Abstract
Objective:
Moderately premature infants, defined here as those born between  and
and  weeks gestation, comprise 3.9% of all births in the United States and 32% of all preterm births. Although long-term outcomes for these infants are better than for less mature infants, morbidity and mortality are still substantially increased in comparison with infants born at term. There is an added survival benefit resulting from birth at a tertiary neonatal care center, and although many of these infants require tertiary level care, delivery at lower level hospitals and subsequent neonatal transfer are still common. Our primary aim was to determine the impact of maternal characteristics and antenatal medical management on the early neonatal course of the moderately premature infant. The secondary aim was to create a clinical prediction rule to determine which infants require intubation and mechanical ventilation in the first 24 h of life. Such a prediction rule could inform the decision to transfer maternal–fetal patients before delivery to a facility with a Level III neonatal intensive care unit (NICU), where optimal care could be provided without the requirement for a neonatal transfer.
weeks gestation, comprise 3.9% of all births in the United States and 32% of all preterm births. Although long-term outcomes for these infants are better than for less mature infants, morbidity and mortality are still substantially increased in comparison with infants born at term. There is an added survival benefit resulting from birth at a tertiary neonatal care center, and although many of these infants require tertiary level care, delivery at lower level hospitals and subsequent neonatal transfer are still common. Our primary aim was to determine the impact of maternal characteristics and antenatal medical management on the early neonatal course of the moderately premature infant. The secondary aim was to create a clinical prediction rule to determine which infants require intubation and mechanical ventilation in the first 24 h of life. Such a prediction rule could inform the decision to transfer maternal–fetal patients before delivery to a facility with a Level III neonatal intensive care unit (NICU), where optimal care could be provided without the requirement for a neonatal transfer.
Study Design:
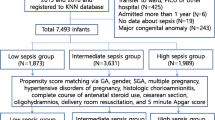
Data for this analysis came from the cohort of infants in the Moderately Premature Infant Project (MPIP) database, a multicenter cohort study of 850 infants born at gestational age  and
and  weeks, with birth weight between 1500 and 2499 g, who were discharged to home alive. We built a logistic regression model to identify maternal characteristics associated with need for tertiary care, as measured by administration of surfactant. Using statistically significant covariates from this model, we then created a numerical decision rule to predict need for tertiary care.
weeks, with birth weight between 1500 and 2499 g, who were discharged to home alive. We built a logistic regression model to identify maternal characteristics associated with need for tertiary care, as measured by administration of surfactant. Using statistically significant covariates from this model, we then created a numerical decision rule to predict need for tertiary care.
Result:
In multivariate modeling, four factors were associated with reduction in the need for tertiary care, including non-White race (odds ratio (OR)=0.5, (0.3, 0.7)), older gestational age, female gender (OR=0.6 (0.4, 0.8)) and use of antenatal corticosteroids (OR=0.5, (0.3, 0.8)). The clinical prediction rule to discriminate between infants who received surfactant, versus those who did not, had an area under the curve of 0.77 (0.73, 0.8).
Conclusion:
Four antenatal risk factors are associated with a requirement for Level III NICU care as defined by the need for surfactant administration. Future analyses will examine a broader spectrum of antenatal characteristics and revalidate the prediction rule in an independent cohort.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Gould JB, Marks AR, Chavez G . Expansion of community-based perinatal care in California. J Perinatol 2002; 22: 630–640.
Lasswell SM, Barfield WD, Rochat RW, Blackmon L . Perinatal regionalization for very low-birth-weight and very preterm infants: a meta-analysis. JAMA 2010; 304: 992–1000.
Lowery C, Bronstein J, McGhee J, Ott R, Reece EA, Mays GP . ANGELS and University of Arkansas for Medical Sciences paradigm for distant obstetrical care delivery. Am J Obstet Gynecol 2007; 196: 534 e531–539.
McCormick MC . The regionalization of perinatal care. Am J Public Health 1981; 71: 571–572.
McCormick MC, Richardson DK . Access to neonatal intensive care. Future Child 1995; 5: 162–175.
