Abstract
Objective:
The objective of this study is to determine child health, development and educational outcomes for infants born following preterm prelabor rupture of the membrane (PPROM).
Study Design:
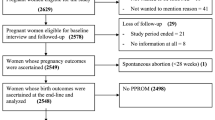
Population-based record linkage cohort study using data from NSW, Australia, 2001 to 2014.
Results:
Of 121 822 births at 20 to 37 weeks, 18 799 (15%) followed PPROM, 56 406 (46%) followed spontaneous labor and 46 617 (38%) were planned. Compared with infants of a similar gestational age born following spontaneous labor or planned delivery, exposure to PPROM did not increase the risk of childhood mortality, childhood hospitalization, developmentally vulnerable at school entry, low reading or numeracy scores. Median latency ranged from 12 days (interquartile range 3 to 37 days) at 25 weeks to 1 day (0 to 2 days) at 36 weeks. Longer latency and more advanced gestational age at birth were associated with better outcomes.
Conclusion:
Infants born following PPROM are at no greater risk of adverse child health, development and education outcomes than those of similar gestational age born without PPROM.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Ananth CV, Vintzileos AM . Epidemiology of preterm birth and its clinical subtypes. J Matern Fetal Neonatal Med 2006; 19 (12): 773–782.
Goldenberg RL, Culhane JF, Iams JD, Romero R . Epidemiology and causes of preterm birth. Lancet 2008; 371 (9606): 75–84.
American College of Obstetrics and Gynecology. ACOG Practice Bulletin No. 139: premature rupture of membranes. Obstet Gynecol 2013; 122 (4): 918–930.
Caughey AB, Robinson JN, Norwitz ER . Contemporary diagnosis and management of preterm premature rupture of membranes. Rev Obstet Gynecol 2008; 1 (1): 11–22.
Kenyon S, Pike K, Jones DR, Brocklehurst P, Marlow N, Salt A et al. Childhood outcomes after prescription of antibiotics to pregnant women with preterm rupture of the membranes: 7-year follow-up of the ORACLE I trial. Lancet 2008; 372 (9646): 1310–1318.
Kibel M, Asztalos E, Barrett J, Dunn MS, Tward C, Pittini A et al. Outcomes of pregnancies complicated by preterm premature rupture of membranes between 20 and 24 weeks of gestation. Obstet Gynecol 2016; 128 (2): 313–320.
Mura T, Picaud JC, Larroque B, Galtier F, Marret S, Roze JC et al. Cognitive impairment at age 5 years in very preterm infants born following premature rupture of membranes. J Pediatr 2013; 163 (2): 435–440.
Pasquier JC, Bujold E, Rabilloud M, Picaud JC, Ecochard R, Claris O et al. Effect of latency period after premature rupture of membranes on 2 years infant mortality (DOMINOS study). Eur J Obstet Gynecol Reprod Biol 2007; 135 (1): 21–27.
Patkai J, Schmitz T, Anselem O, Mokbat S, Jarreau PH, Goffinet F et al. Neonatal and two-year outcomes after rupture of membranes before 25 weeks of gestation. Eur J Obstet Gynecol Reprod Biol 2013; 166 (2): 145–150.
Spinillo A, Capuzzo E, Stronati M, Ometto A, Orcesi S, Fazzi E . Effect of preterm premature rupture of membranes on neurodevelopmental outcome: follow up at two years of age. Br J Obstet Gynaecol 1995; 102 (11): 882–887.
Vermeulen GM, Bruinse HW, de Vries LS . Perinatal risk factors for adverse neurodevelopmental outcome after spontaneous preterm birth. Eur J Obstet Gynecol Reprod Biol 2001; 99 (2): 207–212.
Brinkman S, Silburn S, Lawrence D, Oberklaid F, Goldfield S, Sayers M et al Construct and concurrent validity of the Australian Early Development Index: A Report to the Technical Advisory Group for the Australian Early Development Index: Building Better Communities for Children Project. http://www.aedc.gov.au/resources/publication 2006.
Janus M, Offord DR . Development and psychometric properties of the early development instrument (edi): a measure of children’s school readiness. Can J Behav Sci 2007; 39 (1): 1–22.
Australian Early Development Census International use of the Early Development Index. http://www.aedc.gov.au/about-the-aedc/history/international-use-of-the-early-development-instrument.
Australian Curriculum Assessment and Reporting Authority (ACARA). National Assessment Program—Literacy and Numeracy 2013: Technical Report. http://www.nap.edu.au/_resources/NAPLAN_2013_technical_report.pdf. 2014.
Bentley JP, Ford JB, Taylor LK, Irvine KA, Roberts CL . Investigating linkage rates among probabilistically linked birth and hospitalization records. BMC Med Res Methodol 2012; 12: 149.
Centre for Health Record Linkage. CHeReL Quality Assurance Procedures for Record Linkage. http://www.cherel.org.au/quality-assurance.
Hennessy D, Torvaldsen S, Roberts CL Linkage Rate Between NSW Perinatal Data Collection Birth Records and Government School NAPLAN Educational Records, by Gestational Age at Birth. http://hdl.handle.net/2123/15755 2016.
Bentley JP, Roberts CL, Bowen JR, Martin AJ, Morris JM, Nassar N . Planned birth before 39 weeks and child development: a population-based study. Pediatrics 2016; 138 (6).
