Abstract
Identification and characterization of therapeutic targets for joint conditions, such as osteoarthritis (OA), is exceedingly important for addressing the increasing burden of disease. Transforming growth factor-α (TGFα) is upregulated by articular chondrocytes in experimentally induced and human OA. To test the potential involvement of TGFα, which is an activator of epidermal growth factor receptor (EGFR) signaling, in joint degeneration and to identify signaling mechanisms mediating articular chondrocyte responses to TGFα, rat chondrocytes and osteochondral explants were treated with TGFα and various inhibitors of intracellular signaling pathways. Stimulation of EGFR signaling in articular chondrocytes by TGFα resulted in the activation of RhoA/ROCK (Rho kinase), MEK (MAPK/ERK kinase)/ERK (extracellular-signal-regulated kinase), PI3K (phosphoinositide 3-kinase) and p38 MAPK (mitogen-activated protein kinase) pathways. Modification of the chondrocyte actin cytoskeleton was stimulated by TGFα, but inhibition of only Rho or ROCK activation prevented morphological changes. TGFα suppressed expression of anabolic genes including Sox9, type II collagen and aggrecan, which were rescued only by inhibiting MEK/ERK activation. Furthermore, catabolic factor upregulation by TGFα was prevented by ROCK and p38 MAPK inhibition, including matrix metalloproteinase-13 and tumor necrosis factor-α, which are well known to contribute to cartilage digestion in OA. To assess the ability of TGFα to stimulate degradation of mature articular cartilage, type II collagen and aggrecan cleavage fragments were analyzed in rat osteochondral explants exposed to exogenous TGFα. Normal articular cartilage contained low levels of both cleavage fragments, but high levels were observed in the cartilage treated with TGFα. Selective inhibition of MEK/ERK and Rho/ROCK activation greatly reduced or completely prevented excess type II collagen and aggrecan degradation in response to TGFα. These data suggest that TGFα is a strong stimulator of cartilage degradation and that Rho/ROCK and MEK/ERK signaling have critical roles in mediating these effects.
Similar content being viewed by others
Main
Osteoarthritis (OA) is a chronic, degenerative, synovial joint condition, which affects the knees, hips and other smaller joints of ∼10% of the North American population. The societal burden of OA is increasing and OA already accounts for 25% of visits to primary care physicians and for 50% of nonsteroidal anti-inflammatory drug prescriptions.1, 2 Approximately 80% of individuals have radiographic evidence of OA by age 65 years, of which 60% are symptomatic.1 Furthermore, progressive joint degeneration combined with an inherently low capacity for articular cartilage regeneration makes treatment very difficult. As current therapies are strictly palliative, identification and characterization of therapeutic targets is exceedingly important to meet the increasing burden of disease.
Although important differences exist between primary and secondary types of OA, articular cartilage degeneration is common to all forms. Despite increasing research in this field, molecular interactions leading to the development of OA are not completely understood. Although cartilage degradation is caused by enhanced extracellular matrix (ECM) digestion by proteases (eg, matrix metalloproteinase-13; MMP-13) and insufficient ECM synthesis,3 etiology is influenced by many factors, including age, obesity, history of trauma and family history, among others.4, 5 Therefore, a greater understanding of the pathogenic molecular interactions is required to design therapies for early intervention and for preventing progression.
We discovered recently that transforming growth factor-α (TGFα) is upregulated by articular chondrocytes in a rat model of joint destabilization-induced OA;6, 7 it was also increased in a subset of human OA samples.8 TGFα is a member of the epidermal growth factor (EGF) family of ligands and is well characterized for its roles in inflammatory responses to infection, epithelial maintenance and malignancies.9, 10, 11 Our further investigations determined that TGFα inhibits anabolic and promotes catabolic processes in articular cartilage.8 Thus, interference with TGFα signaling in chondrocytes represents a potential therapeutic strategy for OA.
TGFα signaling is mediated by binding to the epidermal growth factor receptor (EGFR), which is a receptor tyrosine kinase.9 It has been known for several years that TGFα levels are increased in the synovium and synovial fluid of patients with OA or rheumatoid arthritis (RA).12, 13 Therefore, our discovery that TGFα is produced by articular chondrocytes represents an additional source of TGFα production in OA. Furthermore, recent evidence in mice has shown that a constitutive activation of EGFR signaling leads to OA pathogenesis.14 Thus, strong molecular evidence points to a role had by TGFα in OA and, potentially, additional arthropathies.
As a therapeutic strategy, specific inhibition of TGFα binding to the EGFR would require a biological approach to sequester the ligand (eg, similar to TNFα inhibition with adalimumab, etc. in RA), but none exists at present. Another approach, blockade of EGFR activation, is widely known to have strong side effects associated with cell turnover interference (eg, epithelial maintenance), presenting additional challenges. Alternatively, interruption of intracellular signaling downstream of EGFR activation may be a viable strategy. However, the intracellular mechanisms mediating the differential sequelae of TGFα signaling in chondrocytes have not been elucidated.
It is known that Rho/ROCK (Rho kinase) signaling regulates actin cytoskeletal dynamics in chondrocytes,15, 16, 17 whereas MEK (MAPK/ERK kinase)/ERK (extracellular-signal-regulated kinase) signaling alters chondrocyte maturation and phenotype during chondrogenesis.18 Furthermore, MEK/ERK and p38 MAPK (mitogen-activated protein kinase) signaling are implicated in the degenerative processes in articular cartilage.19, 20 Therefore, we hypothesized that these pathways also mediate TGFα signaling in articular chondrocytes and the induction of cartilage degradation. The results of our study show that TGFα activates several intracellular pathways including RhoA/ROCK and MEK/ERK and that each pathway mediates specific aspects of the cartilage response to TGFα.
MATERIALS and METHODS
Reagents
Cell and tissue culture media reagents were purchased from Invitrogen (Burlington, ON, Canada) or Sigma (Oakville, ON, Canada). Pharmacological inhibitors were purchased from Calbiochem (VWR CANLAB, Mississauga, ON, Canada).
