Abstract
Objective:
Respiratory distress syndrome (RDS), requiring mechanical ventilation and exogenous surfactant treatment, and patent ductus arteriosus (PDA), are common co-morbidities in very premature infants. The effects of intra-tracheal surfactant administration on the cardiovascular and pulmonary systems in very premature infants with RDS and PDAs are not well characterized. We evaluated the effects of poractant alfa and beractant, surfactants with different rapidity of onset and duration of action, in very premature infants with RDS. To assess whether there were differences in PDA hemodynamics in very premature infants with RDS treated with poractant alfa and beractant during the first week of life and to assess whether poractant alfa or beractant had a direct effect on PDAs and PDA hemodynamics following the second dose of surfactant.
Study Design:
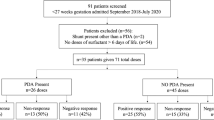
We studied 50 in-born, very premature infants with RDS, 24 0 of 7 to 29 6 of 7 weeks gestation, treated with poractant alfa or beractant, in an open label, 1:1, randomized clinical trial. A subgroup of 16 patients with severe RDS, treated with a second dose of surfactant, had echocardiographical assessments before and 20 to 30 min after the second dose of surfactant.
Result:
There were 25 infants treated with poractant alfa (27.1±1.6 weeks, birth weight 930±231 g) and 25 treated with beractant (26.7±1.7 weeks, P=0.407 and birth weight 898±282 g, P=0.666). Clinically significant PDAs were diagnosed and treated in 8 of 25 (32%) of the poractant alfa and 19 of 25 (76%) of the beractant group (P=0.002). Indomethacin treatment was slightly earlier (3.4±2.5 days) in the poractant alfa than in the beractant group (5.1±4.9 days, P=0.038). Right ventricle pressure (RVP)/systolic arterial pressure (SAP) ratio in the first week was slightly lower in the poractant alfa (64±20%) than in the beractant (78±26%, P=0.048) group. Following a second dose of surfactant, neither poractant alfa nor beractant changed PDA flow. These hemodynamic observations were associated with less respiratory support in the poractant alfa group, allowing earlier extubation (13 of 25 at 48 h and 15 of 25 at 72 h), than in the beractant group (6 of 25 at 48 h, P=0.044, and 8 of 25 at 72 h, P=0.049).
Conclusion:
The more rapid improvement in pulmonary function in the poractant alfa-treated infants was associated with a lower RVP/SAP ratio and a corresponding earlier treatment with indomethacin. Neither surfactant had a significant direct effect on PDA hemodynamics. The lower frequency of clinically significant PDAs in the poractant alfa compared with the beractant group may represent an indirect effect of the differences in the pulmonary improvement induced by the two surfactants.
Similar content being viewed by others
Introduction
Respiratory distress syndrome (RDS), requiring mechanical ventilation and exogenous surfactant treatment, and patent ductus arteriosus (PDA) are common co-morbidities in very premature infants. RDS requiring mechanical ventilation is treated with intra-tracheal surfactant.1 The combined hemodynamic and pulmonary effects of surfactant administration on PDA hemodynamics in this population are not well characterized. Intratracheal surfactant may have direct and indirect hemodynamic effects.2 Exogenous surfactant therapy, for example, may increase shunting across PDAs following rapid decreases in pulmonary vascular resistance.3 Previous studies comparing these surfactant therapies have shown a higher4 and lower5 frequency of PDAs in infants treated with poractant alfa compared with those treated with beractant. We evaluated the hemodynamic effects of beractant (Survanta, Ross Product Division, Abbott Laboratories) and poractant alpha (Curosurf, Dey LP, Napa, CA, USA and Chiesi Farmaceutici Spa, Parma, Italy), the two most commonly used modified animal-derived surfactants in the United States, in premature infants <30 weeks gestational age at birth with RDS. The goal of this paper was to describe PDA patency and hemodynamic differences in very premature infants with moderate to severe RDS treated with these two animal-derived surfactants. We were interested in both the potential direct and indirect effects of these surfactants on PDAs. Respiratory support data for this study population were presented in a companion publication.6
Methods
Study design
A multi-site 1:1 randomized clinical trial comparing poractant alfa (2.5 ml kg–1 for initial dose and 1.25 ml kg–1 subsequent doses) to beractant (4 ml kg–1 for initial and subsequent doses) among very premature, in-born infants <30 weeks gestation was conducted at Boston Medical Center and Caritas St Elizabeth Medical Center, minimizing the variability in initial management of the patients enrolled. Institutional Review Board approval was obtained from each institution. The study was registered NCT00767039. Informed consent was obtained before delivery. Between January 2005 and May 2008, 52 infants with RDS were enrolled and randomized to receive either poractant alfa or beractant for the initial and subsequent doses. Early death occurred in two patients in the beractant group, before a significant PDA could manifest, and these patients were eliminated from analysis for this portion of the study. Entry criteria were in-born premature infants with gestational age <30 week, birth weight >500 g, RDS requiring mechanical ventilation with mean airway pressure ⩾6 cm H2O and FiO2>30% before 8 h of life. Intratracheal surfactant was administered in two aliquots in left and right lateral positions, whereas the baby was supported on a volume cycle ventilator (Drager, Evita) with a tidal volume of 5 ml kg–1, rate 35 breaths per min, inspiratory time 0.35 s and FiO2 as need to maintain saturation 85 to 92%. Surfactant was administered as soon after birth as the diagnosis of RDS requiring intubation was made (within 6 h of birth). The first dose of beractant administration was at 24±17 min and the first dose of poractant alfa at 35±54 min. The endotracheal tube was not suctioned for 1 h following surfactant instillation, unless clinically indicated. Early surfactant administration did not eliminate the need for respiratory support before 72 h in any of the infants included in this study.
