Abstract
Objective:
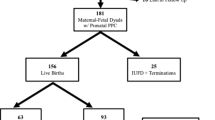
Review all live births 22 0/7 through 26 6/7 weeks gestation born 1996 through 2013 at our institution to describe the decision process and immediate outcomes of palliative comfort care (PCC) versus neonatal intensive care (NICU) and whether any significant family complaints or quality assurance concerns arose.
Study Design:
Retrospective chart review, physician and ethicist interview process and database review focused upon our established periviability counseling guidelines that are directive of PCC at 22 weeks gestation and NICU at 26 weeks but supportive of informed family choice of either option at 23, 24 and 25 weeks.
Result:
At 22 weeks—all 54 infants had PCC; at 23 weeks—29/78 (37%) chose NICU care, 6/29 (21%) infants survived; at 24 weeks—79/108 (73%) chose NICU care, 47/79 (59%) survived; at 25 weeks—147/153 (96%) chose NICU care, 115/147 (78%) survived; and at 26 weeks—all infants had NICU care, 176/203 (87%) survived. Over 18 years and 606 births, we identified only three significant concerns from families and/or physicians that required formal review.
Conclusion:
Most pregnant women and families choose NICU care for their extremely premature infant, but if given the option via shared decision making, a significant proportion will choose PCC at gestational ages that some NICUs mandate resuscitation. We support a reasoned dialogue and bioethical framework that recognizes human values to be irreducibly diverse, sometimes conflicting, and ultimately incommensurable—value pluralism. Respectful shared decision making requires thoughtful and compassionate flexibility, nuanced and individualized suggestions for PCC or NICU and the reduction of hierarchical directives from physicians to families. We continue to advocate and rely upon informed family preference between 23 and 25 weeks gestation in our updated 2015 periviability guidelines.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Raju TN, Mercer BM, Burchfield DJ, Joseph GF . Periviable birth: executive summary of a Joint Workshop by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Academy of Pediatrics, and American College of Obstetricians and Gynecologists. J Perinatol 2014; 34 (5): 333–342.
Srinivas SK . Periviable births: communication and counseling before delivery. Semin Perinatol 2013; 37: 426–430.
Arnold C, Tyson JE . Outcomes following periviable birth. Semin Perinatol 2014; 38: 2–11.
Meadow W . Ethics at the margins of viability. NeoReviews 2013; 14 (12): e588–e591.
Chervenak FA, McCullough LB, Levene MI . An ethically justified, clinically comprehensive approach to periviability: gynaecological, obstetric, perinatal and neonatal dimensions. J Obstet Gynaecol 2007; 27 (1): 3–7.
Janvier A, Barrington KJ . Advocating for the very preterm infant. Pediatrics 2006; 118 (1): 429–430.
Seaton SE, King S, Manktelow BN, Draper ES, Field DJ . Babies born at the threshold of viability: changes in survival and workload over 20 years. Arch Dis Child Fetal Neonatal Ed 2013; 98: F15–F20.
Kaempf JW, Tomlinson MW, Campbell B, Ferguson L, Stewart VT . Counseling pregnant women who may deliver extremely premature infants: medical care guidelines, family choices, and neonatal outcomes. Pediatrics 2009; 123 (6): 1509–1515.
Jefferies AL, Kirpalani HM . Counselling and management for anticipated extremely preterm birth. Paediatr Child Health 2012; 17 (8): 443–444.
Kipnis K . Harm and uncertainty in newborn intensive care. Theor Med Bioethics 2007; 28: 393–412.
Mercer BM, Raju TNK . Periviable birth: management and counseling issues – Volume 1. Semin Perinatol 2013; (37): 381.
Raju TNK, Mercer BM . Periviable birth: management and counseling issues – Part 2. Semin Perinatol 2014; 38: 1.
Kaempf JW, Tomlinson M, Arduza C, Anderson S, Campbell B, Ferguson L et al. Medical staff guidelines for periviability pregnancy counseling and medical treatment of extremely premature infants. Pediatrics 2006; 117 (1): 22–29.
Vermont Oxford Network Nightingale Electronic Reporting System, 2014. Available at www.vtoxford.org.
Holm S . A simple sequentially rejective multiple test procedure. Scand J Stat 1979; 6: 65–70.
Cummings J . Committee on Fetus and Newborn. Clinical report - antenatal counseling regarding resuscitation and intensive care before 25 weeks of gestation. Pediatrics 2015; 136: 588–595.
Gray J . Isaiah Berlin: An Interpretation of his Thought. Princeton University Press: Princeton, NJ, USA, 2013.
Rorty R . An Ethics for Today: Finding Common Ground Between Philosophy and Religion. Columbia University Press: New York, NY, USA, 2008.
Haidt J . The Righteous Mind: Why Good People are Divided by Politics and Religion. Pantheon Books: New York, NY, USA, 2012.
Tuohey J . Providence Health System Oregon region has created an ethics consult service. Health Prog 2006; 87 (2): 1–5.
Janvier A, Leblanc I, Barrington KJ . Nobody likes premies: the relative value of patient’s lives. J Perinatol 2008; 28: 821–826.
Janvier A, Mercurio MR . Saving vs creating: perceptions of intensive care at different ages and the potential for injustice. J Perinatol 2013; 33: 333–335.
Lantos J . Cruel calculus: why saving premature babies is better business than helping them thrive. Health Aff (Millwood) 2010; 29: 2114–2117.
Boss RD, Henderson CM, Wilfond BS . Decisions regarding resuscitation of extremely premature infants – should social context matter? JAMA Pediatr 2015; 169 (6): 521–522.