Primary Chondrocyte and Osteochondral Explant Culture
Primary epiphyseal chondrocytes were isolated from the distal femoral condyles of 1-day-old Sprague–Dawley rats.21 Cells were plated at a density of 4.5 × 104 cells per cm2 on tissue culture-coated multi-well plates (BD Falcon, Mississauga, ON, Canada) in 2:3 DMEM:F12 culture medium with 10% fetal bovine serum, supplemented with 50 μg/ml ascorbic acid, 0.25% L-glutamine and 0.25% penicillin/streptomycin for 48 h. Media was replaced with serum-free media 24 h before the treatment. Treatment was carried out for 48 h in the serum-free media plus 0.1% DMSO vehicle (control) or 10 ng/ml recombinant human TGFα (Biosource—Medicorp, Montréal, QC, Canada) in the presence or absence of 10 μM pharmacological inhibitor of ROCK (Y27632), MEK1/2 (U0126), PI3K (LY294002), or p38 MAPK (SB202190) or 1 μg/ml cell-permeable toxin C3 Rho inhibitor (Cytoskeleton, Denver, CO, USA).
Full joint-width osteochondral explants of distal femoral condyle and proximal tibial plateau articular cartilages were excised from 4–5-month-old male Sprague–Dawley rat knees using a high-speed rotary tool under sterile saline irrigation. Explants were equilibrated for 24 h in α-MEM organ culture medium supplemented with 50 μg/ml ascorbic acid, 0.25% L-glutamine and 0.25% penicillin/streptomycin and then transferred into fresh plates with media plus vehicle or 10 ng/ml TGFα in the presence or absence of inhibitors as described above. Treatment was carried out for 5 days with media changes at 2 and 4 days (+/− treatments as described above). Cell and explant cultures were maintained at 37 °C in a humidified environment with 5% CO2. The use of animals for these purposes was approved by the Animal Care and Use Committee of the University of Western Ontario.
RhoA G-LISA Assay
A RhoA G-LISA assay (Cytoskeleton) was used to assess levels of guanosine tri-phosphate (GTP)- bound RhoA in primary chondrocytes grown to 60% confluence in monolayer, serum-starved for 24 h and treated with 0.1% DMSO vehicle (control) or 10 ng/ml TGFα. Protein was isolated in lysis buffer (provided by the manufacturer) without treatment and after 2, 4, 8, 15 and 30 min of treatment, cells were processed immediately on ice. Lysates were clarified by centrifugation at 10 000 r.p.m. at 4 °C for 2 min. Protein concentration was equalized in all samples to 2 mg/ml before luminescent detection of GTP-bound RhoA levels.
Histological and Immunohistochemical Analyses
Osteochondral explants were fixed for 3 h in 4% paraformaldehyde (PFA) at 4 °C, decalcified and processed for histology, embedded in paraffin and sectioned in the coronal plane. All processing and sectioning was carried out at the Robarts Research Institute Molecular Pathology Laboratory at the University of Western Ontario. Immunohistochemistry (IHC) was performed on tissue sections with rabbit anti-phospho-LIM-kinase1/2 (LIMK1/2), rabbit anti-phospho-myosin light chain 2 (MLC2) (Cell Signaling Technology, Pickering, ON, Canada), goat anti-SOX9 (R&D Systems, Minneapolis, MN, USA), rabbit anti-VDIPEN (MMP-generated aggrecan cleavage fragment) or rabbit anti-COL2-3/4C (MMP-13-generated type II collagen cleavage fragment) antibodies.22, 23 Secondary antibodies included goat anti-rabbit IgG and rabbit anti-goat IgG antibodies conjugated to horseradish peroxidase (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Colorimetric detection with diaminobenzidine substrate (Dako, Carpinteria, CA, USA) was carried out for equal time periods, followed by Harris’ hematoxylin counterstaining. Additional sections were stained with 0.1% safranin-O, 0.02% fast green and Harris’ hematoxylin.
Cytoskeletal Staining and Imaging
Primary chondrocyte cultures (N=3 independent isolations) were plated on glass coverslips and cultured as described above. Cells were fixed with 4% PFA for 10 min at room temperature, washed with PBS, permeabilized with 0.05% Triton X-100/PBS and stained with phalloidin–rhodamine (Cytoskeleton). Nuclei were counterstained with Toto-3 iodide (Molecular Probes, Burlington, ON, Canada) and coverslips were mounted with Vectashield (Vector Laboratories, Burlingame, CA, USA). Images were acquired using a Zeiss LSM510 META confocal microscope and Axiovision LE image processing software (Carl Zeiss, Toronto, ON, Canada).
Protein Isolation and Western Blotting
Protein was extracted from primary chondrocyte cultures (N=3 independent isolations) in 300 μl RIPA buffer (150 mM NaCl, 50 mM Tris-HCl, pH 7.5, 1% deoxycholate, 0.1% SDS, 1% Triton X-100) supplemented with protease and phosphatase inhibitor tablets (Roche Diagnostics, Indianapolis, IN, USA). Cell lysates were sonicated on ice; protein concentration was determined by bicinchoninic acid assay (Sigma). 10% SDS-polyacrylamide gel electrophoresis was performed under reducing conditions, blotted to nitrocellulose membrane and blocked with Odyssey Blocking Reagent (LI-COR Biosciences, Lincoln, NB, USA). Overnight co-incubation at 4 °C with mouse and rabbit primary antibodies to phosphorylated and total LIMK1/2, MLC2, ERK1/2, AKT or p38 MAPK (Cell Signaling Technology and Santa Cruz Biotechnology) and α-actin (Sigma) was carried out. Co-incubation with goat anti-mouse and goat anti-rabbit secondary antibodies conjugated to 680CW and 800CW IRDye infrared detectors (LI-COR Biosciences) was then performed at room temperature for 1 h. Infrared fluorescence detection and quantification was performed using the Odyssey Infrared Imaging System (LI-COR Biosciences).