McCormick MC, Shapiro S, Starfield BH . The regionalization of perinatal services. Summary of the evaluation of a national demonstration program. JAMA 1985; 253: 799–804.
Mohamed MA, Aly H . Transport of premature infants is associated with increased risk for intraventricular haemorrhage. Arch Dis Child Fetal Neonatal Ed 2010; 95 (6): F403–F407.
Paneth N, Kiely JL, Susser M . Age at death used to assess the effect of interhospital transfer of newborns. Pediatrics 1984; 73: 854–861.
Paneth N, Kiely JL, Wallenstein S, Marcus M, Pakter J, Susser M . Newborn intensive care and neonatal mortality in low-birth-weight infants: a population study. N Engl J Med 1982; 307: 149–155.
Stark AR . Levels of neonatal care. Pediatrics 2004; 114: 1341–1347.
American Academy of Pediatrics and American College of Obsetrics and Gynecology. Guidelines for Perinatal Care, 6th edn. AAP: Elk Grove Village, IL; ALOG: Washington, DC, 2007.
Escobar GJ, McCormick MC, Zupancic JA, Coleman-Phox K, Armstrong MA, Greene JD et al. Unstudied infants: outcomes of moderately premature infants in the neonatal intensive care unit. Arch Dis Child Fetal Neonatal Ed 2006; 91: F238–F244.
Saigal S, Doyle LW . An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 2008; 371: 261–269.
Hibbard JU, Wilkins I, Sun L, Gregory K, Haberman S, Hoffman M et al. Respiratory morbidity in late preterm births. JAMA 2010; 304: 419–425.
Richardson DK, Reed K, Cutler JC, Boardman RC, Goodman K, Moynihan T et al. Perinatal regionalization versus hospital competition: the Hartford example. Pediatrics 1995; 96: 417–423.
Vieux R, Fresson J, Hascoet JM, Blondel B, Truffert P, Roze JC et al. Improving perinatal regionalization by predicting neonatal intensive care requirements of preterm infants: an EPIPAGE-based cohort study. Pediatrics 2006; 118: 84–90.
Harris TR, Isaman J, Giles HR . Improved neonatal survival through maternal transport. Obstet Gynecol 1978; 52: 294–300.
Hohlagschwandtner M, Husslein P, Klebermass K, Weninger M, Nardi A, Langer M . Perinatal mortality and morbidity. Comparison between maternal transport, neonatal transport and inpatient antenatal treatment. Arch Gynecol Obstet 2001; 265: 113–118.
Eichenwald EC, Zupancic JA, Mao WY, Richardson DK, McCormick MC, Escobar GJ . Variation in diagnosis of apnea in moderately preterm infants predicts length of stay. Pediatrics 2011; 127: e53–e58.
McCormick MC, Escobar GJ, Zheng Z, Richardson DK . Factors influencing parental satisfaction with neonatal intensive care among the families of moderately premature infants. Pediatrics 2008; 121: 1111–1118.
Profit J, McCormick MC, Escobar GJ, Richardson DK, Zheng Z, Coleman-Phox K et al. Neonatal intensive care unit census influences discharge of moderately preterm infants. Pediatrics 2007; 119: 314–319.
Profit J, Petersen LA, McCormick MC, Escobar GJ, Coleman-Phox K, Zheng Z et al. Patient-to-nurse ratios and outcomes of moderately preterm infants. Pediatrics 2010; 125: 320–326.
Profit J, Zupancic JA, McCormick MC, Richardson DK, Escobar GJ, Tucker J et al. Moderately premature infants at Kaiser Permanente Medical Care Program in California are discharged home earlier than their peers in Massachusetts and the United Kingdom. Arch Dis Child Fetal Neonatal Ed 2006; 91: F245–F250.
Wasson JH, Sox HC, Neff RK, Goldman L . Clinical prediction rules. Applications and methodological standards. N Engl J Med 1985; 313: 793–799.
Zupancic JA, Richardson DK, Horbar JD, Carpenter JH, Lee SK, Escobar GJ . Revalidation of the Score for Neonatal Acute Physiology in the Vermont Oxford Network. Pediatrics 2007; 119: e156–e163.
