Abstract
Objective:
To evaluate the cardiovascular response to short-term prone positioning in neonates.
Study design:
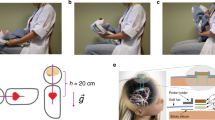
In this prospective study, we continuously monitored heart rate (HR), stroke volume (SV) and cardiac output (CO) by electrical velocimetry in hemodynamically stable neonates in each of the following positions for 10 min: supine, prone and back-to-supine position. Skin blood flow (SBF) was also continuously assessed on the forehead or foot using Laser Doppler technology. Systemic vascular resistance (SVR) index was calculated as mean blood pressure (BP)/CO. Data were analyzed using repeated measures analysis of variance.
Results:
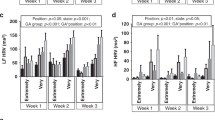
Thirty neonates (gestational age: 35±4 weeks; postmenstrual age: 36±3 weeks) were enrolled. HR did not change in response to positioning. However, in prone position, SV, CO and SBF decreased and SVR index increased from 1.5±0.3 to 1.3±0.3 ml kg−1 (mean ±s.d., P<0.01), 206±44 to 180±41 ml kg−1 min−1 (P<0.01), 0.54±0.30 to 0.44±0.29 perfusion units (P<0.01) and 0.25±0.06 to 0.30±0.07 mm Hg ml−1 kg−1 min−1 (P<0.01), respectively. After placing the infants back-to-supine position, SV, CO, SBF and SVR index returned to baseline. The above pattern of cardiovascular changes was consistent in vast majority of the studied neonates.
Conclusions:
Short-term prone positioning is associated with decreased SV, CO and SBF and increased calculated SVR index.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Balaguer A, Escribano J, Roqué I, Figuls M, Rivas-Fernandez M . Infant position in neonates receiving mechanical ventilation. Cochrane Database Syst Rev 2013; 3: CD003668.
McEvoy C, Mendoza ME, Bowling S, Hewlett V, Sardesai S, Durand M . Prone positioning decreases episodes of hypoxemia in extremely low birth weight infants (1000 grams or less) with chronic lung disease. J Pediatr 1997; 130: 305–309.
Chen SS, Tzeng YL, Gau BS, Kuo PC, Chen JY . Effects of prone and supine positioning on gastric residuals in preterm infants: a time series with cross-over study. Int J Nurs Stud 2013; 50: 1459–1467.
Chang YJ, Anderson GC, Lin CH . Effects of prone and supine positions on sleep state and stress responses in mechanically ventilated preterm infants during the first postnatal week. J Adv Nurs 2002; 40: 161–169.
Bembich S, Oretti C, Travan L, Clarici A, Massaccesi S, Demarini S . Effects of prone and supine position on cerebral blood flow in preterm infants. J Pediatr 2012; 160: 162–164.
Wong FY, Witcombe NB, Yiallourou SR, Yorkston S, Dymowski AR, Krishnan L et al. Cerebral oxygenation is depressed during sleep in healthy term infants when they sleep prone. Pediatrics 2011; 127: e558–e565.
Edgcombe H, Carter K, Yarrow S . Anaesthesia in the prone position. Br J Anaesth 2008; 100: 165–183.
Dharmavaram S, Jellish WS, Nockels RP, Shea J, Mehmood R, Ghanayem A et al. Effect of prone positioning systems on hemodynamic and cardiac function during lumbar spine surgery: an echocardiographic study. Spine (Phila Pa 1976) 2006; 31: 1388–1393 Discussion 1394.
Sudheer PS, Logan SW, Ateleanu B, Hall JE . Haemodynamic effects of the prone position: a comparison of propofol total intravenous and inhalation anaesthesia. Anaesthesia 2006; 61: 138–141.
Schaefer WM, Lipke CS, Kühl HP, Koch KC, Kaiser HJ, Reinartz P et al. Prone versus supine patient positioning during gated 99mTc-sestamibi SPECT: effect on left ventricular volumes, ejection fraction, and heart rate. J Nucl Med 2004; 45: 2016–2020.