RNA Isolation and Real-Time PCR Analyses
Total RNA was isolated from primary cultures using a Qiagen RNeasy Mini Kit (Qiagen, Mississauga, ON, Canada) according to the manufacturer's protocols. Real-time PCR analysis was performed using the Applied Biosystems 7900HT Real-Time PCR System, Eurogentec One-Step RT qPCR MasterMix reagents (Eurogentec, San Diego, CA, USA) and TaqMan Gene Expression Assays (Applied Biosystems, Foster City, CA, USA). Each gene was assessed relative to Gapdh expression using the ΔΔCT method.
Luciferase SOX9 Reporter Gene Assay
Primary cultures were transiently transfected with a plasmid containing 4 × 48 bp SOX9-binding region repeats from the Col2a1 gene as described previously using FuGENE 6 transfection reagent (Roche).24, 25 Each transfection reaction contained 0.25 μg SOX9 reporter plasmid containing the firefly luciferase gene and 0.5 μg control plasmid containing the Renilla luciferase gene (CMV promoter). Cultures were harvested in lysis buffer and luminescence from firefly luciferase was quantified relative to Renilla luciferase using the Dual Luciferase Reporter Assay System (Promega, Madison, WI, USA).
Measurement of Chondrocyte Cell Numbers
Primary chondrocyte culture cell number was analyzed using a Cell Proliferation Kit I (MTT) (Roche Diagnostics, Laval, QC, Canada) according to the manufacturer's protocol as described previously.8 A microplate reader (Tecan US, Durham, NC, USA) was used to quantify the colorimetric reaction by 600 nm absorbance readings.
Statistical Analyses
All data were analyzed by one- or two-way analysis of variance with Tukey's or Bonferroni's post hoc test, respectively, using GraphPad Prism 4.0 software (GraphPad Software, San Diego, CA, USA). P<0.05 was considered statistically significant.
RESULTS
Activation of RhoA/ROCK Signaling by TGFα
We have previously shown that TGFα stimulates stress fiber formation in chondrocytes,8 a phenotype consistent with activation of the RhoA pathway.15 Therefore, we assessed RhoA activity in primary chondrocyte cultures to determine the ability of TGFα signaling (through EGFR) to activate the RhoA/ROCK pathway. In primary chondrocytes, levels of GTP-bound (activated) RhoA were significantly increased after 4 min of stimulation with TGFα compared with controls (Figure 1a). Activated RhoA levels remained significantly elevated after 30 min of treatment. Additional Rho family members (eg, RhoB, RhoC) were not assessed.
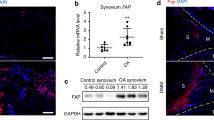
Rho/ROCK pathway activation and morphology. (a) Chondrocytes were cultured with vehicle (control) or 10 ng/ml TGFα for up to 30 min. RhoA G-LISA assay was used to assess levels of GTP-bound RhoA. Mean (N=4 independent isolations) relative light units (RLU) (plus s.d.) are shown. Significantly different means (P<0.05) compared with controls are indicated by asterisks. (b) Protein was isolated from chondrocyte cultures cultured for 15 or 30 min with vehicle only (control) or with 10 ng/ml TGFα. Levels of phosphorylated LIM kinase (phLIMK1/2) and myosin light chain (phMLC2) were assessed relative to total LIMK1/2, MLC2 and β-actin levels by Western blot. (c) Immunostaining for phLIMK1/2 and phMLC2 (brown) and hematoxylin counterstaining of tissue sections from explant cultures incubated for 5 days with or without (control) 10 ng/ml TGFα. Scale bar represents 50 μm. (d) Chondrocytes were cultured with vehicle (DMSO) or 10 ng/ml TGFα for 48 h in the presence or absence of 10 μM ROCK (Y27632), 1 μg/ml RhoA (C3) or 10 μM MEK1/2 (U0126) inhibitor. Cells were fixed and stained with phalloidin–rhodamine for actin (red signal) and Toto-3 iodide for nuclei (green signal) and imaged by confocal microscopy. Scale bar represents 20 μm.
As RhoA activation leads to phosphorylation of effector molecules such as MLC2 and LIMK1/2 by ROCK/Rho-kinase family members,26, 27 we next assessed these downstream targets by western blot and IHC. Phospho-specific antibodies were used to detect levels of phMLC2 and phLIMK1/2 in cell culture protein isolations and in explant culture sections. In TGFα-treated chondrocytes, higher levels of phMLC2 and phLIMK1/2 were seen after 15 and 30 min, respectively, compared with controls (vehicle-only) (Figure 1b). In situ, both phospho targets were increased in mid-zone articular chondrocytes after 5 days of treatment with TGFα relative to controls (Figure 1c). Respectively, these data show immediate and sustained RhoA/ROCK effector activation after stimulation with TGFα in monolayer and in the three-dimensional context of intact articular cartilage.
As Rho/ROCK signaling mediates cytoskeletal rearrangements in chondrocytes,15 we tested cytoskeletal responses in primary chondrocyte cultures in the presence and absence of a Rho (C3 toxin) or ROCK (Y27632) inhibitor. In positive control (vehicle-only) cultures, TGFα induced stress fiber formation as described previously.8 However, cytoskeletal rearrangements and stress fiber formation in response to TGFα were prevented in chondrocytes treated with C3 or Y27632 (Figure 1d), indicating that Rho and ROCK activation is required for these morphological changes. In contrast, inhibition of MEK/ERK activation with the MEK-specific inhibitor U0126 did not prevent cytoskeletal changes induced by TGFα (Figure 1d), demonstrating specific control of chondrocyte shape through Rho/ROCK activation.
