Abstract
Objective:
To determine factors associated with latency time to birth after preterm premature rupture of membranes (PPROM) and the impact on neonatal outcomes.
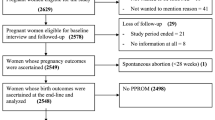
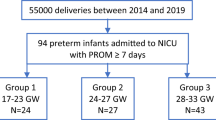
Study Design:
Data on singleton pregnancies with PPROM (n=1535 infants) were prospectively collected in a computerized perinatal/neonatal database at a tertiary care perinatal center. Latency was characterized as ⩽72h versus >72 h after PPROM.
Result:
The percentage of women with latency to birth >72 h decreased from 67% in very preterm (gestational age (GA) 25 to 28 weeks) to 10% in late preterm women (GA 33 to 36 weeks). PPROM women with latency ⩽72 h were more likely to have pregnancy-induced hypertension and birth weight <3%; PPROM women with latency >72 h were more likely to have received steroids and develop clinical chorioamnionitis. PPROM <32 weeks GA with latency ⩽72 h was associated with a two-fold higher incidence of severe neonatal morbidity, while PPROM between 29 to 34 weeks GA and latency ⩽72 h was associated with a higher incidence of moderate neonatal morbidity.
Conclusion:
A latency period >72 h was associated with a decreased incidence of adverse neonatal outcomes up to 32 weeks GA for severe and 34 weeks GA for moderate morbidity indices.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Goldenberg RL, Culhane JF, Iams JD, Romero R . Epidemiology and causes of preterm birth. Lancet 2008; 371 (9606): 75–84.
Mercer BM . Preterm premature rupture of the membranes. Obstet Gynecol 2003; 101 (1): 178–193.
Spinillo A, Capuzzo E, Stronati M, Ometto A, Orcesi S, Fazzi E . Effect of preterm premature rupture of membranes on neurodevelopmental outcome: follow up at two years of age. Br J Obstet Gynaecol 1995; 102 (11): 882–887.
Dammann O, Allred EN, Veelken N . Increased risk of spastic diplegia among very low birth weight children after preterm labor or prelabor rupture of membranes. J Pediatr 1998; 132 (3 Pt 1): 531–535.
Ananth CV, Oyelese Y, Srinivas N, Yeo L, Vintzileos AM . Preterm premature rupture of membranes, intrauterine infection, and oligohydramnios: risk factors for placental abruption. Obstet Gynecol 2004; 104 (1): 71–77.
Kurkinen-Raty M, Koivisto M, Jouppila P . Perinatal and neonatal outcome and late pulmonary sequelae in infants born after preterm premature rupture of membranes. Obstet Gynecol 1998; 92 (3): 408–415.
Murphy DJ, Sellers S, MacKenzie IZ, Yudkin PL, Johnson AM . Case-control study of antenatal and intrapartum risk factors for cerebral palsy in very preterm singleton babies. Lancet 1995; 346 (8988): 1449–1454.
Hannah ME, Ohlsson A, Farine D, Hewson SA, Hodnett ED, Myhr TL et al. Induction of labor compared with expectant management for prelabor rupture of the membranes at term. N Engl J Med 1996; 334 (16): 1005–1010.
Ramsey PS, Nuthalapaty FS, Lu G, Ramin S, Nuthalapaty ES, Ramin KD . Contemporary management of preterm premature rupture of membranes (PPROM): a survey of maternal-fetal medicine providers. Am J Obstet Gynecol 2004; 191 (4): 1497–1502.
Healy AJ, Veille JC, Sciscione A, McNutt LA, Dexter SC . The timing of elective delivery in preterm premature rupture of the membranes: a survey of members of the Society of Maternal-Fetal Medicine. Am J Obstet Gynecol 2004; 190 (5): 1479–1481.
Smith G, Rafuse C, Anand N, Brennan B, Connors G, Crane J et al. Prevalence, management, and outcomes of preterm prelabour rupture of the membranes of women in Canada. J Obstet Gynaecol Can 2005; 27 (6): 547–553.
Spinnato JA, Shaver DC, Bray EM, Lipshitz J . Preterm premature rupture of the membranes with fetal pulmonary maturity present: a prospective study. Obstet Gynecol 1987; 69 (2): 196–201.
Mercer BM, Crocker LG, Boe NM, Sibai BM . Induction versus expectant management in premature rupture of the membranes with mature amniotic fluid at 32 to 36 weeks: a randomized trial. Am J Obstet Gynecol 1993; 169 (4): 775–782.
Cox SM, Leveno KJ . Intentional delivery versus expectant management with preterm ruptured membranes at 30 to 34 weeks' gestation. Obstet Gynecol 1995; 86 (6): 875–879.
Naef III RW, Allbert JR, Ross EL, Weber BM, Martin RW, Morrison JC . Premature rupture of membranes at 34 to 37 weeks′ gestation: aggressive versus conservative management. Am J Obstet Gynecol 1998; 178 (1 Pt 1): 126–130.
Hartling L, Chari R, Friesen C, Vandermeer B, Lacaze-Masmonteil T . A systematic review of intentional delivery in women with preterm prelabor rupture of membranes. J Matern Fetal Neonatal Med 2006; 19 (3): 177–187.
