Abstract
Background:
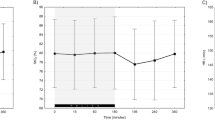
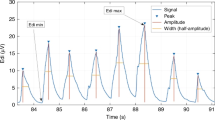
Neurally adjusted ventilator assist (NAVA) uses electrical activity of the diaphragm (Edi) to provide patient-directed ventilatory support. The NAVA level determines the proportional amount of ventilatory support. Systematically increasing NAVA level initially increases peak inspiratory pressure (PIP) while maintaining a constant Edi until a breakpoint (BrP) is reached. Further increases in NAVA level reduce the Edi, while the PIP plateaus. This study was performed to establish whether premature neonates have intact neural feedback systems allowing them to have a BrP.
Method:
NAVA level was increased by 0.5 cm H2O μV−1 every 3 min from 0.5 to 4.0 cm H2O μV−1. PIP, Edi, mean blood pressure, heart rate, respiratory rate, oxygen saturation and FIO2 were recorded. Statistics: Non-linear regression was done for PIP and Edi. Linear regression was done for the other variables. The data from the trials were combined by normalizing to NAVA levels above and below the BrP.
Result:
Nine neonates were studied on NAVA and 12 on non-invasive NAVA. PIP increased until the BrP was reached and then remained unchanged. Edi decreased after the BrP was reached. All other variables remained unchanged.
Conclusion:
Neonates demonstrated a BrP suggesting intact neural feedback mechanisms that may protect lungs from over distention with NAVA ventilation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Beck J, Sinderby C, Lindstrom L, Grassino A . Effects of lung volume on diaphragm EMG signal strength during voluntary contractions. J Appl Physiol 1998; 85: 1123–1134.
Sinderby C, Beck J, Spahija J, Weinberg J, Grassino A . Voluntary activation of the human diaphragm in health and disease. J Appl Physiol 1998; 85 (6): 2146–2158.
Sinderby C, Beck J . Neurally adjusted ventilatory assist (NAVA): an update and summary of experiences. Neth J Crit Care 2007; 11 (5): 243–252.
Navalesi P, Colombo D, Della Corte F . NAVA ventilaton. Minerva Anestesiol 2010; 76: 346–352.
Beck J, Reilly M, Grasselli G, Mirabella L, Slutsky AS, Dunn MS et al. Patient-ventilator interaction during neurally adjusted ventilatory assist in low birth weight infants. Pediatr Res 2009; 65 (6): 663–668.
Vignaux L, Grazioli S, Piquilloud L, Bochaton N, Karam O, Levy-Jamet Y et al. Patient-ventilator asynchrony during noninvasive pressure support ventilation and Neurally Adjusted Ventilatory Assist in infants and children. Pediatr Crit Care Med 2013; 14 (8): e357–e364.
Jubran A, Mathru M, Dries D, Tobin MJ . Continuous recording of mixed venous oxygen saturation during wenaing from mechanical ventilation and the ramificatons thereof. Am J Respir Crit Care Med 1998; 158: 1763–1769.
Levine S, Nguyen T, Taylor N, Friscia ME, Budak MT, Rothenberg P et al. Rapid disuse atrophy of diaphragmatic fibers in mechanically ventilated humans. N Engl J Med 2008; 358 (13): 1327–1335.
Lecomte F, Brander L, Jalde F, Beck J, Qui H, Elie C et al. Physiological response to increasing levels of neurally adjusted ventilatory assist (NAVA). Respir Physiol Neurobiol 2009; 166 (2): 117–124.
Brander L, Leong-Poi H, Beck J, Brunet F, Hutchison SJ, Slutsky AS et al. Titration and implementation of neurally adjusted ventilatory assist in critically ill patients. Chest 2009; 135 (3): 695–703.
Sinderby C, Beck J, Spahija J, de Marchie M, Lacroix J, Navalesi P et al. Inspiratory muscle unloading by neurally adjusted ventilatory assist during maximal inspiratory efforts in healthy subjects. Chest 2007; 131 (3): 711–717.
Ververidis D, Van Gils M, Passath C, Takala J, Brander L . Identification of adequate neurally adjusted ventilatory assist (NAVA) during systematic increases in the NAVA level. IEEE Trans Biomed Eng 2011; 58 (9): 2598–2606.
Patroniti N, Bellani G, Saccavino E, Zanella A, Grasselli G, Isgro S et al. Respiratory pattern during neurally adjusted ventilatory assist in acute respiratory failure patients. Intensive Care Med 2011; 38 (2): 230–239.
Stein HM, Firestone KS . Nava ventilation in neonates: clinical guidelines and management strategies. Neonatol Today 2012; 7 (4): 1–8.
Passath C, Takala J, Tuchscherer D, Jakob SM, Sinderby C, Brander L . Physiological response to changing positive end-expiratory pressure during neurally adjusted ventilatory assist in sedated critically ill adults. Chest 2010; 138 (3): 578–587.
Marantz S, Patrick W, Webster K, Roberts D, Oppenheimer L, Younes M . Response of ventilator-dependent patients to different levels of proportional assist. J Appl Physiol 1996; 80: 397–403.
Kondili E, Xirouchaki N, Vaporidi K, Klimathianaki M, Georgopoulos D . Short-term cardiorespiratory effects of proportional assist and pressure-support ventilation in patients with acute lung injury/acute respiratory distress syndrome. Anesthesiology 2006; 105: 703–708.
Hering E, Breuer J . Die selbststeurung der athmung den nervus vagus. Sitzber Deut Akad Wiss Wein 1868; 57: 672–677.
Vitale V, Duperret S, Mahul P, Delafosse B, Delpuech C, Weismann D et al. Time course evolution of ventilatory responses to inspiratory unloading in patients. Am J Respir Crit Care Med 1998; 157: 428–434.
Acknowledgements
This study was supported by Promedica Toledo Children’s Hospital and Akron Children’s Hospital.
Author Contributions
KSF, SF, SR and HMS contributed to study concept and design, data collection, analysis and interpretation and in writing of the manuscript. DBW contributed to statistical design, data analysis and in writing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Howard M Stein and Kimberly S Firestone are speakers for MAQUET. All other authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Firestone, K., Fisher, S., Reddy, S. et al. Effect of changing NAVA levels on peak inspiratory pressures and electrical activity of the diaphragm in premature neonates. J Perinatol 35, 612–616 (2015). https://doi.org/10.1038/jp.2015.14
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2015.14
This article is cited by
-
Non-invasive neurally adjusted ventilatory assist in preterm infants with RDS: effect of changing NAVA levels
European Journal of Pediatrics (2022)
-
Modes and strategies for providing conventional mechanical ventilation in neonates
Pediatric Research (2021)
-
Effects of heliox and non-invasive neurally adjusted ventilatory assist (NIV-NAVA) in preterm infants
Scientific Reports (2021)
-
Evaluating peak inspiratory pressures and tidal volume in premature neonates on NAVA ventilation
European Journal of Pediatrics (2021)
-
Feasibility and physiological effects of noninvasive neurally adjusted ventilatory assist in preterm infants
Pediatric Research (2017)