Differential Intracellular Signaling Pathway Activation by TGFα
To investigate the extent to which additional pathways are activated by TGFα in chondrocytes, we carried out western blot analysis of chondrocyte protein lysates using antibodies to detect the total and phosphorylated forms of ERK1/2 (MEK/ERK pathway), p38 MAPK and AKT (PI3K pathway) kinases. Higher levels of phosphorylated ERK1/2, p38 MAPK and AKT were seen after stimulation with TGFα compared with untreated controls (Figure 2a). Infrared fluorescent signal quantification determined that levels of phospho-ERK1/2 and phospho-AKT (normalized to total levels) were significantly elevated after 5, 15 and 30 min of stimulation, whereas phospho-p38 MAPK was significantly increased only up to 15 min (not shown).
Activation of multiple signaling pathways and effects on ECM genes and Sox9. (a) Protein was isolated from chondrocyte cultures cultured for up to 30 min with vehicle (control) or 10 ng/ml TGFα. Levels of phosphorylated (ph-) ERK1/2, p38 MAPK and AKT were assessed relative to total ERK1/2, p38 MAPK or AKT levels, respectively, by western blot. (b) Real-time PCR was performed using RNA samples isolated from chondrocytes incubated with vehicle (control) or 10 ng/ml TGFα for 48 h in the presence or absence of 10 μM ROCK (Y27632), MEK (U0126), p38 MAPK (SB202190) or PI3K (LY294002) inhibitor. Mean gene expression values (plus s.d.) for type II collagen (Col2a1), aggrecan (Agc1) and Sox9 from N=4 independent cell isolations are shown normalized to controls. (c) Immunostaining for SOX9 (brown) and hematoxylin counterstaining of tissue sections from explant cultures incubated for 5 days with or without (control) 10 ng/ml TGFα in the presence or absence of 10 μM MEK inhibitor (U0126). Scale bar represents 100 μm. (d) Chondrocytes were transfected with a reporter vector for SOX9 activity and cultured for 48 h with vehicle (control) or TGFα in the presence or absence of an MEK inhibitor. Mean relative light units (RLU) (plus s.d.) from N=4 independent cell isolations, normalized to untreated controls are shown. Significantly different (P<0.05) means (compared with controls) are indicated by asterisks.
ECM Gene Regulation Through MEK/ERK Signaling
TGFα signaling in chondrocytes inhibits ECM gene expression through the suppression of SOX9,8 a critical transcriptional regulator of type II collagen and aggrecan in chondrocytes.28, 29 Thus, we assessed the contribution of the Rho/ROCK, MEK/ERK, PI3K and p38 MAPK pathways to the control of Sox9 and ECM gene expression by TGFα signaling. Inhibition of MEK/ERK activation was achieved with the MEK inhibitor, U0126, and that of PI3K signaling inhibition with the AKT inhibitor, LY294002. Real-time PCR showed that type II collagen (Col2a1) and aggrecan (Agc1) mRNA downregulation in response to TGFα could only be rescued by inhibition of MEK/ERK (Figure 2b). Correlating with these MEK/ERK-dependent reductions in ECM gene expression, the suppression of Sox9 mRNA expression could also be rescued by MEK/ERK inhibition, but not with other compounds (Figure 2b). Finally, MEK/ERK inhibition resulted in the rescue of SOX9 protein expression in TGFα-treated explant cultures (Figure 2c) and SOX9 activity in luciferase reporter gene assay (Figure 2d), validating these results at protein and functional levels.
Complex Control of Proliferation and Catabolic Genes
As TGFα induces mitogenic activity and MMP-13 production, as well as drives inflammatory cytokine gene expression (eg, Tnfa, encoding TNFα) in chondrocytes,8 we explored how these responses are controlled by intracellular signaling pathways. As expected, TGFα induced a significant increase in chondrocyte number after 48 h (Figure 3a). Inhibition of each pathway tested (MEK/ERK, Rho/ROCK, p38 MAPK or PI3K) prevented the increase in cell number and significantly reduced chondrocyte numbers relative to vehicle-only controls (Figure 3a); statistics for the latter are not shown for simplicity.
Effects of different pathways on cell number, Mmp13 and Tnfa expression. (a) MTT analysis was performed by spectrophotometry of chondrocytes cultured with vehicle (control) or 10 ng/ml TGFα in the presence or absence (vehicle) of 10 μM ROCK (Y27632), MEK (U0126), p38 MAPK (SB202190) or PI3K (LY294002) inhibitor. The mean absorbance readings (plus s.d.) from N=5 independent cell isolations are shown. Significant reductions compared with vehicle only occurred in all inhibitor-treated samples +/−TGFα (statistics not shown for simplicity). (b) Real-time PCR was performed using RNA samples isolated from chondrocytes incubated with vehicle (control) or 10 ng/ml TGFα for 48 h in the presence or absence of 10 μM inhibitors as described above. Mean gene expression values (plus s.d.) for matrix metalloproteinase-13 (Mmp13) and (c) tumor necrosis factor-α (Tnfa) from N=4 independent cell isolations are shown normalized to controls. Significantly different (P<0.05) TGFα-treated vs control means are indicated by asterisks.
Real-time PCR analyses of RNA from primary cultures determined that upregulation of Mmp13 could not be rescued by inhibiting any of the pathways investigated (Figure 3b). Conversely, blockade of Rho/ROCK or PI3K signaling dramatically enhanced Mmp13 upregulation in the presence of TGFα (Figure 3b). Although MEK/ERK and PI3K inhibition resulted in the abrogation of basal Tnfa expression below detectable levels (without TGFα treatment), neither could prevent Tnfa induction by TGFα (Figure 3c). In contrast, Rho/ROCK and p38 MAPK inhibitors both prevented Tnfa upregulation (Figure 3c). In parallel experiments, TGFα did not induce the expression of IL-1β mRNA in chondrocytes (not shown).