NSW Health Department. Validation study: NSW midwives data collection. NSW Public Health Bull 2000; 9 (S-2): 97–99. http://www.health.nsw.gov.au/phb/Publications/NSW-mothers-babies-1998.pdf.
Taylor L, Travis S, Pym M, Olive E, Henderson-Smart D . How useful are hospital morbidity data for monitoring conditions occurring in the perinatal period? Aust N Z J Obstet Gynecol 2005; 45: 36–41.
Khambalia AZ, Roberts CL, Nguyen M, Algert CS, Nicholl MC, Morris J . Predicting date of birth and examining the best time to date a pregnancy. Int J Gynaecol Obstet 2013; 123 (2): 105–109.
Buchanan S, Crowther C, Morris J . Preterm prelabour rupture of the membranes: a survey of current practice. Aust N Z J Obstet Gynecol 2004; 44 (5): 400–403.
Hannah ME, Ohlsson A, Farine D, Hewson SA, Hodnett ED, Myhr TL et al. Induction of labor compared with expectant management for prelabor rupture of the membranes at term. N Engl J Med 1996; 334 (16): 1005–1010.
Australian Government. A Snapshot of Early Childhood Development in Australia 2012—AEDI National Report. https://www.aedc.gov.au/resources/reports 2013.
Roberts CL, Lancaster PA . Australian national birthweight percentiles by gestational age. Med J Aust 1999; 170 (3): 114–118.
Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2006. Catalogue 2033.0.55.001. http://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001/. 2008.
Sydney eScholarship Repository. Childhood Outcomes Following Preterm Prelabor Rupture of the Membranes (PPROM): A Population-Based Record Linkage Cohort Study https://ses.library.usyd.edu.au/handle/2123/9877 2017.
Kenyon S, Pike K, Jones DR, Brocklehurst P, Marlow N, Salt A et al. Childhood outcomes after prescription of antibiotics to pregnant women with spontaneous preterm labour: 7-year follow-up of the ORACLE II trial. Lancet 2008; 372 (9646): 1319–1327.
Marlow N, Pike K, Bower E, Brocklehurst P, Jones D, Kenyon S et al. Characteristics of children with cerebral palsy in the ORACLE children study. Dev Med Child Neurol 2012; 54 (7): 640–646.
Livinec F, Ancel PY, Marret S, Arnaud C, Fresson J, Pierrat V et al. Prenatal risk factors for cerebral palsy in very preterm singletons and twins. Obstet Gynecol 2005; 105 (6): 1341–1347.
Hadley CB, Main DM, Gabbe SG . Risk factors for preterm premature rupture of the fetal membranes. Am J Perinatol 1990; 7 (4): 374–379.
Ladfors L, Mattsson LA, Eriksson M, Milsom I . Prevalence and risk factors for prelabor rupture of the membranes (PROM) at or near-term in an urban Swedish population. J Perinat Med 2000; 28 (6): 491–496.
Drassinower D, Friedman AM, Obican SG, Levin H, Gyamfi-Bannerman C . Prolonged latency of preterm prelabour rupture of membranes and neurodevelopmental outcomes: a secondary analysis. BJOG 2016; 123 (10): 1629–1635.
Walker MW, Picklesimer AH, Clark RH, Spitzer AR, Garite TJ . Impact of duration of rupture of membranes on outcomes of premature infants. J Perinatol 2014; 34 (9): 669–672.
Roberts CL, Ford JB, Algert CS, Morris JM. Prolonged latency of preterm prelabour rupture of membranes and neurodevelopmental outcomes. BJOG 2017; 124: 830–831..
Drassinower D, Friedman AM, Obican SG, Levin H, Gyamfi-Bannerman C . Prolonged latency of preterm premature rupture of membranes and risk of cerebral palsy. J Matern Fetal Neonatal Med 2016; 29 (17): 2748–2752.
Roberts CL, Bell JC, Ford JB, Morris JM . Monitoring the quality of maternity care—how well are labour and delivery events reported in population health data? Paed Perinatal Epidemiol 2009; 23: 144–152.
Moster D, Lie RT, Irgens LM, Bjerkedal T, Markestad T . The association of Apgar score with subsequent death and cerebral palsy: a population-based study in term infants. J Pediatr 2001; 138 (6): 798–803.
Acknowledgements
This study uses unit record data from the Australian Early Development Census (AEDC) and the National Assessment Program—Literacy and Numeracy. We thank the Ministry of Health, the NSW Department of Education and Communities (NAPLAN), and the Australian Government Department of Education and Training (AEDC) for provision of population data, and the NSW Centre for Health Record Linkage for record linkage. The findings and views reported in this article are those of the authors and should not be attributed to the departments that provided data. We thank Dr Jillian Patterson for providing supplementary statistical analysis. This work was supported by an Australian National Health and Medical Research Council (NHRMC) project grant (APP1085775). CLR is funded by an NHMRC Senior Research Fellowship (APP1021025). PW and ST were funded through a New South Wales Ministry of Health ‘Population Health and Health Services Research Support Program’ grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Roberts, C., Wagland, P., Torvaldsen, S. et al. Childhood outcomes following preterm prelabor rupture of the membranes (PPROM): a population-based record linkage cohort study. J Perinatol 37, 1230–1235 (2017). https://doi.org/10.1038/jp.2017.123
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.123
This article is cited by
-
Outpatient versus inpatient care for preterm premature rupture of membranes before 34 weeks of gestation
Scientific Reports (2019)