Abstract
Objective:
To investigate the association between small-for-gestational age (SGA) and neurocognitive impairment at 2 years of corrected age among infants born at preterm gestational ages.
Study Design:
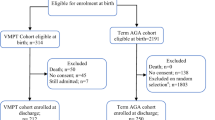
A secondary analysis of a prospectively conducted NICHD/Maternal-Fetal Medicine Units BEAM trial. Non-anomalous pregnancies delivered before 37 weeks of gestation were included in the analysis. Neurocognitive outcomes at 2 years of corrected age were compared between infants who were SGA (<10% for gestational age) and those appropriately grown (AGA). The primary outcome was a severe or moderate neurocognitive impairment at 2 years of corrected age among survivors, defined as either mental (MDI) or psychomotor (PDI) developmental index score <70 for severe and <85 for moderate impairment.
Results:
Of 2299 preterm neonates 67 (3%) were SGA. SGA infants were more often twin pregnancies (31% vs 17%, P=0.003) and delivered more often by cesarean section (63% vs 40%, P<0.001) at similar gestational ages (30.0±2.6 vs 29.5±2.8 weeks, P=0.11). At 2 years of corrected age, SGA and AGA survivors had similar rates of neurocognitive impairment (MDI <70: 18% vs 18%, P=1.0; MDI <85: 44% vs 46%, P=0.96; PDI <70: 20% vs 15%, P=0.51; PDI <85: 40% vs 34%, P=0.48).
Conclusion:
In this cohort, SGA at preterm gestational ages was associated with similar rates of neurocognitive impairment at two years of corrected age among surviving infants.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
March of Dimes. White paper on preterm birth: the global and regional toll, 2009.
Saigal S, Doyle LW . An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008; 371: 261–269.
De Jesus LC, Pappas A, Shankaran S, Li L, Das A, Bell EF et al. Outcomes of small for gestational age infants born at <27 weeks' gestation. J Pediatr 2013; 163 (55–60): e1–e3.
Bickle Graz M, Tolsa JF, Fischer Fumeaux CJ . Being small for gestational age: does it matter for the neurodevelopment of premature infants? A cohort study. PLoS ONE 2015; 10: e0125769.
Lee AC, Katz J, Blencowe H, Cousens S, Kozuki N, Vogel JP et al. National and regional estimates of term and preterm babies born small for gestational age in 138 low-income and middle-income countries in 2010. Lancet Glob Health 2013; 1: e26–36.
Anderson MS . Intrauterine growth restriction and the small-for-gestational-age infant. In: MacDonald MG, Mullett MD (eds). Avery's Neonatology Pathophysiology and Management of the Newborn. Lippincott Williams and Wilkins: Philadelphia, 2005, pp 491-492.
Jelliffe-Pawlowski LL, Hansen RL . Neurodevelopmental outcome at 8 months and 4 years among infants born full-term small-for-gestational-age. J Perinatol 2004; 24: 505–514.
Rouse DJ, Hirtz DG, Thom E, Varner MW, Spong CY, Mercer BM et al. A randomized, controlled trial of magnesium sulfate for the prevention of cerebral palsy. N Engl J Med 2008; 359: 895–905.
Carey JC, Klebanoff MA, Hauth JC, Hillier SL, Thom EA, Ernest JM et al. Metronidazole to prevent preterm delivery in pregnant women with asymptomatic bacterial vaginosis. National Institute of Child Health and Human Development Network of Maternal-Fetal Medicine Units. N Engl J Med 2000; 342: 534–540.
Brenner WE, Edelman DA, Hendricks CH . A standard of fetal growth for the United States of America. Am J Obstet Gynecol 1976; 126: 555–564.
Bayley N . Bayley Scales of Infant Development II. Psychological Corp: San Antonio, TX, 1993.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126: 443–456.
Amaru RC, Bush MC, Berkowitz RL, Lapinski RH, Gaddipati S . Is discordant growth in twins an independent risk factor for adverse neonatal outcome? Obstet Gynecol 2004; 103: 71–76.
Fenton TR, Nasser R, Eliasziw M, Kim JH, Bilan D, Sauve R . Validating the weight gain of preterm infants between the reference growth curve of the fetus and the term infant. BMC Pediatr 2013; 13: 92.
Johnson S . Cognitive and behavioural outcomes following very preterm birth. Semin Fetal Neonatal Med 2007; 12: 363–373.
Aylward GP . Neurodevelopmental outcomes of infants born prematurely. J Dev Behav Pediatr 2014; 35: 394–407.
Guellec I, Lapillonne A, Renolleau S, Charlaluk ML, Roze JC, Marret S et al. Neurologic outcomes at school age in very preterm infants born with severe or mild growth restriction. Pediatrics 2011; 127: e883–e891.
Grobman WA, Lai Y, Rouse DJ, Spong CY, Varner MW, Mercer BM et al. The association of cerebral palsy and death with small-for-gestational-age birthweight in preterm neonates by individualized and population-based percentiles. Am J Obstet Gynecol 2013; 209 (340): e1–e5.
Sharma P, McKay K, Rosenkrantz TS, Hussain N . Comparisons of mortality and pre-discharge respiratory outcomes in small-for-gestational-age and appropriate-for-gestational-age premature infants. BMC Pediatr 2004; 4: 9.
Qiu X, Lodha A, Shah PS, Sankaran K, Seshia MM, Yee W et al. Neonatal outcomes of small for gestational age preterm infants in Canada. Am J Perinatol 2012; 29: 87–94.
Acknowledgements
We acknowledge the assistance of NICHD, the MFMU Network and the Protocol Subcommittee in making the database available on behalf of the project. The contents of this report represent the views of the authors and do not represent the views of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This manuscript was presented in oral format at the 36th Annual Meeting of the Society for Maternal-Fetal Medicine, Atlanta, GA, 1 to 6 February 2016.
Rights and permissions
About this article
Cite this article
Girsen, A., Do, S., El-Sayed, Y. et al. Association between small-for-gestational age and neurocognitive impairment at two years of corrected age among infants born at preterm gestational ages: a cohort study. J Perinatol 37, 958–962 (2017). https://doi.org/10.1038/jp.2017.58
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.58
This article is cited by
-
Developmental trajectories of late preterm infants and predictors of academic performance
Pediatric Research (2023)