Degradation of Articular Cartilage ECM Stimulated by TGFα
We next analyzed cartilage explant tissues for histomorphological changes. Chondrocyte clusters (suggestive of chondrocyte division) were induced by TGFα treatment alone, as reported previously.8 Each inhibitor tested seemed to suppress this increase in clusters (arrowhead, Figure 4), supporting our assessments of cell number. Interestingly, ROCK inhibition promotes hypertrophy of growth plate chondrocytes in part by suppressing cell division,17 suggesting that similar treatment may induce hypertrophy of articular chondrocytes. However, mRNA expression of several hypertrophic markers including alkaline phosphatase (Alp1), bone morphogenetic protein 6 (Bmp6), runt-related transcription factor 2 (Runx2) and bone sialoprotein (Ibsp—undetectable, not shown) was suppressed by TGFα in primary chondrocytes (Figure 5). Production of type X collagen assessed by immunostaining in articular cartilage explants was also unchanged in the presence of TGFα, with or without the ROCK inhibitor (data not shown).
Histology and immunostaining for aggrecan and type II collagen cleavage fragments. Osteochondral explants were cultured for 5 days with vehicle (control) or 10 ng/ml TGFα in the presence or absence of a ROCK (Y27632), MEK (U0126), p38 MAPK (SB202190) or PI3K (LY294002) inhibitor (10 μM). Tissue sections were stained with safranin-O/fast green or immunostained for MMP-generated aggrecan or type II collagen cleavage fragments (brown stain). All sections were counterstained with hematoxylin. Arrowhead indicates chondrocyte cluster. Scale bars represent 50 μm.
Hypertrophic marker gene expression in articular chondrocytes. Real-time PCR was performed using RNA samples isolated from chondrocytes incubated with vehicle (control) or 10 ng/ml TGFα for 48 h in the presence or absence of the ROCK inhibitor (Y27632). Mean gene expression values (plus s.d.) for alkaline phosphatase (Alp1), bone morphogenetic protein 6 (Bmp6) and runt-related transcription factor 2 (Runx2) relative to Gapdh from N=4 independent cell isolations are shown normalized to control (untreated) levels. Asterisks indicate significantly different (P<0.05) means compared with controls.
To assess induction of cartilage degradation, immunostaining for cartilage degradation markers was performed using antibodies against MMP-generated aggrecan (CGGVDIPEN) and type II collagen (COL2-3/4C) cleavage fragments.23, 30 Striking increases in aggrecan and type II collagen cleavage fragment staining were observed in superficial and mid-zone chondrons after 5 days of treatment with TGFα compared with untreated controls (Figure 4). The use of ROCK and MEK inhibitors alone reduced basal levels of aggrecan and type II collagen fragments and prevented increases in aggrecan and type II collagen fragments in the presence of TGFα (Figure 4). PI3K and p38 MAPK inhibition did not reduce basal aggrecan fragment but did reduce basal type II collagen fragment levels (Figure 4). In the presence of TGFα, PI3K and p38 MAPK inhibition was unable to reduce aggrecan cleavage and only slightly reduced type II collagen cleavage (Figure 4).
DISCUSSION
We have previously reported that TGFα upregulation by knee articular chondrocytes is an early event in a rat model of joint destabilization-induced knee OA and that TGFα is elevated in late-stage human knee OA chondrocytes.8 Although it was further determined that TGFα induces chondrocyte phenotype modification, the intracellular mechanisms mediating the suppression of anabolic and activation of catabolic processes remained unclear. The results of this study show that RhoA/ROCK, MEK/ERK, p38 MAPK and PI3K/AKT signaling pathways are activated by the stimulation of articular chondrocytes with TGFα. Moreover, Rho/ROCK and MEK/ERK signaling mediate deleterious outcomes after TGFα stimulation (Figure 6). We also showed that chondrocyte exposure to TGFα results in strong increases in MMP-mediated collagen and proteoglycan digestion within mature articular cartilage. Thus, TGFα seems to be a powerful stimulator of articular cartilage degradation and a modifier of chondrocyte phenotype. Given its temporal increase during cartilage degradation, TGFα is likely to be an important driver in the pathogenesis of joint conditions, such as OA.
Working model of TGFα signaling mechanisms and outcomes. TGFα upregulation is stimulated in osteoarthritic cartilage leading to the activation of multiple signaling pathways including Rho/ROCK and MEK/ERK and increased expression of TNFα. Each pathway mediates multiple outcomes as illustrated. The color reproduction of this figure is available on the html full text version of the manuscript.
It is well established that the phenotypic stability of articular chondrocytes is critical and that modifications to chondrocyte shape (eg, flattening, elongation, hypertrophy) impede the normal functions of the chondrocyte.31, 32 Interestingly, changes in chondrocyte shape are commonly observed in OA.33 Our study shows, for the first time, that Rho/ROCK signaling is activated by TGFα in chondrocytes; this in turn induces elongation of chondrocyte shape and stress fiber formation, most likely through activation of the LIM kinase.27 As MEK/ERK inhibition was unable to prevent stress fiber formation, this suggests that the involvement of Rho/ROCK signaling in this process is specific and direct. The possibility that Rho family members act downstream of EGFR signaling has only recently been suggested.34 Although RhoA activation after EGFR stimulation with heparin binding EGF-like growth factor has been reported,35 this is the first report showing Rho/ROCK activation by TGFα. Interestingly, a crosstalk between Ras-mediated and Rho/ROCK pathways results in Rho/ROCK/LIMK inhibition in other cell types in a MEK-dependent manner.36, 37 In contrast, our studies indicate that TGFα induces Rho/ROCK/LIMK activation in chondrocytes concomitantly with the activation of multiple Ras-mediated pathways (eg, Ras-MEK/ERK and Ras-PI3K). In addition, we observed simultaneous MLC2 activation by TGFα, suggesting that contractility may be induced in articular chondrocytes by EGFR activation.38 Although stress fiber formation and contractility is normal in some cell types such as fibroblasts,39 these events represent unfavorable modification of the articular chondrocyte phenotype through activation of Rho/ROCK signaling. Furthermore, these data suggest that inhibition of Rho/ROCK signaling would favor articular cartilage maintenance and repair.