Pasquier JC, Bujold E, Rabilloud M, Picaud JC, Ecochard R, Claris O et al. Effect of latency period after premature rupture of membranes on 2 years infant mortality (DOMINOS study). Eur J Obstet Gynecol Reprod Biol 2007; 135 (1): 21–27.
ACOG Committee on Practice Bulletins-Obstetrics. ACOG Practice Bulletin No. 80: premature rupture of membranes. Clinical management guidelines for obstetrician-gynecologists. Obstet Gynecol 2007; 109 (4): 1007–1019.
An international classification of retinopathy of prematurity. Pediatrics 1984; 74 (1): 127–133.
Bell MJ . Neonatal necrotizing enterocolitis. N Engl J Med 1978; 298 (5): 281–282.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500 gm. J Pediatr 1978; 92 (4): 529–534.
Mercer BM, Miodovnik M, Thurnau GR, Goldenberg RL, Das AF, Ramsey RD et al. Antibiotic therapy for reduction of infant morbidity after preterm premature rupture of the membranes. a randomized controlled trial. National institute of child health and human development maternal-fetal medicine units network. JAMA 1997; 278 (12): 989–995.
Picone S, Paolillo P . Neonatal outcomes in a population of late-preterm infants. J Matern Fetal Neonatal Med 2010; 23 (Suppl 3): 116–120.
Baron IS, Erickson K, Ahronovich MD, Baker R, Litman FR . Cognitive deficit in preschoolers born late-preterm. Early Hum Dev 2011; 87 (2): 115–119.
Engle WA, Tomashek KM, Wallman C . ‘Late-preterm’ infants: a population at risk. Pediatrics 2007; 120 (6): 1390–1401.
Romeo DM, Di SA, Conversano M, Ricci D, Mazzone D, Romeo MG et al. Neurodevelopmental outcome at 12 and 18 months in late preterm infants. Eur J Paediatr Neurol 2010; 14 (6): 503–507.
Strevens H, Allen K, Thornton JG . Management of premature prelabor rupture of the membranes. Ann NY Acad Sci 2010; 1205: 123–129.
Cousens S, Blencowe H, Gravett M, Lawn JE . Antibiotics for pre-term pre-labour rupture of membranes: prevention of neonatal deaths due to complications of pre-term birth and infection. Int J Epidemiol 2010; 39 (Suppl 1): i134–i143.
Yudin MH, van SJ, Van EN, Boucher M, Castillo E, Cormier B et al. Antibiotic therapy in preterm premature rupture of the membranes. J Obstet Gynaecol Can 2009; 31 (9): 863–874.
Hutzal CE, Boyle EM, Kenyon SL, Nash JV, Winsor S, Taylor DJ et al. Use of antibiotics for the treatment of preterm parturition and prevention of neonatal morbidity: a metaanalysis. Am J Obstet Gynecol 2008; 199 (6): 620–628.
Canavan TP, Simhan HN, Caritis S . An evidence-based approach to the evaluation and treatment of premature rupture of membranes: Part II. Obstet Gynecol Surv 2004; 59 (9): 678–689.
Canavan TP, Simhan HN, Caritis S . An evidence-based approach to the evaluation and treatment of premature rupture of membranes: Part I. Obstet Gynecol Surv 2004; 59 (9): 669–677.
Mercer BM . Management of preterm premature rupture of the membranes. Clin Obstet Gynecol 1998; 41 (4): 870–882.
Acknowledgements
We thank Dr Larry Stitt for statistical assistance, Gail Schmidt and Maria Sinacori for technical assistance, and Dr Renato Natale for his support of the perinatal database. Dr Dan Nayot received a Schulich Research Opportunities Program grant for his work on this project and Dr Barbra de Vrijer was supported by the Strategic Training Initiative in Research in the Reproductive Health Sciences (STIRRHS). Bryan S Richardson is the recipient of the Canada Research Chair in Fetal and Neonatal Health and Development. This paper has been presented SOGC 63rd Annual Clinical Meeting, 2007 (oral), and at the Society for Gynecological Investigation 55th Annual Meeting, 2008 (poster). Research was supported by the Schulich Research Opportunities Program, the Strategic Training Initiative in Research in the Reproductive Health Sciences (STIRRHS), and the Canada Research Chair in Fetal and Neonatal Health and Development.
Contribution to Authorship
Dr Dan Nayot contributed to the conception and design of the study, analyzed the data and prepared the manuscript. Drs Barbra de Vrijer and Debbie Penava, Orlando Da Silva and Bryan Richardson contributed to the conception and design of the study, guided the data analysis and helped critically revise the manuscript. All authors gave final approval to the manuscript for submission.
Details of Ethics Approval
This project was approved by the Health Sciences Research Ethics Board at the University of Western Ontario, London, Ontario, Canada (HSREB 12561E).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nayot, D., Penava, D., Da Silva, O. et al. Neonatal outcomes are associated with latency after preterm premature rupture of membranes. J Perinatol 32, 970–977 (2012). https://doi.org/10.1038/jp.2012.15
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2012.15
Keywords
This article is cited by
-
Perinatal outcomes of twin pregnancies with preterm premature rupture of the membranes at 24–34 weeks’ gestation
Scientific Reports (2021)
-
Risk factors and perinatal outcomes associated with latency in preterm premature rupture of membranes between 24 and 34 weeks of gestation
Archives of Gynecology and Obstetrics (2014)