Abstract
Objective:
To assess the opioid and benzodiazepine usage in a level IV NICU after implementation of pain guidelines.
Study design:
Guidelines were developed for infants undergoing surgical procedures and infants on mechanical ventilation. Data collected for period 1 (July to December 2013) and period 2 (March to August 2014).
Results:
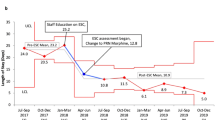
Gestational age, birth weight and infants with hypoxic respiratory failure or requiring major procedures were comparable in two periods. Number of patients exposed to opioids decreased from 62.9% (129/205) in period 1 to 32.8% (82/250) in period 2, P=<0.001. Cumulative dose exposure decreased, opioids in morphine equivalent dose, mg kg−1 (1.64 (0.38 to 6.94) vs 0.51 (0.04 to 2.33), P=0.002), sedatives in midazolam equivalent, mg kg−1 (0.16 (0.03 to 7.39) vs 0.10 (0.00 to 4.00), P=0.03). Ten patients required treatment for iatrogenic opioid withdrawal versus only three in post guideline, P=0.02.
Conclusions:
Evidence-based guidelines led to significant reduction in opioids and sedatives exposure, and in the number of infants requiring methadone for iatrogenic narcotic dependence.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Platt MP, Anand KJ, Aynsley-Green A . The ontogeny of the metabolic and endocrine stress response in the human fetus, neonate and child. Intensive Care Med 1989; 15: S44–S45.
Brummelte S, Chau CM, Cepeda IL, Degenhardt A, Weinberg J, Synnes AR et al. Cortisol levels in former preterm children at school age are predicted by neonatal procedural pain-related stress. Psychoneuroendocrinology 2015; 51: 151–163.
Valeri BO, Ranger M, Chau CM, Cepeda IL, Synnes A, Linhares MB et al. Neonatal invasive procedures predict pain intensity at school age in children born very preterm. Clin J Pain 2016; 32 (12): 1086–1093.
Anand KJ, Sippel WG, Aynsley-Green A . Randomised trial of fentanyl anasethesia in preterm babies undergoing surgery: effects on the stress response. Lancet 1987; 329 (8527): 243–248.
Anand KJ, Brown MJ, Bloom SR, Aynsley-Green A . Studies on the hormonal regulation of fuel metabolism in the human newborn infant undergoing anaesthesia and surgery. Hormone Res 1985; 22: 115–128.
Janvier A, Martinez JL, Barrington K, Lavoie J . Anesthetic technique and postoperative outcome in preterm infants undergoing PDA closure. J Perinatal 2010; 30 (10): 677–682.
Simons SH, van Dijk M, Anand KS, Roofthooft D, van Lingen RA, Tibboel D . Do we still hurt newborn babies? A prospective study of procedural pain and analgesia in neonates. Arch Pediatr Adolesc Med 2003; 157 (11): 1058–1064.
Carbajal R, Rousset A, Danan C, Coquery S, Nolent P, Ducrocq S et al. Epidemiology and treatment of painful procedures in neonates in intensive care units. JAMA 2008; 300 (1): 60–70.
Lago P, Boccuzzo G, Garetti E, Pirelli A, Pieragostini L, Merazzi D et al. Pain management during invasive procedures at Italian NICUs: has anything changed in the last five years? J Matern Fetal Neonatal Med 2013; 26 (3): 303–305.
American Academy of Pediatrics Committee on Fetus and Newborn and Section on Anesthesiology and Pain Medicine. Prevention and management of procedural pain in the neonate: an update. Pediatrics 2016; 137 (2): e20154271.
Taylor BJ, Robbins JM, Gold JI, Logsdon TR, Bird TM, Anand KJ . Assessing postoperative pain in neonates: a multicenter observational study. Pediatrics 2006; 118 (4): e992–e1000.
Hudak ML, Tan RC Committee on Drugs; Committee on Fetus and Newborn; American Academy of Pediatrics. Neonatal drug withdrawal. Pediatrics 2012; 129 (2): e540–e560.