Caeymaex L, Jousselme C, Vasilescu C, Danan C, Falissard B, Bourrat MM et al. Perceived role in end-of-life decision making in the NICU affects long-term parental grief response. Arch Dis Child Fetal Neonatal Ed 2013; 98: F26–F31.
Guillen U, Weiss EM, Munson D, Maton P, Jefferies A, Norman M et al. Guidelines for the management of extremely premature deliveries: a systematic review. Pediatrics 2015; 136 (2): 343–350.
Rysavy MA, Li L, Bell EF, Das A, Hintz SR, Stoll BJ et al. Between-hospital variation in treatment and outcomes in extremely premature infants. N Engl J Med 2015; 372: 1801–1811.
Payot A, Gendron S, Lefebrve F, Doucet H . Deciding to resuscitate extremely premature babies: how do parents and neonatologists engage in the decision? Soc Sci Med 2007; 64: 1487–1500.
Orfali K, Gordon EJ . Autonomy gone awry: a cross-cultural study of parents’ experiences in neonatal intensive care units. Theor Med 2004; 25: 329–365.
Janvier A, Leblanc I, Barrington KJ . The best-interest standard is not applied for neonatal resuscitation decisions. Pediatrics 2008; 121 (5): 963–969.
Moore GP, Lemyre B, Barrowman N, Daboval T . Neurodevelopmental outcomes at 4 to 8 years of children born at 22 to 25 weeks gestational age: a meta-analysis. JAMA Pediatr 2013; 167 (10): 967–974.
Marlow N, Wolke D, Bracewell MA, Samara M . Neurologic and developmental disability at six years of age after extremely preterm birth. N Engl J Med 2005; 352 (1): 9–19.
Synnes AR, Anson S, Arkesteijn A, Butt A, Grunau RE, Rogers M et al. School entry age outcomes for infants with birth weight </= 800 grams. J Pediatr 2010; 157: 989–994.
Hintz SR, Kendrick DE, Wilson-Costello DE, Das A, Bell EF, Vohr BR et al. Early-childhood neurodevelopmental outcomes are not improving for infants born at <25 weeks gestational age. Pediatrics 2011; 127 (1): 62–70.
Sayeed S, Padela A, Naim MY, Lantos JD . A Saudi family making end-of-life decisions in the PICU. Pediatrics 2012; 129 (4): 764–769.
Haward MF, Kirshenbaum NW, Campbell DE . Care at the edge of viability: medical and ethical issues. Clin Perinatol 2011; 38: 471–492.
Silverman WA . Medical decisions: an appeal for reasonableness. Pediatrics 1996; 98 (6): 1182–1184.
Gray J . Straw Dogs. Granta Publications: London, England, 2002.
Zwicker JG, Richardson Harris S . Quality of life of formerly preterm and very low birth weight infants from preschool age to adulthood: a systematic review. Pediatrics 2008; 121 (2): e366–e376.
Ross LF, Frader JE . Newborns and other children: in defense of differential attitudes and treatment. J Pediatr 2013; 162 (6): 1096–1099.
Bell EF . Committee on Fetus and Newborn. Non-initiation or withdrawal of intensive care for high-risk newborns. Pediatrics 2007; 119 (2): 401–403.
Stark AR . Committee on Fetus and Newborn. Clinical report – antenatal counseling regarding resuscitation at an extremely low gestational age. Pediatrics 2009; 124 (1): 422–427.
Gallagher K, Martin J, Keller M, Marlow N . European variation in decision-making and parental involvement during preterm birth. Arch Dis Child Fetal Neonatal Ed 2014; 99: F245–F249.
Kopelman LM . The best interests standard for incompetent or incapacitated persons of all ages. J Law Med Ethics 2007; 35: 187–196.
Harrison H . The offer they can’t refuse: parents and perinatal treatment decisions. Semin Fetal Neonatal Med 2008; 13: 329–334.
Wittgenstein LW . Tractatus Logico-Philosophicus. Harcourt, Brace and Company: New York, NY, USA, 1922.
Acknowledgements
This investigation was supported by the Providence Health and Services Foundation (Portland, OR) and Northwest Newborn Specialists, PC (Portland, OR). The sponsors had no role in the design or conduct of the study. We are indebted to every pregnant woman who presented to Providence St Vincent Medical Center 1996 through 2013 with the possibility of extremely premature birth. We acknowledge their travail, thank them for their insight, respect their experience and learn from them and pledge to improve our counseling and care process. We thank Nicole Tipping, RN for her skilled assistance and dedication to accurate chart and data base review and Lian Wang, MS for her expertise in providing statistical analysis.
Author contributions
The principal investigator Joseph W Kaempf, MD had full access to the data in the study and takes responsibility for the integrity and accuracy of the data analysis. JWK was responsible for the original conception and design of the study and drafted the first and final versions of the manuscript. Co-authors MWT and JT assisted in critical review of the manuscript at every step, all data analysis and participated in the manuscript formulation and final revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Kaempf, J., Tomlinson, M. & Tuohey, J. Extremely premature birth and the choice of neonatal intensive care versus palliative comfort care: an 18-year single-center experience. J Perinatol 36, 190–195 (2016). https://doi.org/10.1038/jp.2015.171
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.171
This article is cited by
-
Extremely premature birth bioethical decision-making supported by dialogics and pragmatism
BMC Medical Ethics (2023)
-
Assessing shared decision making during antenatal consultations regarding extreme prematurity
Journal of Perinatology (2023)
-
Parental request for non-resuscitation in fetal myelomeningocele repair: an analysis of the novel ethical tensions in fetal intervention
Journal of Perinatology (2022)
-
The importance of shared decision-making in the neonatal intensive care unit
Journal of Perinatology (2020)
-
Effect of written outcome information on attitude of perinatal healthcare professionals at the limit of viability: a randomized study
BMC Medical Ethics (2019)