Abstract
Objective:
The objective of the study was to examine normal variations of umbilical cord arterial pH by gestational age (GA).
Study Design:
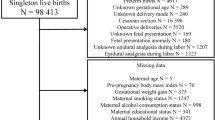
Population-based cohort study of 46 199 infants born from 2008 to 2014 in Stockholm, Sweden, with GA 28 to 42 weeks, Apgar score ⩾7 at 5 min, non-instrumental vaginal delivery, and birth weight for GA⩾3rd and ⩽97th percentile. Quantile regression was used to investigate the associations between GA and infant sex, and pH.
Results:
The mean umbilical cord arterial pH (s.d.) was 7.29 (0.10), 7.27 (0.07), 7.25 (0.07) and 7.23 (0.07) among infants born at 28 to 31, 32 to 36, 37 to 41 and 42 weeks, respectively. Arterial pH decreased linearly with increasing GA, and female infants had higher pH than male infants (P<0.001).
Conclusion:
Umbilical cord arterial pH varied in a linear fashion by GA and was influenced by infant sex. The provided reference curve taking GA into account may yield a more accurate definition of acidosis at birth.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Armstrong L, Stenson BJ . Use of umbilical cord blood gas analysis in the assessment of the newborn. Arch Dis Child Fetal Neonatal Ed 2007; 92 (6): F430–F434.
Malin GL, Morris RK, Khan KS . Strength of association between umbilical cord pH and perinatal and long term outcomes: systematic review and meta-analysis. BMJ 2010; 340: c1471.
Yeh P, Emary K, Impey L . The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51,519 consecutive validated samples. BJOG 2012; 119 (7): 824–831.
Thorp JA, Dildy GA, Yeomans ER, Meyer BA, Parisi VM . Umbilical cord blood gas analysis at delivery. Am J Obstet Gynecol 1996; 175 (3 Pt 1): 517–522.
Helwig JT, Parer JT, Kilpatrick SJ, Laros RK Jr. . Umbilical cord blood acid-base state: what is normal? Am J Obstet Gynecol 1996; 174 (6): 1807–1812; discussion 1812-1804.
Gilstrap LC 3rd, Leveno KJ, Burris J, Williams ML, Little BB . Diagnosis of birth asphyxia on the basis of fetal pH, Apgar score, and newborn cerebral dysfunction. Am J Obstet Gynecol 1989; 161 (3): 825–830.
Hafstrom M, Ehnberg S, Blad S, Noren H, Renman C, Rosen KG et al. Developmental outcome at 6.5 years after acidosis in term newborns: a population-based study. Pediatrics 2012; 129 (6): e1501–e1507.
Kitlinski ML, Kallen K, Marsal K, Olofsson P . Gestational age-dependent reference values for pH in umbilical cord arterial blood at term. Obstet Gynecol 2003; 102 (2): 338–345.
Knutzen L, Svirko E, Impey L . The significance of base deficit in acidemic term neonates. Am J Obstet Gynecol 2015; 213 (3): 373 e371–373 e377.
White CR, Doherty DA, Kohan R, Newnham JP, Pennell CE . Evaluation of selection criteria for validating paired umbilical cord blood gas samples: an observational study. BJOG 2012; 119 (7): 857–865.
Marsal K, Persson PH, Larsen T, Lilja H, Selbing A, Sultan B . Intrauterine growth curves based on ultrasonically estimated foetal weights. Acta Paediatr 1996; 85 (7): 843–848.
Hankins GD, Speer M . Defining the pathogenesis and pathophysiology of neonatal encephalopathy and cerebral palsy. Obstet Gynecol 2003; 102 (3): 628–636.
Victory R, Penava D, Da Silva O, Natale R, Richardson B . Umbilical cord pH and base excess values in relation to adverse outcome events for infants delivering at term. Am J Obstet Gynecol 2004; 191 (6): 2021–2028.
Executive summary: Neonatal encephalopathy and neurologic outcome, second edition. Report of the American College of Obstetricians and Gynecologists' Task Force on Neonatal Encephalopathy. Obstet Gynecol 2014; 123 (4): 896–901.
Herbst A, Wolner-Hanssen P, Ingemarsson I . Risk factors for acidemia at birth. Obstet Gynecol 1997; 90 (1): 125–130.
Nicolaides KH, Economides DL, Soothill PW . Blood gases, pH, and lactate in appropriate- and small-for-gestational-age fetuses. Am J Obstet Gynecol 1989; 161 (4): 996–1001.
