Abstract
Objective:
To identify factors associated with responsiveness to dopamine therapy for hypotension and the relationship to brain injury in a cohort of preterm infants.
Study Design:
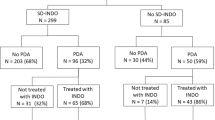
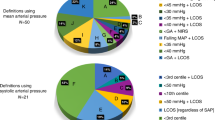
The pharmacy database at St Louis Children’s Hospital was retrospectively queried to identify infants who (a) were born <28 weeks gestation between 2012 and 2014, (b) received dopamine and (c) had blood pressure measurements from an umbilical arterial catheter. A control group was constructed from contemporaneous infants who did not receive dopamine. Mean arterial blood pressure (MABP) at baseline, 1 h and 3 h after initiating dopamine were obtained for each dopamine-exposed infant. MABP measurements at matched time points were obtained in the control group.
Result:
Sixty-nine dopamine-treated and 45 control infants were included. Mean ΔMABP at 3 h was 4.5±6.3 mm of Hg for treated infants vs 1±2.9 for the control. Median dopamine starting dose was 2.5 μg kg−1 min−1. Dopamine-treated infants were less mature and of lower birth weight while also more likely to be intubated at 72 h, diagnosed with intraventricular hemorrhage (IVH) and to die. Failure to respond to dopamine was associated with greater likelihood of developing IVH (odds ratio (OR) 5.8, 95% confidence interval (CI) 1.1–42.3), while a strong response (ΔMABP>10 mm Hg) was associated with a reduction in risk of IVH (OR 0.1, 95% CI 0.01–0.8).
Conclusion:
Low–moderate dose dopamine administration results in modest blood pressure improvements. A lack of response to dopamine is associated with a greater risk of IVH, whereas a strong response is associated with a decreased risk. Further research into underlying mechanisms and management strategies is needed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Zubrow AB, Hulman S, Kushner H, Falkner B . Determinants of blood pressure in infants admitted to neonatal intensive care units: a prospective multicenter study. Philadelphia Neonatal Blood Pressure Study Group. J Perinatol 1995; 15: 470–479.
Cunningham S, Symon AG, Elton RA, Zhu C, McIntosh N . Intra-arterial blood pressure reference ranges, death and morbidity in very low birthweight infants during the first seven days of life. Early Hum Dev 1999; 56: 151–165.
Development of audit measures and guidelines for good practice in the management of neonatal respiratory distress syndrome. Report of a Joint Working Group of the British Association of Perinatal Medicine and the Research Unit of the Royal College of Physicians. Arch Dis Child 1992; 67: 1221–1227.
Bada HS, Korones SB, Perry EH, Arheart KL, Ray JD, Pourcyrous M et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr 1990; 117: 607–614.
Miall-Allen VM, de Vries LS, Whitelaw AG . Mean arterial blood pressure and neonatal cerebral lesions. Arch Dis Child 1987; 62: 1068–1069.
Murphy DJ, Hope PL, Johnson A . Neonatal risk factors for cerebral palsy in very preterm babies: case-control study. BMJ 1997; 314: 404–408.
Seri I, Rudas G, Bors Z, Kanyicska B, Tulassay T . Effects of low-dose dopamine infusion on cardiovascular and renal functions, cerebral blood flow, and plasma catecholamine levels in sick preterm neonates. Pediatr Res 1993; 34: 742–749.
Munro MJ, Walker AM, Barfield CP . Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 2004; 114: 1591–1596.
Børch K, Lou HC, Greisen G . Cerebral white matter blood flow and arterial blood pressure in preterm infants. Acta Paediatr 2010; 99: 1489–1492.
Al-Aweel I, Pursley DM, Rubin LP, Shah B, Weisberger S, Richardson DK . Variations in prevalence of hypotension, hypertension, and vasopressor use in NICUs. J Perinatol 2001; 21: 272–278.
Batton B, Li L, Newman NS, Das A, Watterberg KL, Yoder BA et al. Use of antihypotensive therapies in extremely preterm infants. Pediatrics 2013; 131: e1865–e1873.
Laughon M, Bose C, Allred E, O’Shea TM, Van Marter LJ, Bednarek F et al. Factors associated with treatment for hypotension in extremely low gestational age newborns during the first postnatal week. Pediatrics 2007; 119: 273–280.
Seri I . Cardiovascular, renal, and endocrine actions of dopamine in neonates and children. J Pediatr 1995; 126: 333–344.
Seri I, Tulassay T, Kiszel J, Machay T, Csömör S . Cardiovascular response to dopamine in hypotensive preterm neonates with severe hyaline membrane disease. Eur J Pediatr 1984; 142: 3–9.
Filippi L, Pezzati M, Poggi C, Rossi S, Cecchi A, Santoro C . Dopamine versus dobutamine in very low birthweight infants: endocrine effects. Arch Dis Child Fetal Neonatal Ed 2007; 92: F367–F371.
Hentschel R, Hensel D, Brune T, Rabe H, Jorch G . Impact on blood pressure and intestinal perfusion of dobutamine or dopamine in hypotensive preterm infants. Biol Neonate 1995; 68: 318–324.
Klarr JM, Faix RG, Pryce CJ, Bhatt-Mehta V . Randomized, blind trial of dopamine versus dobutamine for treatment of hypotension in preterm infants with respiratory distress syndrome. J Pediatr 1994; 125: 117–122.