Anand KJ, Willson DF, Berger J, Harrison R, Meert KL, Zimmerman J et al. Tolerance and withdrawal from prolonged opioid use in critically ill children. Pediatrics 2010; 125 (5): e1208–e1225.
Galinkin J, Koh JL, Committee on Drugs; Section on Anesthesiology and Pain Medicine; American Academy of Pediatrics. Recognition and management of iatrogenically induced opioid dependence and withdrawal in children. Pediatrics 2014; 133 (1): 152–155.
McPherson C, Grunau RE . Neonatal pain control and neurologic effects of anesthetics and sedatives in preterm infants. Clin Perinatol 41 (1): 209–227.
Anand KJ, Hall RW, Desai N, Shephard B, Bergqvist LL, Young TE et al, NEOPAIN Trial Investigators Group. Effects of morphine analgesia in ventilated preterm neonates: primary outcomes from the NEOPAIN randomised trial. Lancet 2004; 363 (9422): 1673–1682.
Carbajal R, Eriksson M, Courtois E . Sedation and analgesia practices in neonatal intensive care units (EUROPAIN): results from a prospective cohort study. Lancet Respir Med 2015; 3 (10): 796–812.
de Wildt SN, Kearns GL, Hop WC, Murry DJ, Abdel-Rahman SM, van den Anker JN . Pharmacokinetics and metabolism of intravenous midazolam in preterm infants. Clin Pharmacol Ther 2001; 70 (6): 525–531.
Deindl P, Giordano V, Fuiko R, Waldhoer T, Unterasinger L, Berger A et al. The implementation of systematic pain and sedation management has no impact on outcome in extremely preterm infants. Acta Paediatr 2016; 105 (7): 798–805.
Sharek PJ, Powers R, Koehn A, Anand KJ . Evaluation and development of potentially better practices to improve pain management of neonates. Pediatrics 2006; 118: S78–S86.
Dyke MP, Kohan R, Evans S . Morphine increases synchronous ventilation in preterm infants. J Paediatr Child Health 1995; 31 (3): 176–179.
Furdon SA, Eastman M, Benjamin K, Horgan MJ . Outcome measures after standardized pain management strategies in postoperative patients in the neonatal intensive care unit. J Perinat Neonatal Nurs 1998; 12 (1): 58–69.
Deindl P, Unterasinger L, Kappler GP . Successful implementation of a neonatal pain and sedation protocol at 2 NICUs. Pediatrics 2013; 132: e211–e218.
Taketomo CK, Hodding JH, Kraus DM . The Lexicomp Pediatric & Neonatal Dosage Handbook. Wolters Kluwer: Hudson, OH, 2013.
Anand KJ, International Evidence-Based Group for Neonatal Pain. Consensus statement for the prevention and management of pain in the newborn. Arch Pediatr Adolesc Med 2001; 155 (2): 173–180.
Lago P, Garetti E, Merazzi D, Pieragostini L, Ancora G, Pirelli A et al. Guidelines for procedural pain in the newborn. Acta Paediatr 2009; 98 (6): 932–939.
Jeffries SA, McGloin R, Pitfield AF, Carr RR . Use of methadone for prevention of opioid withdrawal in critically ill children. Can J Hosp Pharm 2012; 65 (1): 12–18.
Barr J, Zomorodi K, Bertaccini EJ, Shafer SL, Geller E . A double-blind, randomized comparison of i.v. lorazepam versus midazolam for sedation of ICU patients via a pharmacologic model. Anesthesiology 2001; 95 (2): 286–298.
Fleishman R, Zhou C, Gleason C, Larison C, Myaing MT, Mangione-Smith R . Standardizing morphine use for ventilated preterm neonates with a nursing-driven comfort protocol. J Perinatol 2015; 35 (1): 46–51.
Deeter KH, King MA, Ridling D, Irby GL, Lynn AM, Zimmerman JJ . Successful implementation of a pediatric sedation protocol for mechanically ventilated patients. Crit Care Med 2011; 39 (4): 683–688.
Gharavi B, Schott C, Nelle M, Reiter G, Linderkamp O . Pain management and the effect of guidelines in neonatal units in Austria, Germany and Switzerland. Pediatr Int 2007; 49 (5): 652–658.
