Abstract
Objective:
To compare work of breathing (WOB) indices between two nCPAP settings and two levels of HFNC in a crossover study.
Study Design:
Infants with a CGA 28–40 weeks, baseline of HFNC 3–5 lpm or nCPAP 5-6 cmH2O and fraction of inspired oxygen ⩽40% were eligible. WOB was analyzed using respiratory inductive plethysmography (RIP) for each of the four modalities: HFNC 3 and 5 lpm, nCPAP 5 and 6 cmH2O. N=20; Study weight 1516 g (±40 g).
Result:
Approximately 12 000 breaths were analyzed indicating a high degree of asynchronous breathing and elevated WOB indices at all four levels of support. Phase angle values (means) (P<0.01): HFNC 3 lpm (114.7°), HFNC 5 lpm (96.7°), nCPAP 5 cmH2O (87.2°), nCPAP 6 cmH2O (80.5°). The mean phase relation of total breath (PhRTB) (means) (P<0.01): HFNC 3 lpm (63.2%), HFNC 5 lpm (55.3%), nCPAP 5 cmH2O (49.3%), nCPAP 6 cmH2O (48.0%). The relative labored breathing index (LBI) (means) (P⩽0.001): HFNC 3 lpm (1.39), HFNC 5 lpm (1.31), nCPAP 5 cmH2O (1.29), nCPAP 6 cmH2O (1.26). Eighty-two percent of the study subjects—respiratory mode combinations displayed clustering, in which a proportion of breaths either occurred predominantly out-of-phase (relative asynchrony) or in-phase (relative synchrony).
Conclusion:
In this study, WOB indices were statistically different, yet clinically similar in that they were elevated with respect to normal values. These infants with mild-to-moderate respiratory insufficiency demonstrate a meaningful elevation in WOB indices and continue to require non-invasive respiratory support. Patient variability exists with regard to biphasic clustered breathing patterns and the level of supplemental fraction of inspired oxygen ⩽40% alone does not provide guidance to the optimal matching of WOB indices and non-invasive respiratory support.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Donn SM, Sinha SK . Minimising ventilator induced lung injury in preterm infants. Arch Dis Child Fetal Neonatal Ed 2006; 91 (3): F226–F230.
Holleman-Duray D, Kaupie D, Weiss MG . Heated humidified high-flow nasal cannula: use and a neonatal early extubation protocol. J Perinatol 2007; 27 (12): 776–781.
Shoemaker MT, Pierce MR, Yoder BA, DiGeronimo RJ . High flow nasal cannula versus nasal CPAP for neonatal respiratory disease: a retrospective study. J Perinatol 2007; 27 (2): 85–91.
DeLemos RA, McLaughlin GW, Robison EJ, Schulz J, Kirby RR . Continuous positive airway pressure as an adjunct to mechanical ventilation in the newborn with respiratory distress syndrome. Anesth Analg 1973; 52 (3): 328–332.
Chernick V . Hyaline-membrane disease: therapy with constant lung-distending pressure. N Engl J Med 1973; 289 (6): 302–304.
Chatila WMD, Nugent TMD, Vance GRN, Gaughan JP, Criner GJMD . The effects of high-flow vs low-flow oxygen on exercise in advanced obstructive airways disease. Chest 2004; 126 (4): 1108–1115.
Dysart K, Miller TL, Wolfson MR, Shaffer TH . Research in high flow therapy: mechanisms of action. Respir Med 2009; 103 (10): 1400–1405.
Frizzola M, Miller TL, Rodriguez ME, Zhu Y, Rojas J, Hesek A et al. High-flow nasal cannula: impact on oxygenation and ventilation in an acute lung injury model. Pediatr Pulmonol 2011; 46 (1): 67–74.
Miller SM, Dowd SA . High-flow nasal cannula and extubation success in the premature infant: a comparison of two modalities. J Perinatol 2010; 30 (12): 805–808.
TMDM Spentzas, Minarik MMD, Patters AB, BCRTL Vinson, GMD Stidham . Children with respiratory distress treated with high-flow nasal cannula. J Intens Care Med 2009; 24 (5): 323–328.
Saslow JG, Aghai ZH, Nakhla TA, Hart JJ, Lawrysh R, Stahl GE et al. Work of breathing using high-flow nasal cannula in preterm infants. J Perinatol 2006; 26 (8): 476–480.
Locke RG, Wolfson MR, Shaffer TH, Rubenstein SD, Greenspan JS . Inadvertent administration of positive end-distending pressure during nasal cannula flow. Pediatrics 1993; 91 (1): 135–138.
Sivieri EM, Gerdes JS, Abbasi S . Effect of HFNC flow rate, cannula size, and nares diameter on generated airway pressures: an in vitro study. Pediatr Pulmonol 2012; 48 (5): 506–514.
Spence KL, Murphy D, Kilian C, McGonigle R, Kilani RA . High-flow nasal cannula as a device to provide continuous positive airway pressure in infants. J Perinatol 2007; 27 (12): 772–775.
Kubicka ZJ, Limauro J, Darnall RA . Heated, humidified high-flow nasal cannula therapy: yet another way to deliver continuous positive airway pressure? Pediatrics 2008; 121 (1): 82–88.
de Klerk A . Humidified high-flow nasal cannula: is it the new and improved CPAP? Adv Neonat Care 2008; 8 (2): 98–106.
Hammer J . NC. Assessment of thoraco-abdominal asynchrony. Paediatr Resp Rev 2009; 10 (2): 75–80.