TGFα elicits a mitogenic response in chondrocytes and other cell types.8, 40 Although this observation indicates an opportunity to increase the number of chondrocytes available for cartilage regeneration (eg, for tissue engineering strategies), such an approach would require that maintenance of the chondrocyte phenotype could be achieved. However, in addition to severe phenotypic modulation, chondrocytes exhibit reduced expression of anabolic genes and elevated Mmp13 and Tnfa expression when stimulated with TGFα. Therefore, additional chondrocytes generated by TGFα-stimulated mitogenesis would be unlikely to regenerate damaged articular cartilage. Moreover, as concerted activation of all pathways studied herein is necessary to elicit a mitogenic response to TGFα, attempts to block deleterious effects mediated by the Rho/ROCK and MEK/ERK pathways would also prevent induction of chondrocyte division and negate the possibility of generating additional chondrocytes.
Hypertrophy of articular chondrocytes in OA is believed to contribute to OA pathogenesis,41 despite being a normal developmental process in growth plate chondrocytes. Interestingly, blocking Rho/ROCK signaling suppresses proliferation and induces MMP-13 expression in growth plate chondrocytes,17 similar to articular chondrocytes studied herein. However, although Rho/ROCK inhibition promotes chondrocyte hypertrophy in the growth plate, none of the hypertrophic markers assessed were elevated by chondrocytes exposed to TGFα and a ROCK inhibitor. As articular chondrocytes are arrested in a non-hypertrophic state,42 an additional stimulus may be required to ‘switch on’ articular chondrocytes and resume the developmental program to hypertrophy. We therefore conclude that exposure to TGFα does not promote hypertrophy of articular chondrocytes, even in the presence of a ROCK inhibitor.
Nevertheless, it is clear that attempts to strategically modulate Rho/ROCK or MEK/ERK signaling could be complicated by mixed outcomes. For example, MEK/ERK inhibition restores ECM gene expression, but fewer chondrocytes are generated, and Tnfa expression remains elevated. Similarly, inhibition of Rho/ROCK signaling blocks Tnfa expression and prevents phenotype modification, but induces Mmp13.
Evidence for activation of multiple intracellular pathways by EGFR signaling has accumulated for many cell types other than chondrocytes.43, 44 Not surprisingly then, we observed that EGFR stimulation with TGFα results in the activation of MEK/ERK, PI3K/AKT and p38 MAPK pathways contemporaneously with Rho/ROCK. Activation of these pathways likely influences articular chondrocyte physiology as in cartilage development. For example, Rho/ROCK signaling modified chondrocyte shape in this study and induced chondrocyte phenotype changes during chondrogenesis.15, 16, 17, 45 Similarly, MEK/ERK signaling led to the suppression of chondrocyte differentiation46 and caused suppression of ECM gene expression and SOX9 levels in our experiments with articular chondrocytes. These findings are further supported by Yagi et al,47 who showed that suppression of MEK/ERK signaling by Bcl-2 increases SOX9 expression in chondrocytes. TGFα is upregulated by OA chondrocytes, our findings indicate that MEK/ERK activation by TGFα reduces anabolic activity and thereby the capacity to replace damaged and eroded articular cartilage. Interestingly, IGF-1 maintains proteoglycan production in chondrocytes through a PI3K-dependent mechanism, whereas MEK/ERK activation reduces chondrocyte responsiveness to IGF-1 by inhibiting the activation of PI3K.48 Thus, TGFα may suppress aggrecan production by blunting PI3K responses in chondrocytes through the MEK/ERK activation. Taken together, data from our group and from others therefore strongly suggest that inhibition of MEK/ERK activation factors is a key step in the prevention of cartilage degradation.
We also show in this study that TGFα stimulates the cleavage of aggrecan and type II collagen by MMPs, indicating that MMP activity is increased by the activation of the EGFR. Interestingly, type II collagen cleavage fragment staining pattern was similar to that of MMP-13 expression induced by TGFα,8 whereas MMP-13 is known to stimulate type II collagen digestion in the OA cartilage.23, 49 Strikingly, degradation of type II collagen and aggrecan was reduced when MEK/ERK and Rho/ROCK inhibitors were used in the presence of TGFα, although Mmp13 mRNA induction was not suppressed. Therefore, despite the fact that Mmp13 transcript levels remain increased when Rho/ROCK or MEK/ERK signaling is blocked, MMP-13 activity is reduced. Rho/ROCK and MEK/ERK signaling inhibition may therefore prevent MMP-13 activation at the post-transcriptional level. Furthermore, as TNFα induces MMP-13 activity50 and as blocking Rho/ROCK and MEK/ERK prevented Tnfa induction/reduced basal Tnfa expression respectively, enhanced TNFα production may be a driver of ECM digestion induced by TGFα.
Taken together, our observations suggest that blockade of Rho/ROCK and MEK/ERK signaling effectively reduces ECM damage in the cartilage exposed to TGFα. Whereas inhibition of Rho/ROCK activation by TGFα prevents changes in chondrocyte shape, MEK/ERK signaling inhibition rescues the suppression of ECM gene expression and SOX9. Our results align with previous studies that have described roles for MEK/ERK signaling in articular cartilage degeneration19, 20, 48 and point to a similar role for Rho/ROCK. This report also adds to the growing body of evidence indicating that inappropriate activation of the EGFR leads to cartilage degradation.8, 14, 51 It is important to note that additional pathways are stimulated by EGFR activation with TGFα and that these pathways may confer protective benefits. For example, as PI3K signaling is required for proteoglycan production in response to IGF-1 but is suppressed by MEK/ERK signaling,48 PI3K activation by TGFα may be enhanced to stimulate anabolic responses when MEK/ERK activation is blocked. Therefore, as an alternative strategy to block EGFR activation itself or sequestration of TGFα, we have shown the efficacy of interfering with TGFα signaling downstream of the EGFR to reduce cartilage degeneration, as is the case for MEK/ERK and Rho/ROCK inhibition. Although a therapeutic approach involving systemic inhibition of these essential intracellular signaling pathways would not be viable, local inhibitor delivery may be effective for bypassing systemic side effects. However, as repeated intra-articular injection is not preferred as a method of long-term local delivery, development of alternative approaches such as viral-based gene knockdown strategies may be required.
