Abstract
Objective:
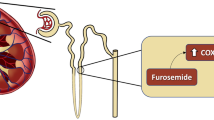
To determine whether platelet counts can predict the likelihood of successful closure of patent ductus arteriosus (PDA) with indomethacin.
Study Design:
This was a retrospective cohort study of infants <32 weeks’ gestational age (GA) and birth weight <1500 g with PDA. Clinical characteristics between infants who achieved ductal closure with indomethacin and those who failed were compared. Multivariable logistic regression was used to identify predictors of successful ductal closure.
Results:
In infants with hemodynamically significant PDA, older GA (odds ratio=1.54; 95% confidence interval: 1.12 to 2.13), male gender (odds ratio=3.02; 95% confidence interval: 1.08 to 8.49) and higher platelet count (odds ratio=1.5; 95% confidence interval: 1.04 to 2.17) prior to indomethacin treatment were associated with successful ductal closure with indomethacin.
Conclusion:
Older GA, male gender and higher platelet count at time of treatment of hemodynamically significant PDA are predictors of successful ductal closure with indomethacin.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
The Vermont-Oxford Trials Network: very low birth weight outcomes for 1990. Investigators of the Vermont-Oxford Trials Network Database Project. Pediatrics 1993; 91 (3): 540–545.
Koch J, Hensley G, Roy L, Brown S, Ramaciotti C, Rosenfeld CR . Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics 2006; 117 (4): 1113–1121.
Hamrick SE, Hansmann G . Patent ductus arteriosus of the preterm infant. Pediatrics 2010; 125 (5): 1020–1030.
Noori S, McCoy M, Friedlich P, Bright B, Gottipati V, Seri I et al. Failure of ductus arteriosus closure is associated with increased mortality in preterm infants. Pediatrics 2009; 123 (1): e138–e144.
Van Overmeire B, Smets K, Lecoutere D, Van de Broek H, Weyler J, Degroote K et al. A comparison of ibuprofen and indomethacin for closure of patent ductus arteriosus. N Engl J Med 2000; 343 (10): 674–681.
Boo NY, Mohd-Amin I, Bilkis AA, Yong-Junina F . Predictors of failed closure of patent ductus arteriosus with indomethacin. Singapore Med J 2006; 47 (9): 763–768.
Couser RJ, Ferrara TB, Wright GB, Cabalka AK, Schilling CG, Hoekstra RE et al. Prophylactic indomethacin therapy in the first twenty-four hours of life for the prevention of patent ductus arteriosus in preterm infants treated prophylactically with surfactant in the delivery room. J Pediatr 1996; 128 (5 Pt 1): 631–637.
Chorne N, Jegatheesan P, Lin E, Shi R, Clyman RI . Risk factors for persistent ductus arteriosus patency during indomethacin treatment. J Pediatr 2007; 151 (6): 629–634.
Itabashi K, Ohno T, Nishida H . Indomethacin responsiveness of patent ductus arteriosus and renal abnormalities in preterm infants treated with indomethacin. J Pediatr 2003; 143 (2): 203–207.
Kim ES, Kim EK, Choi CW, Kim HS, Kim BI, Choi JH et al. Intrauterine inflammation as a risk factor for persistent ductus arteriosus patency after cyclooxygenase inhibition in extremely low birth weight infants. J Pediatr 2010; 157 (5): 745–750 e741.
Dani C, Bertini G, Corsini I, Elia S, Vangi V, Pratesi S et al. The fate of ductus arteriosus in infants at 23-27 weeks of gestation: from spontaneous closure to ibuprofen resistance. Acta Paediatr 2008; 97 (9): 1176–1180.
Weiss H, Cooper B, Brook M, Schlueter M, Clyman R . Factors determining reopening of the ductus arteriosus after successful clinical closure with indomethacin. J Pediatr 1995; 127 (3): 466–471.
Van Overmeire B, Van de Broek H, Van Laer P, Weyler J, Vanhaesebrouck P . Early versus late indomethacin treatment for patent ductus arteriosus in premature infants with respiratory distress syndrome. J Pediatr 2001; 138 (2): 205–211.
Echtler K, Stark K, Lorenz M, Kerstan S, Walch A, Jennen L et al. Platelets contribute to postnatal occlusion of the ductus arteriosus. Nat Med 2010; 16 (1): 75–82.
Alyamac Dizdar E, Ozdemir R, Sari FN, Yurttutan S, Gokmen T, Erdeve O et al. Low platelet count is associated with ductus arteriosus patency in preterm newborns. Early Hum Dev 2012; 88 (10): 813–816.