Greenough A, Emery EF . Randomized trial comparing dopamine and dobutamine in preterm infants. Eur J Pediatr 1993; 152: 925–927.
Rozé JC, Tohier C, Maingueneau C, Lefèvre M, Mouzard A . Response to dobutamine and dopamine in the hypotensive very preterm infant. Arch Dis Child 1993; 69: 59–63.
Miall-Allen VM, Whitelaw AG . Response to dopamine and dobutamine in the preterm infant less than 30 weeks gestation. Crit Care Med 1989; 17: 1166–1169.
Pellicer A, Valverde E, Elorza MD, Madero R, Gayá F, Quero J et al. Cardiovascular support for low birth weight infants and cerebral hemodynamics: a randomized, blinded, clinical trial. Pediatrics 2005; 115: 1501–1512.
Valverde E, Pellicer A, Madero R, Elorza D, Quero J, Cabañas F . Dopamine versus epinephrine for cardiovascular support in low birth weight infants: analysis of systemic effects and neonatal clinical outcomes. Pediatrics 2006; 117: e1213–e1222.
Bourchier D, Weston PJ . Randomised trial of dopamine compared with hydrocortisone for the treatment of hypotensive very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 1997; 76: F174–F178.
Gill AB, Weindling AM . Randomised controlled trial of plasma protein fraction versus dopamine in hypotensive very low birthweight infants. Arch Dis Child 1993; 69: 284–287.
Lundstrøm K, Pryds O, Greisen G . The haemodynamic effects of dopamine and volume expansion in sick preterm infants. Early Hum Dev 2000; 57: 157–163.
Cuevas L, Yeh TF, John EG, Cuevas D, Plides RS . The effect of low-dose dopamine infusion on cardiopulmonary and renal status in premature newborns with respiratory distress syndrome. Am J Dis Child 1960 1991; 145: 799–803.
Parry G, Tucker J, Tarnow-Mordi W . CRIB II: an update of the clinical risk index for babies score. Lancet 2003; 361: 1789–1791.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500gm. J Pediatr 1978; 92: 529–534.
Köksal N, Baytan B, Bayram Y, Nacarküçük E . Risk factors for intraventricular haemorrhage in very low birth weight infants. Indian J Pediatr 2002; 69: 561–564.
Ment LR, Oh W, Ehrenkranz RA, Philip AG, Duncan CC, Makuch RW . Antenatal steroids, delivery mode, and intraventricular hemorrhage in preterm infants. Am J Obstet Gynecol 1995; 172: 795–800.
Dani C, Poggi C, Bertini G, Pratesi S, Di Tommaso M, Scarselli G et al. Method of delivery and intraventricular haemorrhage in extremely preterm infants. J Matern Fetal Neonatal Med. 2010; 23: 1419–1423.
Anand K, Hall RW, Desai N, Shephard B, Bergqvist LL, Young TE et al. Effects of morphine analgesia in ventilated preterm neonates: primary outcomes from the NEOPAIN randomised trial. Lancet 2004; 363: 1673–1682.
Lazzara A, Ahmann P, Dykes F, Brann AW, Schwartz J . Clinical predictability of intraventricular hemorrhage in preterm infants. Pediatrics 1980; 65: 30–34.
Vesoulis ZA, Liao SM, Trivedi SB, Ters NE, Mathur AM . A novel method for assessing cerebral autoregulation in preterm infants using transfer function analysis. Pediatr Res 2015 (doi:10.1038/pr.2015.238; e-pub ahead of print).
Soul JS, Hammer PE, Tsuji M, Saul JP, Bassan H, Limperopoulos C et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res 2007; 61: 467–473.
Noori S, McCoy M, Anderson MP, Ramji F, Seri I . Changes in cardiac function and cerebral blood flow in relation to peri/intraventricular hemorrhage in extremely preterm infants. J Pediatr 2014; 164: 264–270.e3.
Wollner L, McCarthy ST, Soper ND, Macy DJ . Failure of cerebral autoregulation as a cause of brain dysfunction in the elderly. Br Med J 1979; 1: 1117–1118.
Watterberg KL, Scott SM . Evidence of early adrenal insufficiency in babies who develop bronchopulmonary dysplasia. Pediatrics 1995; 95: 120–125.
Bajwa N, Berner M, Worley S, Pfister R . Population based age stratified morbidities of premature infants in Switzerland. Swiss Med Wkly 2011; 141: w13212.
Acknowledgements
We thank Brandy Zeller, PharmD and Caren Livisky, PharmD for their assistance in identifying infants using the pharmacy database system and Anthony Barton for his tireless efforts in recruitment and data management. This study was supported by Intellectual and Developmental Disabilities Research Center (IDDRC) at Washington University (NIH/NICHD P30 HD062171), Washington University Institute of Clinical and Translational Sciences KL2 Training Program (NIH/NCATS KL2 TR000450) and The Barnes-Jewish Hospital Foundation and the Washington University Institute of Clinical and Translational Sciences Clinical and Translational Funding Program (NIH/NCATS UL1 TR000448).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Vesoulis, Z., Ters, N., Foster, A. et al. Response to dopamine in prematurity: a biomarker for brain injury?. J Perinatol 36, 453–458 (2016). https://doi.org/10.1038/jp.2016.5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.5
This article is cited by
-
Blood pressure values and hypotension management in extremely preterm infants: a multi-center study
Journal of Perinatology (2022)
-
Divergent risk factors for cerebellar and intraventricular hemorrhage
Journal of Perinatology (2018)