Abstract
Future priorities for the management of hypoxemic respiratory failure (HRF) and pulmonary hypertension include primary prevention of neonatal lung diseases, ‘precision medicine’ and translating promising clinical and preclinical research into novel therapies. Promising areas of investigation include noninvasive ventilation strategies, emerging pulmonary vasodilators (for example, cinaciguat, intravenous bosentan, rho-kinase inhibitors, peroxisome proliferator-activated receptor-γ agonists) and hemodynamic support (arginine vasopressin). Research challenges include the optimal timing for primary prevention interventions and development of validated biomarkers that predict later disease or serve as surrogates for long-term respiratory outcomes. Differentiating respiratory disease endotypes using biomarkers and experimental therapies tailored to the underlying pathobiology are central to the concept of ‘precision medicine’ (that is, prevention and treatment strategies that take individual variability into account). The ideal biomarker should be expressed early in the neonatal course to offer an opportunity for effective and targeted interventions to modify outcomes. The feasibility of this approach will depend on the identification and validation of accurate, rapid and affordable point-of-care biomarker tests. Trials targeting patient-specific pathobiology may involve less risk than traditional randomized controlled trials that enroll all at-risk neonates. Such approaches would reduce trial costs, potentially with fewer negative trials and improved health outcomes. Initiatives such as the Prematurity and Respiratory Outcomes Program, supported by the National Heart, Lung, and Blood Institute, provide a framework to develop refined outcome measures and early biomarkers that will enhance our understanding of novel, mechanistic therapeutic targets that can be tested in clinical trials in neonates with HRF.
Similar content being viewed by others
Introduction
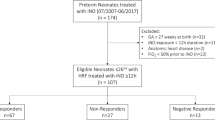
Management strategies for hypoxemic respiratory failure (HRF) and pulmonary hypertension (PH) in the neonate continue to evolve; however, the response to pharmacologic intervention remains suboptimal.1, 2, 3, 4, 5, 6, 7, 8, 9 Challenges to developing evidence-based therapies for HRF and PH in neonates include a broad range of etiologies and disease phenotypes, the lack of early predictors of clinically meaningful long-term outcomes and difficulties in designing and conducting research in this population. This article summarizes the challenges and considerations in carrying out research in HRF and related PH, as well as promising directions and priorities for future research. This article is the conclusion of a series summarizing presentations and discussions from a roundtable discussion focused on HRF in neonates.
Research challenges
Recognizing phenotypes and identifying subpopulations with distinct mechanisms of disease (endotypes) are critical to identifying effective therapies for HRF and PH and reducing exposure to therapies that are not likely to benefit specific patients. For example, one of the more challenging areas of research has been the prevention and treatment of PH associated with severe bronchopulmonary dysplasia (BPD). The development of BPD is influenced by complex and poorly understood interactions between genetic and epigenetic factors and environmental exposures during both antenatal and postnatal periods of development.10 Structurally and biochemically immature lungs, hyperoxia and oxidant injury, volutrauma, inflammation, and poor respiratory drive have all been implicated in the aberrant pulmonary development associated with BPD. Genomic heterogeneity also exists with distinct biologic pathways contributing to the pathogenesis of mild/moderate BPD versus severe disease. It is likely that distinct causal factors dominate in different patients. Failure to identify subpopulations with distinct endotypes can increase exposure to therapies unlikely to benefit individual patients and fuels doubt about biologically plausible therapies that may benefit a subset of at-risk infants.10
The failure to recognize BPD disease endotypes poses a considerable challenge to researchers and contributes to the so-called ‘negative trials.’ These trials, better termed ‘statistically negative trials’ or ‘indeterminate trials,’ cannot prove that a therapy is ineffective.11 Alternate explanations for a ‘negative trial’ include insufficient sample size; small effect size due to failure to optimize the timing, dose or duration of therapy; and poor ‘noise-to-signal ratio’ (that is, excess variation in outcome). The ability of a clinical trial to identify a statistically significant effect is related to the magnitude of the effect of the therapy (‘signal’) and the variation (‘noise’) in the outcome of the study that can be introduced by heterogeneity in patient populations (highly relevant to BPD research), heterogeneous center practices, clinical care and medical co-interventions.11
Strategies to increase the likelihood of a positive trial (assuming the intervention is indeed effective) include increasing the sample size, enhancing the signal and reducing the noise. However, these strategies involve tradeoffs in generalizability, cost, sample size, signal or noise.11 For example, randomized registries or large ‘simple’ trials increase sample size, but registries typically rely on electronic medical record data that are subject to noise while large ‘simple’ trials limit data collection and potentially introduce control noise.11 Adequately powered intervention studies can be complicated by concerns on the part of investigators, institutional review boards and pharmaceutical companies about conducting research in vulnerable populations such as neonates.10
Inherent research challenges in premature infants further complicate the conduct of adequately powered intervention studies. Recruitment of sufficient numbers of appropriate patients with BPD-associated PH, for example, is hindered by the fact that it is a rare condition characterized by substantial phenotypic and endotypic diversity.10 Greater phenotypic and endotypic precision have the potential to enhance the signal–noise ratio; however, the tradeoff is sample size. As endotyping improves, smaller sample sizes should be needed to demonstrate efficacy in targeted populations; however, large multicenter collaborative efforts will be needed to enroll adequate numbers of these highly selected patient populations for sufficiently powered trials.