Gappa M, Pillow JJ, Allen J, Mayer O, Stocks J . Lung function tests in neonates and infants with chronic lung disease: lung and chest-wall mechanics. Pediatr Pulmonol 2006; 41 (4): 291–317.
Wolfson MR, Greenspan JS, Deoras KS, Allen JL, Shaffer TH . Effect of position on the mechanical interaction between the rib cage and abdomen in preterm infants. J Appl Physiol 1992; 72 (3): 1032–1038.
Allen JL, Greenspan JS, Deoras KS, Keklikian E, Wolfson MR, Shaffer TH . Interaction between chest wall motion and lung mechanics in normal infants and infants with bronchopulmonary dysplasia. Pediatr Pulmonol 1991; 11 (1): 37–43.
Allen JL, Wolfson MR, McDowell K, Shaffer TH . Thoracoabdominal asynchrony in infants with airflow obstruction. Am Rev Respir Dis 1990; 141 (2): 337–342.
Locke R, Greenspan JS, Shaffer TH, Rubenstein SD, Wolfson MR . Effect of nasal CPAP on thoracoabdominal motion in neonates with respiratory insufficiency. Pediatr Pulmonol 1991; 11 (3): 259–264.
Deoras KS, Greenspan JS, Wolfson MR, Keklikian EN, Shaffer TH, Allen JL . Effects of inspiratory resistive loading on chest wall motion and ventilation: differences between preterm and full-term infants. Pediatr Res 1992; 32 (5): 589–594.
Miller TL, Palmer C, Shaffer TH, Wolfson MR . Neonatal chest wall suspension splint: a novel and noninvasive method for support of lung volume. Pediatr Pulmonol 2005; 39 (6): 512–520.
Miller TL, Cox T, Blackson T, Paul D, Weiss K, Shaffer TH . Pulmonary function assessment in an infant with Barnes syndrome: proactive evaluation for surgical intervention. Pediatrics 2006; 118 (4): e1264–e1267.
Rodriguez ME, Mackenzie WG, Ditro C, Miller TL, Chidekel A, Shaffer TH . Skeletal dysplasias: evaluation with impulse oscillometry and thoracoabdominal motion analysis. Pediatr Pulmonol 2010; 45 (7): 679–686.
Warren RH, Horan SM, Robertson PK . Chest wall motion in preterm infants using respiratory inductive plethysmography. Eur Respir J. 1997; 10 (10): 2295–2300.
Newth CJL, Hammer J . Measurements of Thoraco-Abdominal Asynchrony and Work of Breathing in Children. Paediatric Pulmonary Function Testing: Basel, Karger; 2005. 9 p.
Rusconi F, Gagliardi L, Aston H, Silverman M . Respiratory inductive plethysmography in the evaluation of lower airway obstruction during methacholine challenge in infants. Pediatr Pulmonol 1995; 20 (6): 396–402.
Hellwig B, Hengstler JG, Schmidt M, Gehrmann MC, Schormann W, Rahnenfuhrer J . Comparison of scores for bimodality of gene expression distributions and genome-wide evaluation of the prognostic relevance of high-scoring genes. BMC bioinformatics. 2010; 11: 276.
Technology NIoSa. Guide to the Statistical Tests. csrc.nist.gov/groups/ST/toolkit/rng/stats_tests.html2000 [updated June 19, 2012; cited 2013 January].
Campbell DM, Shah PS, Shah V, Kelly EN . Nasal continuous positive airway pressure from high flow cannula versus infant flow for preterm infants. J Perinatol 2006; 26 (9): 546–549.
TL Miller . High flow nasal cannula therapy in neonatology. Resp Ther 8 (2): 30–35.
Chang GY, Cox CA, Shaffer TH . Nasal cannula, CPAP, and high-flow nasal cannula: effect of flow on temperature, humidity, pressure, and resistance. Biomed Instr Technol 2011; 45 (1): 69–74.
Acknowledgements
We would like to thank the parents and families in the Neonatal Intensive Care Unit. This study was supported by Nemours Biomedical Research (THS), NIH COBRE P20 GM 103464-8 (THS), Christiana Neonatal Research (RL, BDJ) and NIGMS T32-GM08562 (ER) pediatric clinical pharmacology fellow funded by NICHD.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
de Jongh, B., Locke, R., Mackley, A. et al. Work of breathing indices in infants with respiratory insufficiency receiving high-flow nasal cannula and nasal continuous positive airway pressure. J Perinatol 34, 27–32 (2014). https://doi.org/10.1038/jp.2013.120
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2013.120
Keywords
This article is cited by
-
Machine learning for automatic identification of thoracoabdominal asynchrony in children
Pediatric Research (2021)
-
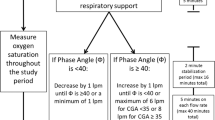
Adjustment of high flow nasal cannula rates using real-time work of breathing indices in premature infants with respiratory insufficiency
Journal of Perinatology (2021)
-
Effects of nasal high flow on nocturnal hypercapnia, sleep, and sympathovagal balance in patients with neuromuscular disorders
Sleep and Breathing (2021)
-
A novel noninvasive approach for evaluating work of breathing indices in a developmental rat model using respiratory inductance plethysmography
Scientific Reports (2020)
-
Cardiorespiratory behavior of preterm infants receiving continuous positive airway pressure and high flow nasal cannula post extubation: randomized crossover study
Pediatric Research (2020)