Abstract
Objective:
To investigate the effect of lung recruitment maneuver (LRM) with positive end-expiratory pressure (PEEP) on oxygenation and outcomes in preterm infants ventilated by proportional assist ventilation (PAV) for respiratory distress syndrome (RDS).
Study Design:
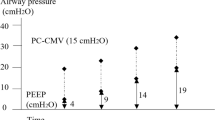
Preterm infants on PAV for RDS after surfactant randomly received an LRM (group A, n=12) or did not (group B, n=12). LRM entailed increments of 0.2 cm H2O PEEP every 5 min, until fraction of inspired oxygen (FiO2)=0.25. Then PEEP was reduced and the lung volume was set on the deflation limb of the pressure/volume curve. When saturation of peripheral oxygen fell and FiO2 rose, we reincremented PEEP until SpO2 became stable.
Result:
Group A and B infants were similar: gestational age 29.5±1.0 vs 29.4±0.9 weeks; body weight 1314±96 vs 1296±88 g; Silverman Anderson score for babies at start of ventilation 8.6±0.8 vs 8.2±0.7; initial FiO2 0.56±0.16 vs 0.51±0.14, respectively. The less doses of surfactant administered in group A than that in group B (P<0.05). Groups A and B showed different max PEEP during the first 12 h of life (8.4±0.5 vs 6.7±0.6 cm H2O, P=0.00), time to lowest FiO2 (101±18 versus 342±128 min; P=0.000) and O2 dependency (7.83±2.04 vs 9.92±2.78 days; P=0.04). FiO2 levels progressively decreased (F=43.240, P=0.000) and a/AO2 ratio gradually increased (F=30.594, P=0.000). No adverse events and no differences in the outcomes were observed.
Conclusion:
LRM led to the earlier lowest FiO2 of the first 12 h of life and a shorter O2 dependency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Muscedere JG, Mullen JB, Gan K, Slutsky AS . Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 1994; 149: 1327–1334.
Van Kaam AH, de Jaegere A, Haitsma JJ, Van Aalderen WM, Kok JH, Lachmann B . Positive pressure ventilation with the open lung concept optimizes gas exchange and reduces ventilator induced lung injury in newborn piglets. Pediatr Res 2003; 53: 245–253.
Rimensberger PC, Cox PN, Frndova H, Bryan AC . The open lung during small tidal volume ventilation: concepts of recruitment and ‘optimal’ positive end-expiratory pressure. Crit Care Med 1999; 27: 1946–1952.
Schulze A, Bancalari E . Proportional assist ventilation in infants. Clin Perinatol 2001; 28: 561–578.
Sabapathi S, David GS . Management of neonatal respiratory distress syndrome. Paediatr Child Health 2012; 22: 518–522.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R et al. European consensus guidelines on the management of neonatal respiratory distress syndrome in preterm infants-2010 update. Neonatology 2010; 97: 402–417.
Colman Y, Krauss B . Microstream capnography technology: A new approach to an old problem. J Clin Monit 1999; 15: 403–409.
Silverman WC, Anderson DH . Controlled clinical trial on effects of water mist on obstructive respiratory signs, death rate and necropsy findings among premature infants. Pediatrics 1956; 17: 1–4.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA et al. National Institutes of Child Health and Human Development Neonatal Research Network. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics 2005; 116: 1353–1360.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978; 92: 529–534.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol 2005; 123: 991–999.
Richard JC, Maggiore SM, Mercat A . Clinical review: bedside assessment of alveolar recruitment. Crit Care 2004; 8: 163–169.
Rouby JJ . Lung overinflation: the hidden face of alveolar recruitment. Anesthesiology 2003; 99: 2–4.
Muscedere JG, Mullen JBM, Gan K, Slutsky AS . Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 1994; 149: 1327–1334.
Halter JM, Steinberg JM, Schiller HJ, Da Silva M, Gatto LA, Landas S et al. Positive end-expiratory pressure after a recruitment maneuver prevents both alveolar collapse and recruitment/derecruitment. Am J Respir Crit Care Med 2003; 167: 1620–1626.
Muscedere JG, Mullen JB, Gan K, Slutsky AS . Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 1994; 149: 1327–1334.
Dreyfuss D, Saumon G . Barotrauma is volutrauma but which volume is the one responsible? Intensive Care Med 1992; 18: 139–141.
Ricard JD, Dreyfuss D, Saumon G . Ventilator-induced lung injury. Eur Respir J Suppl 2003; (42: 2S–9S.
Tobin MJ . Mechanical ventilation. N Engl J Med 1994; 330: 1056–1061.
Muscedere JG, Mullen BM, Gan K, Slutsky AS . Tidal ventilation at low airway pressures can augment lung injury. Am J Respir Crit Care Med 1994; 149: 1327–1334.
Tusman G, Bohm SH, Vazquez de Anda GF, do Campo JL, Lachmann B . ‘Alveolar recruitment strategy’ improves arterial oxygenation during general anaesthesia. Br J Anaesth 1999; 82: 8–13.
Maisch S, Reissmann H, Fuellekrug B, Weismann D, Rutkowski T, Tusman G et al. Compliance and dead space fraction indicate an optimal level of positive endexpiratory pressure after recruitment in anesthetized patients. Anesth Analg 2008; 106: 175–181.
Castoldi F, Daniele I, Fontana P, Cavigioli F, Lupo E, Lista G . Lung Recruitment Maneuver during Volume Guarantee Ventilation of Preterm Infants with Acute Respiratory Distress Syndrome. Am J Perinatol 2011; 28: 521–528.
Jobe A, Ikegami M, Jacobs H, Jones S . Surfactant and pulmonary blood flow distributions following treatment of premature lambs with natural surfactant. J Clin Invest 1984; 73: 848–856.
O ’Donnell CPF, Stenson BJ . Respiratory strategies for preterm infants at birth. Semin Fetal Neonatal Med 2008; 13: 401–409.
Moya FR, Sinha SK . Surfactant trials. Pediatrics 2006; 117: 245–247.
Acknowledgements
We thank all the neonatal units and staff who responded to our survey. This research was funded by grants from Jiangsu Province Health Department (Project no: F201233).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wu, R., Li, SB., Tian, ZF. et al. Lung recruitment maneuver during proportional assist ventilation of preterm infants with acute respiratory distress syndrome. J Perinatol 34, 524–527 (2014). https://doi.org/10.1038/jp.2014.53
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.53