Optimizing the timing, dose and duration of therapy are obvious strategies to increase the strength of the signal.11 Use of alternative trial designs is another strategy. Adaptive or response-adaptive trial designs, for example, allow investigators to modify the intervention as information from the trial accrues, thereby magnifying the signal. Adaptive designs are increasingly used in oncology trials and there is an historical precedent in neonatology with the randomized ‘play-the-winner’ statistical method or the repeated significance test plan of the sequential analysis described by Armitage.12 The ‘play-the-winner’ strategy was used in early extracorporeal membrane oxygenation trials in neonatal respiratory failure to adapt randomization in favor of the group with improved survival.13 The sequential analysis method was used to compare high-frequency jet ventilation with conventional ventilation in neonates with HRF.14 In this trial, separate sequential analyses (two-sided, α=0.05, power=0.95 to detect 85:15 advantage) were performed for mortality, air leak, BPD, intraventricular hemorrhage and assignment crossover; and a combined analysis was performed, with death overriding other outcome variables. Enrollment was completed when the combined analysis reached the sequential design boundary indicating no treatment difference.14
Other than optimizing the dose and duration of therapy, the most important concept for maximizing treatment effect is targeting the causal pathophysiology of the disease (that is, endotypes are important). Unfortunately, there are gaps in our knowledge that place considerable limits on understanding BPD and other neonatal respiratory diseases. Limited fundamental understanding of the biology of some diseases, such as HRF and specifically BPD, plus the lack of positive examples to guide decisions, limits the adoption of this targeting strategy.
Current definitions of BPD are based on center-specific preferences for oxygen use and oxygen saturation targets. The operational definition of BPD has changed over time based on the ‘requirement’ for supplemental oxygen,15, 16 and more recently, timed room-air challenge in selected infants.17 However, increasing use of respiratory support strategies that administer high or low flow with ambient air or with supplemental oxygen confounds oxygen-based definitions of BPD.18 None of the current definitions of BPD take into account recent changes in management strategies that increasingly involve the use of high-flow nasal cannula systems at the full range of fraction of inspired oxygen (FiO2), including FiO2 of 0.21, or extremely low-flow cannula support (<0.1 Lpm) with FiO2 of 1.0.
Fundamentally, there are inherent shortcomings in defining a disease by its management with no association to the underlying pathophysiology, disease progression or phenotype variability.10 For example, the relevance of an outcome at 36 weeks’ gestational age is problematic as lung development continues beyond term and throughout childhood. A 36-week outcome may result in the ‘misclassification’ of infants whose oxygen need is a reflection of immature control of breathing, immature oral feeding patterns, a compliant chest wall or upper airway structural immaturity, rather than lung pathology. Infants of a lower gestational age remain on support longer and stay in the hospital longer, which undermines the relevance of a 36-week outcome. Definitions based on the need for supplemental oxygen are ill-suited for predicting longer-term outcomes and evaluating the multifactorial nature of BPD. Overall, current operational definitions of BPD lack endotypic insight and fail to quantify disease severity or predict long-term respiratory outcomes.18, 19
It is important to recognize, however, that the key challenge is not only the operational definition of BPD, but also our lack of fundamental understanding of the pathobiology of BPD and other neonatal respiratory diseases. The optimal timing for interventions is unclear.10 There is no consensus regarding whether BPD has its origins in utero, at the time of delivery or in the early postnatal period. The timing of BPD initiation may be different in each neonate, varying with gestational age and other maternal and fetal or neonatal characteristics. For instance, BPD may have an antenatal origin in a 23-week gestation infant exposed to preterm labor and chorioamnionitis, but a postnatal onset in a 33-week gestation infant exposed to high mechanical ventilator settings. Both infants may have genetic components that predispose to or modify the disease. Nor is it known how interactions between antenatal exposures and postnatal events modulate the risk or severity of BPD. Our understanding of how various BPD phenotypes evolve over time is also incomplete. The lack of validated biomarkers that predict later disease and can serve as surrogates for long-term respiratory outcomes poses additional challenges to research and therapeutic advances. In addition, there is a great need for comprehensive genomic analysis of existing and future BPD cohorts to identify genetic modifiers of the disease. This approach could lead to partnerships in the pharmaceutical industry that may provide ‘precision’ therapies that will benefit some infants with specific genetic etiologies. Efforts to overcome such challenges include the prospective multicenter Prematurity and Respiratory Outcomes Program (PROP), supported by the National Heart, Blood, and Lung Institute (NHLBI), which will provide a highly granular description of outcomes both at the time of discharge from the neonatal intensive care units and throughout the first year of life, as well as a comprehensive biorepository for identification of biomarkers and genetic causes.18, 20, 21 Databases and cohorts such as PROP should be combined and harmonized with those from other collaborations and countries to accelerate discovery.