In summary, this study advances our understanding of the mechanisms controlling the metabolic outcomes of TGFα signaling in articular cartilage. We conclude that modulation of the signaling pathways downstream of the EGFR, at least when activated by TGFα, is a compelling strategy for the treatment of joint conditions, such as OA.
References
Green GA . Understanding NSAIDs: from aspirin to COX-2. Clin Cornerstone 2001;3:50–60.
Kopec JA, Rahman MM, Berthelot JM, et al. Descriptive epidemiology of osteoarthritis in British Columbia, Canada. J Rheumatol 2007;34:386–393.
Abramson SB, Attur MG, Yasici Y . Prospects for disease modification in osteoarthritis. Nat Clin Pract Rheumatol 2006;2:304–312.
Aigner T . Osteoarthritis. Curr Opin Rheumatol 2007;19:427–428.
Goldring MB, Goldring SR . Osteoarthritis. J Cell Physiol 2007;213:626–634.
Appleton CTG, McErlain D, Pitelka V, et al. Forced mobilization accelerates pathogenesis: characterization of a pre-clinical surgical model of osteoarthritis. Arthritis Res Ther 2007;9:R13.
Appleton CTG, Pitelka V, Henry JL, et al. Global analyses of gene expression in early experimental osteoarthritis. Arthritis Rheum 2007;56:1854–1868.
Appleton CT, Usmani SE, Bernier SM, et al. Transforming growth factor alpha suppression of articular chondrocyte phenotype and Sox9 expression in a rat model of osteoarthritis. Arthritis Rheum 2007;56:3693–3705.
Brachmann R, Lindquist PB, Nagashima M, et al. Transmembrane TGF-alpha precursors activate EGF/TGF-alpha receptors. Cell 1989;56:691–700.
Groenen LC, Nice EC, Burgess AW . Structure-function relationships for the EGF/TGF-alpha family of mitogens. Growth Factors 1994;11:235–257.
Macleod K, Mullen P, Sewell J, et al. Altered ErbB receptor signaling and gene expression in cisplatin-resistant ovarian cancer. Cancer Res 2005;65:6789–6800.
Hallbeck AL, Walz TM, Briheim K, et al. TGF-alpha and ErbB2 production in synovial joint tissue: increased expression in arthritic joints. Scand J Immunol 2005;34:204–211.
Ritchlin C, Dwyer E, Bucala R, et al. Sustained and distinctive patterns of gene activation in synovial fibroblasts and whole synovial tissue obtained from inflammatory synovitis. Scand J Immunol 1994;40:292–298.
Zhang Y-W, Su Y, Lanning N, et al. Targeted disruption of Mig-6 in the mouse genome leads to early onset degenerative joint disease. Proc Natl Acad Sci USA 2005;102:11740–11745.
Woods A, Wang G, Beier F . RhoA/ROCK signaling regulates Sox9 expression and actin organization during chondrogenesis. J Biol Chem 2005;280:11626–11634.
Woods A, Beier F . RhoA/ROCK signaling regulates chondrogenesis in a context-dependent manner. J Biol Chem 2006;281:13134–13140.
Wang G, Woods A, Sabari S, et al. RhoA/ROCK signaling suppresses hypertrophic chondrocyte differentiation. J Biol Chem 2004;279:13205–13214.
Bobick BE, Kulyk WM . The MEK-ERK signaling pathway is a negative regulator of cartilage-specific gene expression in embryonic limb mesenchyme. J Biol Chem 2004;279:4588–4595.
Fan Z, Bau B, Yang H, et al. IL-1 beta induction of IL-6 and LIF in normal articular human chondrocytes involves the ERK, p38 and NF-kappa B signaling pathways. Cytokine 2004;28:17–24.
Fan Z, Soder S, Oehler S, et al. Activation of interleukin-1 signaling cascades in normal and osteoarthritic articular cartilage. Am J Pathol 2007;171:938–946.
Séguin CA, Bernier SM . TNF-alpha suppresses link protein and type II collagen expression in chondrocytes: role of MEK1/2 and NF-kappa B signaling pathways. J Cell Physiol 2003;197:356–369.
Sztrolovics R, Alini M, Roughley PJ, et al. Aggrecan degradation in human intervertebral disc and articular cartilage. Biochem J 1997;326:235–241.
Billinghurst RC, Dahlberg L, Ionescu M, et al. Enhanced cleavage of type II collagen by collagenases in osteoarthritic articular cartilage. J Clin Invest 1997;99:1534–1545.
Weston AD, Chandraratna RAS, Torchia J, et al. Requirement for RAR-mediated gene repression in skeletal progenitor differentiation. J Cell Biol 2002;158:39–51.
James C, Woods A, Underhill TM, et al. The transcription factor ATF3 is upregulated during chondrocyte differentiation and represses cyclin D1 and A gene transcription. BMC Mol Biol 2006;7:30.
Yamashiro S, Totsukawa G, Yamakita Y, et al. Citron kinase, a Rho-dependent kinase, induces Di-phosphorylation of regulatory light chain of myosin II. Mol Biol Cell 2003;14:1745–1756.
Maekawa M, Ishizaki T, Boku S, et al. Signaling from Rho to the actin cytoskeleton through protein kinases ROCK and LIM-kinase. Science 1999;285:895–898.
Lefebvre V, Behringer RR, de Crombrugghe B . L-Sox5, Sox6 and Sox9 control essential steps of the chondrocyte differentiation pathway. Osteoarthr Cartil 2001;9:S69–S75.
Lefebvre V, Huang W, Harley VR, et al. SOX9 is a potent activator of the chondrocyte-specific enhancer of the pro alpha1(II) collagen gene. Mol Cell Biol 1997;17:2336–2346.
Hughes C, Caterson B, Fosang A, et al. Monoclonal antibodies that specifically recognize neoepitope sequences generated by ‘aggrecanase’ and matrix metalloproteinase cleavage of aggrecan: application to catabolism in situ and in vitro. Biochem J 1995;305:799–804.
