Abstract
Objective:
Determine time-to-delivery and mode-of-delivery in labor induction among women with unripe cervix.
Study design:
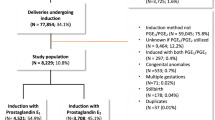
7551 nulliparous women with singleton deliveries, ⩾37 weeks, Bishop Score ⩽6, induced with dinoprostone, misoprostol or transcervical single balloon catheter. Linear regression analysis was used to estimate mean time-to-delivery with β-estimates and 95% confidence intervals with adjustments. Multivariable logistic regression analysis was used to calculate odds of cesarean delivery, instrumental vaginal delivery, maternal and neonatal outcomes.
Results:
Adjusted mean time-to-delivery was 6.9 and 1.5 h shorter, respectively, when inducing labor with balloon catheter (mean 18.3 h, β −6.9, 95% confidence intervals; −7.6 to −6.3) or misoprostol (mean 23.7 h, β −1.5, 95% confidence intervals; −2.3 to −0.8) compared with dinoprostone (mean 25.2 h). There were no significant differences in adverse maternal or infant outcomes between induction methods.
Conclusions:
Balloon catheter is the most effective induction method with respect to time-to-delivery in nulliparous women at term compared with prostaglandin methods.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ekeus C, Lindgren H . Induced Labor in Sweden, 1999-2012: a Population-Based Cohort Study. Birth 2016; 43 (2): 125–133.
National Collaborating Centre for Ws, Children's H. National Institute for Health and Clinical Excellence: Guidance. Induction of Labour. RCOG Press. National Collaborating Centre for Women's and Children's Health: London, UK, 2008.
Socialstyrelsen. Graviditeter, förlossningar och nyfödda barn. Medicinska födelseregistret 1973–2013. 2014.
Caughey AB, Sundaram V, Kaimal AJ, Gienger A, Cheng YW, McDonald KM et al. Systematic review: elective induction of labor versus expectant management of pregnancy. Ann Intern Med 2009; 151 (4): 252–263 w253-263.
Cheng YW, Delaney SS, Hopkins LM, Caughey AB . The association between the length of first stage of labor, mode of delivery, and perinatal outcomes in women undergoing induction of labor. Am J Obstet Gynecol 2009; 201 (5): 477.e471–477.
Crane JM . Factors predicting labor induction success: a critical analysis. Clin Obstet Gynecol 2006; 49 (3): 573–584.
Roos N, Sahlin L, Ekman-Ordeberg G, Kieler H, Stephansson O . Maternal risk factors for postterm pregnancy and cesarean delivery following labor induction. Acta Obstet Gynecol Scand 2010; 89 (8): 1003–1010.
Walker KF, Bugg GJ, Macpherson M, McCormick C, Grace N, Wildsmith C et al. Randomized Trial of Labor Induction in Women 35 Years of Age or Older. N Engl J Med 2016; 374 (9): 813–822.
Mishanina E, Rogozinska E, Thatthi T, Uddin-Khan R, Khan KS, Meads C . Use of labour induction and risk of cesarean delivery: a systematic review and meta-analysis. Can Med Assoc J 2014; 186 (9): 665–673.
Glantz JC . Term labor induction compared with expectant management. Obstet Gynecol 2010; 115 (1): 70–76.
Jozwiak M, Bloemenkamp KW, Kelly AJ, Mol BW, Irion O, Boulvain M . Mechanical methods for induction of labour. Cochrane Database Syst Rev 2012; 3: Cd001233.
WHO Guidelines Approved by the Guidelines Review Committee. WHO Recommendations for Induction of Labour. World Health Organization. (c) World Health Organization 2011: Geneva, 2011.
Pennell CE, Henderson JJ, O'Neill MJ, McChlery S, Doherty DA, Dickinson JE . Induction of labour in nulliparous women with an unfavourable cervix: a randomised controlled trial comparing double and single balloon catheters and PGE2 gel. BJOG 2009; 116 (11): 1443–1452.
Jozwiak M, Oude Rengerink K, Benthem M, van Beek E, Dijksterhuis MG, de Graaf IM et al. Foley catheter versus vaginal prostaglandin E2 gel for induction of labour at term (PROBAAT trial): an open-label, randomised controlled trial. Lancet 2011; 378 (9809): 2095–2103.
Ten Eikelder ML, Oude Rengerink K, Jozwiak M, de Leeuw JW, de Graaf IM, van Pampus MG et al. Induction of labour at term with oral misoprostol versus a Foley catheter (PROBAAT-II): a multicentre randomised controlled non-inferiority trial. Lancet 2016; 387 (10028): 1619–1628.
Prager M, Eneroth-Grimfors E, Edlund M, Marions L . A randomised controlled trial of intravaginal dinoprostone, intravaginal misoprostol and transcervical balloon catheter for labour induction. BJOG 2008; 115 (11): 1443–1450.
Stephansson O, Sandstrom A, Petersson G, Wikstrom AK, Cnattingius S . Prolonged second stage of labour, maternal infectious disease, urinary retention and other complications in the early postpartum period. BJOG 2016; 123 (4): 608–616.
ACOG Committee on Practice Bulletins — Obstetrics. ACOG Practice Bulletin No. 107: Induction of labor. Obstetrics and gynecology 2009; 114 (2 Pt 1): 386–397.
Alfirevic Z, Aflaifel N, Weeks A . Oral misoprostol for induction of labour. Cochrane Database Syst Rev 2014; 6: Cd001338.
Delaney S, Shaffer BL, Cheng YW, Vargas J, Sparks TN, Paul K et al. Labor induction with a Foley balloon inflated to 30 mL compared with 60 mL: a randomized controlled trial. Obstet Gynecol 2010; 115 (6): 1239–1245.
Aghideh FK, Mullin PM, Ingles S, Ouzounian JG, Opper N, Wilson ML et al. A comparison of obstetrical outcomes with labor induction agents used at term. J Matern Fetal Neonat Med 2014; 27 (6): 592–596.
Alfirevic Z, Keeney E, Dowswell T, Welton NJ, Medley N, Dias S et al. Which method is best for the induction of labour? A systematic review, network meta-analysis and cost-effectiveness analysis. Health Technol Assess 2016; 20 (65): 1–584.
Acknowledgements
This study was supported by grants from the Swedish Research Council (2013-2429, OS) and by grants provided by the Stockholm County Council (ALF project 20130156, OS). The regional ethical committee at Karolinska Institutet, Stockholm, Sweden approved the study protocol (No.2009/275-31 and No.2012/365-32).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Rights and permissions
About this article
Cite this article
Wollmann, C., Ahlberg, M., Petersson, G. et al. Time-to-delivery and delivery outcomes comparing three methods of labor induction in 7551 nulliparous women: a population-based cohort study. J Perinatol 37, 1197–1203 (2017). https://doi.org/10.1038/jp.2017.122
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.122
This article is cited by
-
Safety and Efficacy of Cervical Ripening and Induction of Labor Using Prostaglandin E1 in Primiparas, Multiparas and Grand Multiparas
The Journal of Obstetrics and Gynecology of India (2023)