Future priorities
To optimize outcomes in neonates at risk for lung diseases, future priorities should focus on primary prevention, emerging approaches (for example, ‘precision medicine’) and translating promising clinical and preclinical research into novel therapies. A recent NHLBI workshop highlighted promising areas for research, including an understanding of normal and aberrant lung development, distinguishing BPD endotypes and determining biomarkers for targeted therapeutic approaches.10 The workshop also identified research priorities that included a recommendation to validate sensitive and specific early ‘omic’ signatures to differentiate BPD endotypes and adopt study designs that integrate personalized medicine using biomarkers and experimental therapies tailored to the underlying pathobiology.10
Identification of biomarkers
Identification of validated biomarkers of disease will facilitate the development of tailored personalized therapeutic approaches22 while reducing healthcare costs and the risks associated with broadly applying ineffective and potentially dangerous and costly therapies. Improved patient endotyping with the use of biomarkers prior to randomization may enhance safety and efficacy of randomized controlled trials of novel therapies. The downside would be increased screening costs, which may result in fewer eligible patients and require more collaborative efforts among centers.
To ensure the broadest adoption and greatest clinical impact, biomarkers in BPD and HRF should be practical, affordable and predictive of later disease. They may also serve as surrogates for the long-term respiratory outcomes that are most important to patients and the healthcare system. Validation of a biomarker in replication cohorts is a prerequisite for widespread acceptance; however, there are several challenges to the development of biomarkers for long-term respiratory disease outcomes. Both DNA and microRNA, for example, can provide information about genetic predisposition or resilience factors in lung disease, but it is unknown which is the most useful or even which samples should be collected (for example, amniotic fluid, tracheal aspirate, blood, urine or stool). Normalization of biomarker values represents another challenge. For instance, using urine creatinine as the denominator of a urine biomarker in neonates drastically increases the noise-to-signal ratio because of the wide range and typically very low values of normal creatinine in newborns. Another challenge for biomarker discovery is the presence of multiple confounders and identification of an appropriate control group—this is particularly challenging in very preterm neonates who may or may not develop BPD.
In choosing a biomarker, there are statistical and methodological issues to be addressed a priori, such as the use of absolute values at a single time point versus values that change over time. It may be that the pattern of change in a particular biomarker over time rather than its absolute value is most predictive of long-term respiratory outcomes.18, 20 Interactions between various biomarkers, such as the balance between inflammatory and anti-inflammatory biomarkers or oxidant versus antioxidant capacity, must also be integrated into study designs and the selection of biomarkers. Measuring inflammatory biomarkers alone may be of little predictive value, for instance, but the balance of inflammatory and anti-inflammatory cytokines (or oxidant versus antioxidant capacity) may be prognostic.
Government-supported research organizations have proposed initiatives to promote creative new approaches for detecting, measuring and analyzing a wide range of biomedical information including molecular, genomic, cellular, clinical and environmental parameters. ‘Translational bioinformatics,’ which aim to link and generate insights from clinical and genetic databases and apply those data to clinical care, is a powerful tool that can generate new biomedical knowledge relevant to neonatal care.23 Incorporation of knowledge derived from these data into clinical practice via electronic medical records and other means can promote prospective evaluation of its impact on patient outcomes and facilitate delivery of personalized, precision medicine.