Escobar GJ, Shaheen SM, Breed EM, Botas C, Greene JD, Yoshida CK et al. Richardson score predicts short-term adverse respiratory outcomes in newborns >/=34 weeks gestation. J Pediatr 2004; 145: 754–760.
Richardson DK, Gray JE, McCormick MC, Workman K, Goldmann DA . Score for Neonatal Acute Physiology: a physiologic severity index for neonatal intensive care. Pediatrics 1993; 91: 617–623.
The CRIB (clinical risk index for babies) score: a tool for assessing initial neonatal risk and comparing performance of neonatal intensive care units. The International Neonatal Network. Lancet 1993; 342: 193–198.
Buhrer C, Metze B, Obladen M . CRIB, CRIB-II, birth weight or gestational age to assess mortality risk in very low birth weight infants? Acta Paediatr 2008; 97: 899–903.
Parry G, Tucker J, Tarnow-Mordi W . CRIB II: an update of the clinical risk index for babies score. Lancet 2003; 361: 1789–1791.
Broughton SJ, Berry A, Jacobe S, Cheeseman P, Tarnow-Mordi WO, Greenough A . The mortality index for neonatal transportation score: a new mortality prediction model for retrieved neonates. Pediatrics 2004; 114: e424–e428.
Burstyn I . Antepartum risk score predicts adverse birth outcomes. J Obstet Gynaecol Can 2010; 32: 16–20.
Tyson JE, Parikh NA, Langer J, Green C, Higgins RD . Intensive care for extreme prematurity—moving beyond gestational age. N Engl J Med 2008; 358: 1672–1681.
Hintz SR, Bann CM, Ambalavanan N, Cotten CM, Das A, Higgins RD . Predicting time to hospital discharge for extremely preterm infants. Pediatrics 2009; 125: e146–e154.
Lee SK, Zupancic JA, Pendray M, Thiessen P, Schmidt B, Whyte R et al. Transport risk index of physiologic stability: a practical system for assessing infant transport care. J Pediatr 2001; 139: 220–226.
Blackwell MT, Eichenwald EC, McAlmon K, Petit K, Linton PT, McCormick MC et al. Interneonatal intensive care unit variation in growth rates and feeding practices in healthy moderately premature infants. J Perinatol 2005; 25: 478–485.
Eichenwald EC, Blackwell M, Lloyd JS, Tran T, Wilker RE, Richardson DK . Inter-neonatal intensive care unit variation in discharge timing: influence of apnea and feeding management. Pediatrics 2001; 108: 928–933.
Blackmon LR, Barfield WD, Stark AR . Hospital neonatal services in the United States: variation in definitions, criteria, and regulatory status, 2008. J Perinatol 2009; 29: 788–794.
Shapiro-Mendoza CK, Tomashek KM, Kotelchuck M, Barfield W, Nannini A, Weiss J et al. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics 2008; 121: e223–e232.
Acknowledgements
The original data collection for MPIP was funded by the Agency for Health Care Research and Quality (RO1 HS 10131). Dr Dukhovny's work on this project was supported in part by the AHRQ T32 HS000063 Training Grant (2009 to 2010) and the National Institutes of Health Loan Repayment Program (2010 to 2012). We thank John D Greene from Kaiser Permanente for his statistical support on this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website
Supplementary information
Rights and permissions
About this article
Cite this article
Dukhovny, D., Dukhovny, S., Pursley, D. et al. The impact of maternal characteristics on the moderately premature infant: an antenatal maternal transport clinical prediction rule. J Perinatol 32, 532–538 (2012). https://doi.org/10.1038/jp.2011.155
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2011.155
Keywords
This article is cited by
-
Video-call based newborn triage system for local birth centres can be established without major instalment costs using commercially available smartphones
Scientific Reports (2020)
-
Comparison of state risk-appropriate neonatal care policies with the 2012 AAP policy statement
Journal of Perinatology (2018)
-
Characteristics of neonatal transports in California
Journal of Perinatology (2016)
-
United States and territory policies supporting maternal and neonatal transfer: review of transport and reimbursement
Journal of Perinatology (2016)