Wiberg N, Kallen K, Herbst A, Olofsson P . Relation between umbilical cord blood pH, base deficit, lactate, 5-minute Apgar score and development of hypoxic ischemic encephalopathy. Acta Obstet Gynecol Scand 2010; 89 (10): 1263–1269.
Wiberg N, Kallen K, Olofsson P . Physiological development of a mixed metabolic and respiratory umbilical cord blood acidemia with advancing gestational age. Early Hum Dev 2006; 82 (9): 583–589.
Forhead AJ, Fowden AL . Thyroid hormones in fetal growth and prepartum maturation. J Endocrinol 2014; 221 (3): R87–R103.
Fyfe KL, Yiallourou SR, Wong FY, Horne RS . The development of cardiovascular and cerebral vascular control in preterm infants. Sleep Med Rev 2014; 18 (4): 299–310.
Soothill PW, Nicolaides KH, Rodeck CH, Campbell S . Effect of gestational age on fetal and intervillous blood gas and acid-base values in human pregnancy. Fetal Ther 1986; 1 (4): 168–175.
Gregg AR, Weiner CP . ‘Normal’ umbilical arterial and venous acid-base and blood gas values. Clin Obstet Gynecol 1993; 36 (1): 24–32.
Nava S, Bocconi L, Zuliani G, Kustermann A, Nicolini U . Aspects of fetal physiology from 18 to 37 weeks' gestation as assessed by blood sampling. Obstet Gynecol 1996; 87 (6): 975–980.
Ramin SM, Gilstrap LC 3rd, Leveno KJ, Burris J, Little BB . Umbilical artery acid-base status in the preterm infant. Obstet Gynecol 1989; 74 (2): 256–258.
Dickinson JE, Eriksen NL, Meyer BA, Parisi VM . The effect of preterm birth on umbilical cord blood gases. Obstet Gynecol 1992; 79 (4): 575–578.
Chanrachakul B, Chua S, Nordstrom L, Yam J, Arulkumaran S . Umbilical artery blood gas and lactate in healthy newborns. J Med Assoc Thai 1999; 82 (4): 388–393.
Rose J, Butler EE, Lamont LE, Barnes PD, Atlas SW, Stevenson DK . Neonatal brain structure on MRI and diffusion tensor imaging, sex, and neurodevelopment in very-low-birthweight preterm children. Dev Med Child Neurol 2009; 51 (7): 526–535.
Kent AL, Wright IM, Abdel-Latif ME . Mortality and adverse neurologic outcomes are greater in preterm male infants. Pediatrics 2012; 129 (1): 124–131.
Skiold B, Alexandrou G, Padilla N, Blennow M, Vollmer B, Aden U . Sex differences in outcome and associations with neonatal brain morphology in extremely preterm children. J Pediatr 2014; 164 (5): 1012–1018.
Clifton VL . Review: sex and the human placenta: mediating differential strategies of fetal growth and survival. Placenta 2010; 31 Suppl: S33–S39.
Fellman V, Hellstrom-Westas L, Norman M, Westgren M, Kallen K, Lagercrantz H et al. One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA 2009; 301 (21): 2225–2233.
Apgar V . A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg 1953; 32 (4): 260–267.
Wiberg N, Kallen K, Olofsson P . Delayed umbilical cord clamping at birth has effects on arterial and venous blood gases and lactate concentrations. BJOG 2008; 115 (6): 697–703.
Westgate J, Garibaldi JM, Greene KR . Umbilical cord blood gas analysis at delivery: a time for quality data. Br J Obstet Gynaecol 1994; 101 (12): 1054–1063.
Acknowledgements
Professor Sven Cnattingius initiated and conceptualized the research database, and is responsible for the database infrastructure. The work was supported by the Stockholm County Council (ALF 20130156, 20140105, 20150118 and post-doctoral financial support); and the Swedish Research Council (2013–2429). The funders had no involvement in study design, collection, analysis, and/or interpretation of data, writing of the report or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Skiöld, B., Petersson, G., Ahlberg, M. et al. Population-based reference curve for umbilical cord arterial pH in infants born at 28 to 42 weeks. J Perinatol 37, 254–259 (2017). https://doi.org/10.1038/jp.2016.207
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2016.207
This article is cited by
-
Maternal overweight and obesity increase the risk of fetal acidosis during labor
Journal of Perinatology (2018)