Novel and emerging treatment strategies
Translational bioinformatics and other techniques have the potential to translate promising clinical and preclinical research into novel HRF and PH therapies in the clinical setting. Innovative lung recruitment strategies and ventilatory approaches such as airway pressure release ventilation or ‘BiVent’ and neurally adjusted ventilatory assist, pulmonary vasodilators, and hemodynamic support are among the novel approaches deserving further study. Greater insight into the pathobiology of chronic pulmonary vascular disease in infants has led to the consideration of novel pharmacologic treatment and prevention approaches. Although these signaling pathways and medications are investigational at this time, they do provide a glimpse into current research and potential future approaches.
One therapeutic approach stems from our expanded understanding of the contribution of nitric oxide (NO) signaling to the pathogenesis of PH. A growing body of evidence suggests that disrupted L-citrulline–L-arginine–NO signaling is involved in the pathogenesis of chronic hypoxia-induced PH in newborns.24, 25 Hypoxia reduces NO production in pulmonary arterial endothelial cells (PAECs) by uncoupling endothelial NO synthase, which is responsible for synthesizing NO from L-arginine.24 L-arginine supplementation can improve NO signaling and, thereby, ameliorate chronic PH; oral citrulline may be more effective than arginine in increasing serum L-arginine concentrations and represents an alternate means for improving NO signaling.26, 27
Putative mechanisms by which L-citrulline improves NO signaling are via recoupling of endothelial NO synthase, reducing superoxide generation and enhancing NO synthesis as shown in hypoxic PAECs and in chronic hypoxia-induced PH in animal models.24 In newborn piglets, L-citrulline ameliorated chronic hypoxia-induced PH and increased NO production in animals exposed to chronic hypoxia.28 Pulmonary arterial pressure and pulmonary vascular resistance were significantly lower in hypoxic animals treated with L-citrulline than in untreated hypoxic animals (P<0.001). In vivo exhaled NO production (P=0.03) and nitrite/nitrate accumulation in the perfusate of isolated lungs (P=0.04) were significantly higher in L-citrulline-treated hypoxic piglets compared with untreated hypoxic animals. Another in vivo study demonstrated that L-citrulline administered subcutaneously attenuates arrested alveolar growth and PH in experimental oxygen-induced BPD in newborn rats.29 L-citrulline preserved alveolar and vascular growth in oxygen-exposed rat pups and decreased pulmonary arterial medial wall thickness and right ventricular hypertrophy. Together, these findings suggest that supplementation with L-citrulline or L-arginine may represent a novel therapeutic approach to ameliorate PH and prevent BPD in neonates.
Endothelin (ET) receptor blockers have historically been used as rescue therapy late in the treatment course in infants with severe established PH rather than as a pulmonary vasodilator early in the course in infants at risk for the development of chronic PH. Given the importance of elevated ET levels in the pathophysiology of congenital diaphragmatic hernia (CDH)30 and other neonatal respiratory conditions associated with PH, investigation of the potential therapeutic efficacy of intravenous bosentan (a non-specific ET-1 receptor blocker) may be warranted as potential primary therapy from birth in neonates with CDH, prior to the development of established PH.
Rho-kinase (ROCK) is another important signaling pathway that regulates vascular tone and myogenic reactivity, and contributes to hypertensive vascular remodeling in experimental models.31, 32, 33, 34, 35 Interestingly, ROCK inhibitors have been shown to be effective in the setting of decreased endothelial NO synthase. In animal models of genetically reduced endothelial NO production (endothelial NO synthase knockout mice and spontaneously hypertensive rats) and pharmacologically reduced endogenous NO production, ROCK inhibition produces a strong vasodilator response.36, 37 In a fetal sheep model of experimental persistent PH of newborn (PPHN), ROCK inhibition increased left pulmonary artery blood flow and decreased pulmonary vascular resistance by 25% both in fetal and neonatal lambs.33 After birth, the same effect was seen with ROCK inhibition. Notably, the effects of ET-1 on pulmonary artery endothelial cell function are mediated by ROCK, and blocking the pathway may be a novel approach to managing PH associated with high ET levels.38, 39
Peroxisome proliferator-activated receptor-γ (PPARγ) agonists produce vasodilation through the inhibition of ROCK; thus, both ROCK and PPARγ regulate smooth muscle cell proliferation and contribute to vascular remodeling in adult PH.40 During fetal life, PPARγ is present at constant levels in the lung, but tends to decrease as the fetus transitions to a newborn and then into adulthood. In experimental models of PH and lung injury, activation of PPARγ prevents PH and reduces lung injury.41, 42 In PPHN, PAEC dysfunction contributes to impaired angiogenesis. In vitro studies of isolated PAECs demonstrate that ET-1 decreases PPARγ protein expression and activity, and impairs endothelial cell function. Administering PPARγ agonists in that setting restores PAEC function. Although these studies demonstrate a potential role for PPARγ agonists in the treatment of PH, experience with adult patients raises concern about toxicity, which may limit translation to clinical use.
