cells. Infect Immun 2007;75:4472–4481.
Thomas W, Ascott ZK, Harmey D et al. Cytotoxic necrotizing factor from Escherichia coli induces RhoA-dependent expression of the cyclooxygenase-2 Gene. Infect Immun 2001;69:6839–6845.
Bamba H, Ota S, Kato A et al. High expression of cyclooxygenase-2 in macrophages of human colonic adenoma. Int J Cancer 1999;83:470–475.
Hull MA, Booth JK, Tisbury A et al. Cyclooxygenase 2 is up-regulated and localized to macrophages in the intestine of Min mice. Br J Cancer 1999;79:1399–1405.
Hull MA, Faluyi OO, Ko CW et al. Regulation of stromal cell cyclooxygenase-2 in the ApcMin/+ mouse model of intestinal tumorigenesis. Carcinogenesis 2006;27:382–391.
Hardwick JC, van den Brink GR, Offerhaus GJ et al. NF-kappaB, p38 MAPK and JNK are highly expressed and active in the stroma of human colonic adenomatous polyps. Oncogene 2001;20:819–827.
Chang YJ, Wu MS, Lin JT et al. Induction of cyclooxygenase-2 overexpression in human gastric epithelial cells by Helicobacter pylori involves TLR2/TLR9 and c-Src-dependent nuclear factor-kappaB activation. Mol Pharmacol 2004;66:1465–1477.
Acknowledgements
We thank Professor Maria Belvisi and Dr Mark Birrell (Respiratory Pharmacology, National Heart and Lung Institute, Imperial College, London) for kindly giving TLR4 knockout mice. We thank the ICCF platform for confocal microscopy and the CICS platform for transmission electronic microscopy. This study was supported by the Ministère de l’Enseignement supérieur et de la Recherche, Inserm, and Université d’Auvergne (UMR1071), INRA (USC-2018), and by a grant from Ligue contre le cancer. Jennifer Raisch was supported by the Fondation pour la Recherche Médicale and Anaelle Dubois by the Conseil Régional d’Auvergne.
Special note: This paper is dedicated to the memory of Professor Arlette Darfeuille-Michaud who sadly passed away on 28 June 2014.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
Tumors of patients with colorectal cancer are abnormally colonized by E. coli. In this study, the authors provide evidence showing that tumor-infiltrating bacteria can support tumor progression by persisting within immune cells and inducing production of pro-tumoral factors such as COX-2.
Rights and permissions
About this article
Cite this article
Raisch, J., Rolhion, N., Dubois, A. et al. Intracellular colon cancer-associated Escherichia coli promote protumoral activities of human macrophages by inducing sustained COX-2 expression. Lab Invest 95, 296–307 (2015). https://doi.org/10.1038/labinvest.2014.161
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2014.161
This article is cited by
-
Gut microbiota modulation: a tool for the management of colorectal cancer
Journal of Translational Medicine (2022)
-
E. coli diversity: low in colorectal cancer
BMC Medical Genomics (2020)
-
Microbiota dysbiosis and barrier dysfunction in inflammatory bowel disease and colorectal cancers: exploring a common ground hypothesis
Journal of Biomedical Science (2018)
-
The gut microbiota influences anticancer immunosurveillance and general health
Nature Reviews Clinical Oncology (2018)
-
Barrett's esophagus is associated with a distinct oral microbiome
Clinical and Translational Gastroenterology (2018)