Abstract
Objective:
Nonspecific manifestations and a varied distribution of brain lesions can delay the diagnosis of herpes simplex encephalitis (HSE) in neonates. The aim of this study was to report predominant brain lesions in neonatal HSE, and then to investigate the association between pattern of predominant brain lesions, clinical variables and neurodevelopmental outcome.
Study Design:
A multicenter retrospective study was performed in neonates diagnosed with HSE between 2009 and 2014. Magnetic resonance (MR) images, including diffusion-weighted images, were obtained in the acute and chronic phase.
Results:
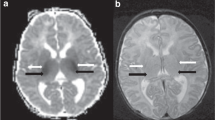
Three predominant areas of brain injury could be defined based on characteristic MRI findings in 10 of the 13 infants (77%). The inferior frontal/temporal pole area was involved in five (38%) patients. The watershed distribution was present in six (46%) patients. Four (31%) infants involved the corticospinal tract area. No significant association was found between any predominant distribution of brain lesion pattern and sex, country, viral type or viral load. However, the corticospinal tract involvement was significantly associated with motor impairment (P=0.045).
Conclusion:
Three predominant areas of brain lesion could be recognized in neonatal HSE. Recognition of those areas can improve prediction of neurodevelopmental outcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Corey L, Wald A . Maternal and neonatal herpes simplex virus infections. N Engl J Med 2009; 361: 1376–1385.
Kimberlin DW, Lin CY, Jacobs RF, Powell DA, Corey L, Gruber WC et al. Safety and efficacy of high-dose intravenous acyclovir in the management of neonatal herpes simplex virus infection. Pediatrics 2001; 108: 203–208.
Lepez-Medina E, Cantey JB, Sanchez PJ . The mortality of neonatal herpes simplex virus infection. J Pediatr 2015; 166: 1529–1532.
Kimberlin DW . Herpes simplex virus infections of the central nervous system. Semin Pediatr Infect Dis 2003; 14: 83–89.
Kimberlin DW, Lin CY, Jacobs RF, Powell DA, Frenkel LM, Gruber WC et al. Natural history of neonatal herpes simplex virus infections in the acyclovir era. Pediatrics 2001; 108: 223–229.
Vossough A, Zimmerman RA, Bilaniuk LT, Schwartz EM . Imaging findings of neonatal herpes simplex virus type 2 encephalitis. Neuroradiology 2008; 50: 355–366.
Pelligra G, Lynch N, Miller SP, Sargent MA, Osiovich H . Brainstem involvement in neonatal herpes simplex virus type 2 encephalitis. Pediatrics 2007; 120: e442.
Noorbehesht B, Enzmann DR, Sullender W, Bradley JS, Arvin AM . Neonatal herpes simplex encephalitis: correlation of clinical and CT findings. Radiology 1987; 162: 813–819.
Herman TE, Cleveland RH, Kushner DC, Taveras JM . CT of neonatal herpes encephalitis. Am J Neuroradiol 1985; 6: 773–775.
Whitley R, Arvin A, Prober C, Corey L, Burchett S, Plotkin S et al. Predictors of morbidity and mortality in neonates with herpes simplex virus infections. The National Institute Of Allergy And Infectious Diseases Collaborative Antiviral Study Group. N Engl J Med 1991; 324: 450–454.
Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B . Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997; 39: 214–223.
Ikuzawa M, Matsushita Y, Nakase A . The Kyoto Scale of Psychological Development, 2nd edn. Nakanishiya Publishers: Kyoto, Japan, 1995 [in Japanese].
Luiz D, Barnard A, Knosen N, Kotras N, Horrocks S, McAlinden P et al. Griffiths Mental Development Scales: Extended Revised. Two To Eight Years. Administration Manual. Hogrefe: Oxford, UK, 2006.
Kimberlin DW, Whitley RJ, Wan W, Powell DA, Storch G, Ahmed A et al. Oral acyclovir suppression and neurodevelopment after neonatal herpes. N Engl J Med 2011; 365: 1284–1292.
Kimura H, Futamura M, Kito H, Ando T, Goto M, Kuzushima K et al. Detection of viral DNA in neonatal herpes simplex virus infections: frequent and prolonged presence in serum and cerebrospinal fluid. J Infect Dis 1991; 164: 289–293.
Melvin AJ, Mohan KM, Schiffer JT, Drolette LM, Mararet A, Corey L et al. Plasma and cerebrospinal fluid herpes simplex virus levels at diagnosis and outcome of neonatal infection. J Pediatr 2015; 166: 827–833.
Sakai T, Abe Y, Sassa K, Yamanouchi H . A case of neonatal herpes simplex virus encephalitis with characteristic MRI features in the early period. No To Hattatsu 2014; 46: 447–449 [in Japanese].
Bajaj M, Mody S, Natarajan G . Clinical and neuroimaging findings in neonatal herpes virus infection. J Pediatr 2014; 165: 404–407.
Verboon-Maciolek MA, Groenendaal F, Cowan F, Govaert P, van Loon AM, de Vries LS . White matter damage in neonatal enterovirus meningoencephalitis. Neurology 2006; 66: 1267–1269.
Verboon-Maciolek MA, Groenendaal F, Hahn CD, Hellmann J, van Loon AM, Boivin G et al. Human parechovirus causes encephalitis with white matter injury in neonates. Ann Neurol 2008; 64: 266–273.
Yeom JS, Kim YS, Seo JH, Park JS, Park ES, Lim JY et al. Distinctive pattern of white matter injury in neonates with rotavirus infection. Neurology 2015; 84: 21–27.
Verboon-Maciolek MA, Truttmenn AC, Groenendaal F, Skranes J, Dollner H, Hunt RW et al. Development of cystic periventricular leukomalacia in newborn infants after rotavirus infection. J Pediatr 2012; 160: 165–168.
Dhawan A, Kecskes Z, Jyoti R, Kent AL . Early diffusion-weighted magnetic resonance imaging findings in neonatal herpes encephalitis. J Pediatr Child Health 2006; 42: 824–826.
Kubota T, Ito M, Maruyama K, Kato Y, Miyajima Y, Ogawa A et al. Serial diffusion-weighted imaging of neonatal herpes encephalitis: a case report. Brain Dev 2007; 29: 171–173.
Acknowledgements
We thank our infant patients and their families whose participation made this research possible. We also thank Dr Kubota, Dr Tsuji and Dr Ando for recruiting the patients and Dr Murk for the virological studies in Utrecht. All phases of this study were supported by a Grant-in-Aid for Scientific Research (C) (no. 26461543); Grants for Scientific Research on Innovative Areas (15H01578), from the Ministry of Education, Culture, Sports, Science and Technology in Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Kidokoro, H., de Vries, L., Ogawa, C. et al. Predominant area of brain lesions in neonates with herpes simplex encephalitis. J Perinatol 37, 1210–1214 (2017). https://doi.org/10.1038/jp.2017.114
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.114
This article is cited by
-
Uncommon acute neuroimaging findings in severe neonatal herpes simplex virus 2 and consequences of delayed diagnosis
Emergency Radiology (2021)
-
Clinical features of gingivostomatitis due to primary infection of herpes simplex virus in children
BMC Infectious Diseases (2020)
-
Non-congenital viral infections of the central nervous system: from the immunocompetent to the immunocompromised child
Pediatric Radiology (2020)