Impaired NO-cyclic guanosine monophosphate (cGMP) signaling with decreased soluble guanylate cyclase (sGC) activity contributes to severe PH post birth.43 In the presence of increased reactive oxygen species, sGC becomes oxidized, decreasing the ability to produce cGMP-mediated dilation. A study of the effects of cinaciguat, an sGC activator that is effective in the setting of oxidized sGC, found cinaciguat-induced pulmonary vasodilation in fetal lambs with PPHN induced by in utero ductus arteriosus ligation. Pulmonary vascular resistance was reduced by 36% (P<0.001).44 Importantly, the pulmonary vascular response to cinaciguat was greater than the effects of increased oxygen and inhaled nitric oxide alone. The effects of cinaciguat on enhanced cGMP production in pulmonary artery smooth muscle cells from normal fetal sheep and from sheep with chronic intrauterine PH were greater under hyperoxic conditions (FiO2 50%) compared with its effects in room air. It is particularly encouraging that cinaciguat increased cGMP production in the presence of hyperoxia in both normal and PPHN pulmonary artery smooth muscle cells. This suggests that in the presence of oxidized sGC, cinaciguat may still be effective in increasing cGMP production and vasodilation. Thus, cinaciguat may provide a novel treatment option for severe PH.
Additional strategies could emerge from improved understanding of the role of oxidant stress in PH. The use of intratracheal recombinant human superoxide dismutase acutely induces pulmonary vasodilation, improves oxygenation and decreases oxidative stress in lambs with PPHN.45 Oxidant stress selectively induces the phosphodiesterase type 5 enzyme and oxidizes sGC, resulting in the breakdown of cGMP. In addition to sildenafil, newer long-acting phosphodiesterase type 5 inhibitors, such as tadalafil, appear to be effective in animal models of PPHN.46 Additional insights will likely be gained from a better understanding of the generation of reactive oxygen species from specific subcellular compartments.
Altered hemodynamics contribute to adverse outcomes in PPHN, and limited success with current vasoactive therapies, such as dopamine and epinephrine, has generated interest in novel regulators of systemic vascular tone. Arginine vasopressin is a vasopressor agent that acts through arginine vasopressin 1A receptors on the smooth muscle cells in the systemic circulation to produce vasoconstriction. Vasopressin is increasingly used in some centers to support infants with PPHN and hemodynamic instability, especially in the setting of CDH. The strength of this compound is its ability to produce non-catecholamine-dependent vasoconstriction. Thus, vasopressin can be effective in the setting of catecholamine resistance. Intriguingly, in infants with CDH and refractory hypotension, vasopressin improved systemic hemodynamics and gas exchange without adverse effects on pulmonary vascular resistance and was associated with a trend towards a decrease in the pulmonary to systemic pressure ratio.47 These results suggest a potential role for vasopressin therapy in patients with CDH with catecholamine-resistant refractory hypotension.
Conclusions
In summary, the recognition of phenotypes and identification of subpopulations with distinct mechanisms of disease (endotypes) are critical to finding safe and efficacious therapies for HRF and PH, and reducing exposure to therapies not likely to benefit certain patients. As such, identification of biomarker-driven BPD endotypes holds promise for a new era of research in the prevention of BPD and HRF. Use of validated biomarkers to guide treatment for distinct study populations should prove less risky and costly than traditional randomized controlled trials that enroll all infants deemed at risk. This ultimately should reduce the costs of clinical care with the hope of improved outcomes. Future research priorities should focus on primary prevention of neonatal lung diseases, emerging approaches (for example, ‘precision medicine’) and translating promising clinical and preclinical research into novel therapies. Novel areas of investigation include pulmonary vasodilators, including intravenous bosentan and emerging agents (citrulline, cinaciguat, ROCK inhibitors, PPARγ agonists), and hemodynamic support (arginine vasopressin). Multicenter randomized trials are needed to evaluate the efficacy of novel therapies in the setting of neonatal HRF and PH.