Pump B, Talleruphuus U, Christensen NJ, Warberg J, Norsk P . Effects of supine, prone, and lateral positions on cardiovascular and renal variables in humans. Am J Physiol Regul Integr Comp Physiol 2002; 283: R174–R180.
Yap K, Campbell P, Cherk M, McGrath C, Kalff V . Effect of prone versus supine positioning on left ventricular ejection fraction (LVEF) and heart rate using ECG gated Tl-201 myocardial perfusion scans and gated cardiac blood pool scans. J Med Imaging Radiat Oncol 2012; 56: 525–531.
Osthaus WA, Huber D, Beck C, Winterhalter M, Boethig D, Wessel A et al. Comparison of electrical velocimetry and transpulmonary thermodilution for measuring cardiac output in piglets. Paediatr Anaesth 2007; 17: 749–755.
Norozi K, Beck C, Osthaus WA, Wille I, Wessel A, Bertram H . Electrical velocimetry for measuring cardiac output in children with congenital heart disease. Br J Anaesth 2008; 100: 88–94.
Zoremba N, Bickenbach J, Krauss B, Rossaint R, Kuhlen R, Schälte G . Comparison of electrical velocimetry and thermodilution techniques for the measurement of cardiac output. Acta Anaesthesiol Scand 2007; 51: 1314–1319.
Noori S, Drabu B, Soleymani S, Seri I . Continuous non-invasive cardiac output measurements in the neonate by electrical velocimetry: a comparison with echocardiography. Arch Dis Child Fetal Neonatal Ed 2012; 97: F340–F343.
Skatvedt O, Grøgaard J . Infant sleeping position and inspiratory pressures in the upper airways and oesophagus. Arch Dis Child 1994; 71: 138–140.
Yiallourou SR, Sands SA, Walker AM, Horne RS . Maturation of heart rate and blood pressure variability during sleep in term-born infants. Sleep 2012; 35: 177–186.
Sahni R, Schulze KF, Kashyap S, Ohira-Kist K, Fifer WP, Myers MM . Postural differences in cardiac dynamics during quiet and active sleep in low birthweight infants. Acta Paediatr 1999; 88: 1396–1401.
Ammari A, Schulze KF, Ohira-Kist K, Kashyap S, Fifer WP, Myers MM et al. Effects of body position on thermal, cardiorespiratory and metabolic activity in low birth weight infants. Early Hum Dev 2009; 85: 497–501.
Yiallourou SR, Walker AM, Horne RS . Effects of sleeping position on development of infant cardiovascular control. Arch Dis Child 2008; 93: 868–872.
Chong A, Murphy N, Matthews T . Effect of prone sleeping on circulatory control in infants. Arch Dis Child 2000; 82: 253–256.
Acknowledgements
This study was, in part, supported by grant support from the National Heart, Lung and Blood Institute (1RO1HL103765-01).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ma, M., Noori, S., Maarek, JM. et al. Prone positioning decreases cardiac output and increases systemic vascular resistance in neonates. J Perinatol 35, 424–427 (2015). https://doi.org/10.1038/jp.2014.230
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2014.230
This article is cited by
-
Comparison of massage and prone position on heart rate and blood oxygen saturation level in preterm neonates hospitalized in neonatal intensive care units
Egyptian Pediatric Association Gazette (2023)
-
Prone sleeping affects cardiovascular control in preterm infants in NICU
Pediatric Research (2021)
-
Elevated midline head positioning of extremely low birth weight infants: effects on cardiopulmonary function and the incidence of periventricular-intraventricular hemorrhage
Journal of Perinatology (2019)
-
Epinephrine versus dopamine in neonatal septic shock: a double-blind randomized controlled trial
European Journal of Pediatrics (2018)
-
Cardiac output decreases and systemic vascular resistance increases in newborns placed in the left-lateral position
Journal of Perinatology (2017)