Benya PD, Shaffer JD . Dedifferentiated chondrocytes reexpress the differentiated collagen phenotype when cultured in agarose gels. Cell 1982;30:215–224.
Zanetti NC, Solursh M . Induction of chondrogenesis in limb mesenchymal cultures by disruption of the actin cytoskeleton. J Cell Biol 1984;99:115–123.
Pritzker KPH, Gay S, Jimenez SA, et al. Osteoarthritis cartilage histopathology: grading and staging. Osteoarthr Cartil 2006;14:13–29.
Mateus AR, Seruca R, Machado JC, et al. EGFR regulates RhoA-GTP dependent cell motility in E-cadherin mutant cells. Hum Mol Genet 2007;16:1639–1647.
Yin J, Lu J, Yu F-SX . Role of small GTPase Rho in regulating corneal epithelial wound healing. Invest Ophthalmol Vis Sci 2008;49:900–909.
Nebl G, Fischer S, Penzel R, et al. Dephosphorylation of cofilin is regulated through Ras and requires the combined activities of the Ras-effectors MEK and PI3K. Cell Signal 2004;16:235–243.
Jung J, Kim M, Choi S, et al. Molecular mechanism of cofilin dephosphorylation by ouabain. Cell Signal 2006;18:2033–2040.
Ikebe M, Hartshorne DJ . Phosphorylation of smooth muscle myosin at two distinct sites by myosin light chain kinase. J Biol Chem 1985;260:10027–10031.
Iwabu A, Smith K, Allen FD, et al. Epidermal growth factor induces fibroblast contractility and motility via a protein kinase C delta-dependent pathway. J Biol Chem 2004;279:14551–14560.
Richter A, Drummond DR, MacGarvie J, et al. Contribution of the transforming growth factor-alpha beta-loop beta-sheet to binding and activation of the epidermal growth factor receptor. J Biol Chem 1995;270:1612–1616.
Kamekura S, Kawasaki Y, Hoshi K, et al. Contribution of runt-related transcription factor 2 to the pathogenesis of osteoarthritis in mice after induction of knee joint instability. Arthritis Rheum 2006;54:2462–2470.
Yang X, Chen L, Xu X, et al. TGF-beta/Smad3 signals repress chondrocyte hypertrophic differentiation and are required for maintaining articular cartilage. J Cell Biol 2001;153:35–46.
Alroy I, Yarden Y . The ErbB signaling network in embryogenesis and oncogenesis: signal diversification through combinatorial ligand-receptor interactions. FEBS Lett 1997;410:83–86.
Hackel PO, Zwick E, Prenzel N, et al. Epidermal growth factor receptors: critical mediators of multiple receptor pathways. Curr Opin Cell Biol 1999;11:184–189.
Stanton LA, Sabari S, Sampaio AV, et al. p38 MAP kinase signalling is required for hypertrophic chondrocyte differentiation. Biochem J 2004;378:53–62.
Yoon Y-M, Oh C-D, Kim D-Y, et al. Epidermal growth factor negatively regulates chondrogenesis of mesenchymal cells by modulating the protein kinase C-alpha, Erk-1, and p38 MAPK signaling pathways. J Biol Chem 2000;275:12353–12359.
Yagi R, McBurney D, Horton Jr WE . Bcl-2 positively regulates Sox9-dependent chondrocyte gene expression by suppressing the MEK-ERK1/2 signaling pathway. J Biol Chem 2005;280:30517–30525.
Starkman BG, Cravero JD, Delcarlo M, et al. IGF-I stimulation of proteoglycan synthesis by chondrocytes requires activation of the PI 3-kinase pathway but not ERK MAPK. Biochem J 2005;389:723–729.
Smith MD, Triantafillou S, Parker A, et al. Synovial membrane inflammation and cytokine production in patients with early osteoarthritis. J Rheumatol 1997;24:365–371.
Liacini A, Sylvester J, Qing Li W, et al. Induction of matrix metalloproteinase-13 gene expression by TNF alpha is mediated by MAP kinases, AP-1, and NF-kappa B transcription factors in articular chondrocytes. Exp Cell Res 2003;288:208–217.
Vincourt J-B, Vignaud J-M, Lionneton F, et al. Increased expression of matrilin-3 not only in osteoarthritic articular cartilage but also in cartilage-forming tumors, and down-regulation of SOX9 via epidermal growth factor domain 1-dependent signaling. Arthritis Rheum 2008;58:2798–2808.
Acknowledgements
We acknowledge the assistance of Dr L Coolen, K Pitchers, V Pitelka and J Rockel at The University of Western Ontario. FB is the Canada Research Chair in Musculoskeletal Health. JSM is supported by the Shriners of North America. This study was supported by funding from the Canadian Institutes of Health Research (Grant no. MOP86574) and the University of Western Ontario Schulich Research Opportunities Program.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Appleton, C., Usmani, S., Mort, J. et al. Rho/ROCK and MEK/ERK activation by transforming growth factor-α induces articular cartilage degradation. Lab Invest 90, 20–30 (2010). https://doi.org/10.1038/labinvest.2009.111
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2009.111
Keywords
This article is cited by
-
Restoring the dampened expression of the core clock molecule BMAL1 protects against compression-induced intervertebral disc degeneration
Bone Research (2022)
-
Overexpression of MIG-6 in the cartilage induces an osteoarthritis-like phenotype in mice
Arthritis Research & Therapy (2020)
-
mRNA level of ROCK1, RHOA, and LIMK2 as genes associated with apoptosis in evaluation of effectiveness of adalimumab treatment
Pharmacological Reports (2020)
-
The EphA4 Signaling is Anti-catabolic in Synoviocytes but Pro-anabolic in Articular Chondrocytes
Calcified Tissue International (2020)
-
Identification of Chondrocyte Genes and Signaling Pathways in Response to Acute Joint Inflammation
Scientific Reports (2019)