References
Roberts JD Jr, Fineman JR, Morin FC III, Shaul PW, Rimar S, Schreiber MD et al. Inhaled nitric oxide and persistent pulmonary hypertension of the newborn. The Inhaled Nitric Oxide Study Group. N Engl J Med 1997; 336: 605–610.
Inhaled nitric oxide and hypoxic respiratory failure in infants with congenital diaphragmatic hernia. The Neonatal Inhaled Nitric Oxide Study Group (NINOS). Pediatrics 1997; 99: 838–845.
Clark RH, Kueser TJ, Walker MW, Southgate WM, Huckaby JL, Perez JA et al. Low-dose nitric oxide therapy for persistent pulmonary hypertension of the newborn. Clinical Inhaled Nitric Oxide Research Group. N Engl J Med 2000; 342: 469–474.
Early compared with delayed inhaled nitric oxide in moderately hypoxaemic neonates with respiratory failure: a randomised controlled trial. The Franco-Belgium Collaborative NO Trial Group. Lancet 1999; 354: 1066–1071.
Gonzalez A, Fabres J, D'Apremont I, Urcelay G, Avaca M, Gandolfi C et al. Randomized controlled trial of early compared with delayed use of inhaled nitric oxide in newborns with a moderate respiratory failure and pulmonary hypertension. J Perinatol 2010; 30: 420–424.
Konduri GG, Solimano A, Sokol GM, Singer J, Ehrenkranz RA, Singhal N et al. A randomized trial of early versus standard inhaled nitric oxide therapy in term and near-term newborn infants with hypoxic respiratory failure. Pediatrics 2004; 113: 559–564.
Konduri GG, Sokol GM, Van Meurs KP, Singer J, Ambalavanan N, Lee T et al. Impact of early surfactant and inhaled nitric oxide therapies on outcomes in term/late preterm neonates with moderate hypoxic respiratory failure. J Perinatol 2013; 33: 944–949.
Findlay RD, Taeusch HW, Walther FJ . Surfactant replacement therapy for meconium aspiration syndrome. Pediatrics 1996; 97: 48–52.
Lotze A, Mitchell BR, Bulas DI, Zola EM, Shalwitz RA, Gunkel JH . Multicenter study of surfactant (beractant) use in the treatment of term infants with severe respiratory failure. Survanta in Term Infants Study Group. J Pediatr 1998; 132: 40–47.
McEvoy CT, Jain L, Schmidt B, Abman S, Bancalari E, Aschner JL . Bronchopulmonary dysplasia: NHLBI Workshop on the Primary Prevention of Chronic Lung Diseases. Ann Am Thorac Soc 2014; 11 Suppl 3: S146–S153.
Rubenfeld GD . Confronting the frustrations of negative clinical trials in acute respiratory distress syndrome. Ann Am Thorac Soc 2015; 12 Suppl 1: S58–S63.
Armitage P . Sequential Medical Trials, 2nd ed. New York, USA: John Wiley & Sons, 1975.
Bartlett RH, Roloff DW, Cornell RG, Andrews AF, Dillon PW, Zwischenberger JB . Extracorporeal circulation in neonatal respiratory failure: a prospective randomized study. Pediatrics 1985; 76: 479–487.
Carlo WA, Siner B, Chatburn RL, Robertson S, Martin RJ . Early randomized intervention with high-frequency jet ventilation in respiratory distress syndrome. J Pediatr 1990; 117: 765–770.
Shennan AT, Dunn MS, Ohlsson A, Lennox K, Hoskins EM . Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 1988; 82: 527–532.
Jobe AH, Bancalari E . Bronchopulmonary dysplasia. Am J Respir Crit Care Med 2001; 163: 1723–1729.
Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics 2004; 114: 1305–1311.
Maitre NL, Ballard RA, Ellenberg JH, Davis SD, Greenberg JM, Hamvas A et al. Respiratory consequences of prematurity: evolution of a diagnosis and development of a comprehensive approach. J Perinatol 2015; 35: 313–321.
Poindexter BB, Feng R, Schmidt B, Aschner JL, Ballard RA, Hamvas A et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann Am Thorac Soc 2015; 12: 1822–1830.
Pryhuber GS, Maitre NL, Ballard RA, Cifelli D, Davis SD, Ellenberg JH et al. Prematurity and respiratory outcomes program (PROP): study protocol of a prospective multicenter study of respiratory outcomes of preterm infants in the United States. BMC Pediatr 2015; 15: 37.