Dani C, Poggi C, Fontanelli G . Relationship between platelet count and volume and spontaneous and pharmacological closure of ductus arteriosus in preterm infants. Am J Perinatol 2013; 30 (5): 359–364.
Fujioka K, Morioka I, Miwa A, Morikawa S, Shibata A, Yokoyama N et al. Does thrombocytopenia contribute to patent ductus arteriosus? Nat Med 2011; 17 (1): 29–30 author reply 30-21.
Sallmon H, Weber SC, Huning B, Stein A, Horn PA, Metze BC et al. Thrombocytopenia in the first 24 h after birth and incidence of patent ductus arteriosus. Pediatrics 2012; 130 (3): e623–e630.
Shah NA, Hills NK, Waleh N, McCurnin D, Seidner S, Chemtob S et al. Relationship between circulating platelet counts and ductus arteriosus patency after indomethacin treatment. J Pediatr 2011; 158 (6): 919–923 e911-912.
Waleh N, Hodnick R, Jhaveri N, McConaghy S, Dagle J, Seidner S et al. Patterns of gene expression in the ductus arteriosus are related to environmental and genetic risk factors for persistent ductus patency. Pediatr Res 2010; 68 (4): 292–297.
Waleh N, Seidner S, McCurnin D, Giavedoni L, Hodara V, Goelz S et al. Anatomic closure of the premature patent ductus arteriosus: The role of CD14+/CD163+ mononuclear cells and VEGF in neointimal mound formation. Pediatr Res 2011; 70 (4): 332–338.
Thebaud B, Wu XC, Kajimoto H, Bonnet S, Hashimoto K, Michelakis ED et al. Developmental absence of the O2 sensitivity of L-type calcium channels in preterm ductus arteriosus smooth muscle cells impairs O2 constriction contributing to patent ductus arteriosus. Pediatr Res 2008; 63 (2): 176–181.
Chen JX, O'Mara PW, Poole SD, Brown N, Ehinger NJ, Slaughter JC et al. Isoprostanes as physiological mediators of transition to newborn life: novel mechanisms regulating patency of the term and preterm ductus arteriosus. Pediatr Res 2012; 72 (2): 122–128.
Campbell M . Incidence of cardiac malformations at birth and later, and neonatal mortality. Br Heart J 1973; 35 (2): 189–200.
Stephens BE, Gargus RA, Walden RV, Mance M, Nye J, McKinley L et al. Fluid regimens in the first week of life may increase risk of patent ductus arteriosus in extremely low birth weight infants. J Perinatol 2008; 28 (2): 123–128.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author Contributions
Mohamed Farooq Ahamed: Dr Ahamed was responsible for acquisition of the data, analysis and interpretation of the data, drafting of the manuscript and critical revision of the manuscript for important intellectual content. Prasoon Verma: Dr Verma was responsible for acquisition of data. Drs Verma and Lee contributed equally to the manuscript. Simon Lee: Dr Lee was responsible for the study concept, acquisition of data and revision of the manuscript. Dan Wang: Ms. Wang was responsible for analysis and interpretation of the data, statistical analysis and revision of the manuscript for important intellectual content. Mimi Kim: Dr Kim was responsible for analysis and interpretation of the data, statistical analysis and critical revision of the manuscript for important intellectual content. Melissa Vega: Ms Vega was responsible for acquisition of the data and administrative, technical and material support. Mamta Fuloria: Dr Fuloria was responsible for the study concept and design, acquisition of the data, drafting of the manuscript, critical revision of the manuscript for important intellectual content and study supervision.
Rights and permissions
About this article
Cite this article
Ahamed, M., Verma, P., Lee, S. et al. Predictors of successful closure of patent ductus arteriosus with indomethacin. J Perinatol 35, 729–734 (2015). https://doi.org/10.1038/jp.2015.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.33
This article is cited by
-
Clinical and echocardiography predictors of response to first-line acetaminophen treatment in preterm infants with hemodynamically significant patent ductus arteriosus
Journal of Perinatology (2024)
-
Neonatal acute kidney injury during indomethacin therapy: does it predict ductal closure?
Journal of Nephrology (2023)
-
Predictors of successful patent ductus arteriosus closure with acetaminophen in preterm infants
Journal of Perinatology (2021)
-
Plasma B-type natriuretic peptide cannot predict treatment response to ibuprofen in preterm infants with patent ductus arteriosus
Scientific Reports (2020)
-
Base excess and hematocrit predict response to indomethacin in very low birth weight infants with patent ductus arteriosus
Italian Journal of Pediatrics (2019)