Bhandari V, Bergqvist LL, Kronsberg SS, Barton BA, Anand KJ, NEOPAIN Trial Investigators Group. Morphine administration and short-term pulmonary outcomes among ventilated preterm infants. Pediatrics 2005; 116 (2): 352–359.
Saarenmaa E, Huttunen P, Leppäluoto J, Meretoja O, Fellman V . Advantages of fentanyl over morphine in analgesia for ventilated newborn infants after birth: A randomized trial. J Pediatr 1999; 134 (2): 144–150.
Ancora G, Lago P, Garetti E, Pirelli A, Merazzi D, Mastrocola M et al. Efficacy and safety of continuous infusion of fentanyl for pain control in preterm newborns on mechanical ventilation. J Pediatr 2013; 163 (3): 645–651.
Hall RW, Kronsberg SS, Barton BA, Kaiser JR, Anand KJ, NEOPAIN Trial Investigators Group. Morphine, hypotension, and adverse outcomes among preterm neonates: who's to blame? Secondary results from the NEOPAIN trial. Pediatrics 2005; 115 (5): 1351–1359.
Bellù R, de Waal K, Zanini R . Opioids for neonates receiving mechanical ventilation: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2010; 95 (4): F241–F251.
Dominguez KD, Lomako DM, Katz RW, Kelly HW . Opioid withdrawal in critically ill neonates. Ann Pharmacotherapy 2003; 37 (4): 473–477.
Franck LS, Vilardi J, Durand D, Powers R . Opioid withdrawal in neonates after continuous infusions of morphine or fentanyl during extracorporeal membrane oxygenation. Am J Crit Care 1998; 7 (5): 364–369.
Best KM, Boullata JI, Curley MA . Risk factors associated with iatrogenic opioid and benzodiazepine withdrawal in critically ill pediatric patients: a systematic review and conceptual model. Pediatr Crit Care Med 2015; 16 (2): 175–183.
Anand KJ, Barton BA, McIntosh N, Lagercrantz H, Pelausa E, Young TE et al. Analgesia and sedation in preterm neonates who require ventilatory support: results from the NOPAIN trial. Neonatal outcome and prolonged analgesia in neonates. Arch Pediatr Adolesc Med 1999; 153 (4): 331–338.
Ng E, Taddio A, Ohlsson A . Intravenous midazolam infusion for sedation of infants in the neonatal intensive care unit. Cochrane Database Syst Rev 2012; 13 (6): CD002052.
Wong I St, John-Green C, Walker SM . Opioid-sparing effects of perioperative paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs) in children. Paediatr Anaesth 2013; 23 (6): 475–495.
Celia I, de Wild SN, van Disk M, van den Berg MM, van den Bosch GE, Duivenvoorden HJ et al. Effect of intravenous paracetamol on postoperative morphine requirements in neonates and infants undergoing major non cardiac surgery: a randomized controlled trial. JAMA 2013; 309 (2): 149–154.
Ohlsson A, Shah PS . Paracetamol (acetaminophen) for prevention or treatment of pain in newborns. Cochrane Database Syst Rev 2016; (10): CD011219.
Menon G1, Boyle EM, Bergqvist LL, McIntosh N, Barton BA, Anand KJ . Morphine analgesia and gastrointestinal morbidity in preterm infants: secondary results from the NEOPAIN trial. Arch Dis Child Fetal Neonatal Ed 2008; 93 (5): F362–F367.
Gallo AM . The fifth vital sign: implementation of the Neonatal Infant Pain Scale. J Obstet Gynecol Neonatal Nurs 2003; 32 (2): 199–206.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Rana, D., Bellflower, B., Sahni, J. et al. Reduced narcotic and sedative utilization in a NICU after implementation of pain management guidelines. J Perinatol 37, 1038–1042 (2017). https://doi.org/10.1038/jp.2017.88
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.88
This article is cited by
-
Adequate Pain Management and Sedation in the Neonate: a Fine Balance
Current Treatment Options in Pediatrics (2018)