University of Pennsylvania; National Heart, Lung, and Blood Institute. Prematurity and Respiratory Outcomes Program (PROP). In: Clinicaltrials.gov [Internet]. Bethesda (MD): National Library of Medicine (US), 2011 [cited 2 Dec 2015]. Available from https://www.clinicaltrials.gov/ct2/show/NCT01435187?term=NCT01435187&rank=1 NLM. Identifier: NCT01435187.
Collins FS, Varmus H . A new initiative on precision medicine. N Engl J Med 2015; 372: 793–795.
Palma JP, Benitz WE, Tarczy-Hornoch P, Butte AJ, Longhurst CA . Neonatal informatics: transforming neonatal care through translational bioinformatics. Neoreviews 2012; 13: e281–e284.
Fike CD, Summar M, Aschner JL . L-citrulline provides a novel strategy for treating chronic pulmonary hypertension in newborn infants. Acta Paediatr 2014; 103: 1019–1026.
Fike CD, Dikalova A, Kaplowitz MR, Cunningham G, Summar M, Aschner JL . Rescue treatment with L-citrulline inhibits hypoxia-induced pulmonary hypertension in newborn pigs. Am J Respir Cell Mol Biol 2015; 53: 255–264.
Erez A, Nagamani SC, Shchelochkov OA, Premkumar MH, Campeau PM, Chen Y et al. Requirement of argininosuccinate lyase for systemic nitric oxide production. Nat Med 2011; 17: 1619–1626.
Schwedhelm E, Maas R, Freese R, Jung D, Lukacs Z, Jambrecina A et al. Pharmacokinetic and pharmacodynamic properties of oral L-citrulline and L-arginine: impact on nitric oxide metabolism. Br J Clin Pharmacol 2008; 65: 51–59.
Ananthakrishnan M, Barr FE, Summar ML, Smith HA, Kaplowitz M, Cunningham G et al. L-citrulline ameliorates chronic hypoxia-induced pulmonary hypertension in newborn piglets. Am J Physiol Lung Cell Mol Physiol 2009; 297: L506–L511.
Vadivel A, Aschner JL, Rey-Parra GJ, Magarik J, Zeng H, Summar M et al. L-citrulline attenuates arrested alveolar growth and pulmonary hypertension in oxygen-induced lung injury in newborn rats. Pediatr Res 2010; 68: 519–525.
Keller RL, Tacy TA, Hendricks-Munoz K, Xu J, Moon-Grady AJ, Neuhaus J et al. Congenital diaphragmatic hernia: endothelin-1, pulmonary hypertension, and disease severity. Am J Respir Crit Care Med 2010; 182: 555–561.
Büssemaker E, Pistrosch F, Förster S, Herbrig K, Gross P, Passauer J et al. Rho kinase contributes to basal vascular tone in humans: role of endothelium-derived nitric oxide. Am J Physiol Heart Circ Physiol 2007; 293: H541–H547.
Chapados R, Abe K, Ihida-Stansbury K, McKean D, Gates AT, Kern M et al. ROCK controls matrix synthesis in vascular smooth muscle cells: coupling vasoconstriction to vascular remodeling. Circ Res 2006; 99: 837–844.
Parker TA, Roe G, Grover TR, Abman SH . Rho kinase activation maintains high pulmonary vascular resistance in the ovine fetal lung. Am J Physiol Lung Cell Mol Physiol 2006; 291: L976–L982.
Wang Z, Jin N, Ganguli S, Swartz DR, Li L, Rhoades RA . Rho-kinase activation is involved in hypoxia-induced pulmonary vasoconstriction. Am J Respir Cell Mol Biol 2001; 25: 628–635.
Oka M, Homma N, Taraseviciene-Stewart L, Morris KG, Kraskauskas D, Burns N et al. Rho kinase-mediated vasoconstriction is important in severe occlusive pulmonary arterial hypertension in rats. Circ Res 2007; 100: 923–929.
Löhn M, Steioff K, Bleich M, Busch AE, Ivashchenko Y . Inhibition of Rho-kinase stimulates nitric oxide-independent vasorelaxation. Eur J Pharmacol 2005; 507: 179–186.
Abe K, Tawara S, Oi K, Hizume T, Uwatoku T, Fukumoto Y et al. Long-term inhibition of Rho-kinase ameliorates hypoxia-induced pulmonary hypertension in mice. J Cardiovasc Pharmacol 2006; 48: 280–285.
Homma N, Nagaoka T, Morio Y, Ota H, Gebb SA, Karoor V et al. Endothelin-1 and serotonin are involved in activation of RhoA/Rho kinase signaling in the chronically hypoxic hypertensive rat pulmonary circulation. J Cardiovasc Pharmacol 2007; 50: 697–702.
Gien J, Tseng N, Seedorf G, Roe G, Abman SH . Endothelin-1 impairs angiogenesis in vitro through Rho-kinase activation after chronic intrauterine pulmonary hypertension in fetal sheep. Pediatr Res 2013; 73: 252–262.
Gien J, Tseng N, Seedorf G, Roe G, Abman SH . Peroxisome proliferator activated receptor-gamma-Rho-kinase interactions contribute to vascular remodeling after chronic intrauterine pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 2014; 306: L299–L308.
Dasgupta C, Sakurai R, Wang Y, Guo P, Ambalavanan N, Torday JS et al. Hyperoxia-induced neonatal rat lung injury involves activation of TGF-{beta} and Wnt signaling and is protected by rosiglitazone. Am J Physiol Lung Cell Mol Physiol 2009; 296: L1031–L1041.
Nicola T, Ambalavanan N, Zhang W, James ML, Rehan V, Halloran B et al. Hypoxia-induced inhibition of lung development is attenuated by the peroxisome proliferator-activated receptor-gamma agonist rosiglitazone. Am J Physiol Lung Cell Mol Physiol 2011; 301: L125–L134.
Steinhorn RH, Russell JA, Morin FC III . Disruption of cGMP production in pulmonary arteries isolated from fetal lambs with pulmonary hypertension. Am J Physiol 1995; 268: H1483–H1489.
Chester M, Seedorf G, Tourneux P, Gien J, Tseng N, Grover T et al. Cinaciguat, a soluble guanylate cyclase activator, augments cGMP after oxidative stress and causes pulmonary vasodilation in neonatal pulmonary hypertension. Am J Physiol Lung Cell Mol Physiol 2011; 301: L755–L764.
Lakshminrusimha S, Russell JA, Wedgwood S, Gugino SF, Kazzaz JA, Davis JM et al. Superoxide dismutase improves oxygenation and reduces oxidation in neonatal pulmonary hypertension. Am J Respir Crit Care Med 2006; 174: 1370–1377.
Tessler RB, Zadinello M, Fiori H, Colvero M, Belik J, Fiori RM . Tadalafil improves oxygenation in a model of newborn pulmonary hypertension. Pediatr Crit Care Med 2008; 9: 330–332.
Acker SN, Kinsella JP, Abman SH, Gien J . Vasopressin improves hemodynamic status in infants with congenital diaphragmatic hernia. J Pediatr 2014; 165: 53–58.
Acknowledgements
This article is based on discussions at a roundtable meeting supported by a grant from Mallinckrodt Pharmaceuticals, formerly Ikaria. Presentations and discussions were developed solely by the participants, without grantor input. The meeting chair (RHS) determined the agenda and attendees. JLA, JG, NA, JPK, GGK, SL, ODS and RHS developed the presentations and led the discussions upon which this article is based. Participants provided critical review and revisions to the outline and manuscript drafts, provided final approval of the version to be published, and are accountable for the integrity of the content and for addressing questions. Writing and editorial assistance was provided by John Kross, and Sharon Suntag and Julie Gerke of Quintiles.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
JLA, JG, NA, JPK, GGK, SL, ODS and RHS received honoraria for their participation in a roundtable meeting supported by a grant from Mallinckrodt Pharmaceuticals, formerly Ikaria. JLA is named on an intellectual property rights patent for the use of intravenous citrulline for neonatal lung diseases. NA has received research support from Pfizer and has received research support as a mentor from Ikaria. GGK has received consulting fees from Boston Health Economics and Actelion Clinical Research. SL was a member of the speaker’s bureau for Ikaria from June 2010 to October 2014 and has received grant support from the American Academy of Pediatrics and Canadian Pediatric Society. RHS has received research grant support from Pfizer. NIH Grants: 1U01HL101456 (JLA); U01 HL122626 and R01 HD067126 (NA); 5R01HD072929-03 (SL); 5R01HL057268-11 (GGK); 5R01HL054705-13 (RHS).
Rights and permissions
About this article
Cite this article
Aschner, J., Gien, J., Ambalavanan, N. et al. Challenges, priorities and novel therapies for hypoxemic respiratory failure and pulmonary hypertension in the neonate. J Perinatol 36 (Suppl 2), S32–S36 (2016). https://doi.org/10.1038/jp.2016.47
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.47
This article is cited by
-
Cost-effectiveness analysis of pulse oximetry screening for critical congenital heart defects following homebirth and early discharge
European Journal of Pediatrics (2019)