Echocardiograms were obtained at 2 to 7 days of life, before institution of medical treatment of PDAs, to assess ductal patency and hemodynamics in the two groups. As this was the time when most PDAs are recognized, many of these echocardiograms were obtained for clinical indications (heart murmur, persistent mechanical ventilation or on CPAP with respiratory deterioration, increased apnea, hypotension or wide pulse pressure, etc.). Asymptomatic patients had echocardiograms at the convenience of the echocardiography technician within the specified time. Only patients with symptomatic PDAs that were hemodynamically significant by echocardiography were treated as clinically indicated (medically or surgically). Medical treatment used standard indomethacin dosing.7 Subsequent echocardiograms were obtained as clinically indicated. Echocardiographical assessment included PDA size, right ventricular systolic pressure (RVP) derived from Doppler interrogation of Tricuspid regurgitant jet or PDA gradient, LA/Ao ratio, and systemic arterial blood pressure. Hemodynamically significant PDAs in patients on persistent respiratory support (ventilator or CPAP) were defined as having at least two of the following criteria: PDA>1.5 mm, diastolic retrograde flow in the descending aorta and/or left atrial enlargement with a left atrium to aortic root diameter ratio >1.4. Infants with significant congenital heart disease, multiple congenital anomalies or moribund infants anticipated to expire within the first 3 days of life were eliminated from the study. Echocardiograms were also obtained in a subset of 16 infants immediately before and 20 to 30 min after administration of the second dose of surfactant, to assess the direct effect of these surfactants on PDA hemodynamics. The differential effects of these surfactants on regional cerebral blood flow were previously reported.8
If a PDA was hemodynamically significant or became significant at a later time, the infants were treated with indomethacin, unless there were medical contraindications (clinical diagnosis of necrotizing enterocolitis, thrombocytopenia <100 000, or impaired renal function with a creatinine >1.6 or BUN>35). We recorded when the infant was treated with indomethacin, the number of 3 dose courses administered and if surgical ligation was necessary.
Data analysis
Data were presented as mean±s.d. A student's t-test for continuous or χ2 for discrete variables, was used to determine statistical significance between the two groups for demographical (GA, gender, race, birth weight, antenatal betamethasone administration and SNAP II score), hemodynamic and treatment data. Apgar scores are presented as median (25 and 75 percentile), and compared using a Mann–Whitney rank sum test. The study was not designed to evaluate the long-term morbidities. The respiratory data were collected with corresponding hemodynamic data, to evaluate the effect of the two surfactant preparations on PDAs and PDA hemodynamics. Data analysis for this paper was generated using SAS software, Version 9.13 of the SAS System for Windows. Copyright 2004 SAS Institute SAS and all other SAS Institute product or service names are registered trademarks or trademarks of SAS Institutes, Cary, NC, USA.
Results
A total of 52 subjects were enrolled, 25 patients randomized to poractant alfa and 27 to beractant therapy group. Two patients in the beractant group died in the first week of life, before they would have been considered candidates for PDA treatment, and were eliminated from the data analysis. The demographic characteristics of each group were similar and shown in Table 1. Overall, 8 of 25 (32%) of the infants treated with poractant alfa and 19 of 25 (76%, P=0.002) of the infants treated with beractant had PDAs treated with indomethacin or surgical ligation (Table 2). PDA ligations were required in 4 of 25 (16%) of the poractant alfa and 7 of 25 (28%, P=0.311) of infants treated with beractant. Infants in the poractant alfa group tended to be treated earlier (3.4±2.5 days), than infants treated with beractant (5.1±4.9 days, P=0.038). The differences in PDA treatment between groups was associated with differences in the respiratory status that allowed early extubation (Figure 1) of more infants in the poractant alfa group (13 of 25, 52% at 48 h and 15 of 25, 60% at 72 h), than in the beractant group (6 of 25, 24% at 48 h, P=0.044, and 8 of 25, 32% at 72 h, P=0.049).
To determine whether there were early hemodynamic differences in the infants treated with poractant alfa and beractant, we prospectively performed echocardiographic evaluations of the infants at 2 to 7 days of life, before initiation of therapy for significant PDAs (Table 3). There were 25 infants in the poractant alfa and 25 in the beractant group that had echocardiographic studies in the first week. In the first week of life, PDAs (any size) were present in 15 of 25 (60%) of infants treated with poractant alfa and 14 of 25 (56%, P=0.562) infants treated with beractant. PDAs >1.5 mm were present in 12 of 25 (48%) of the poractant alfa group, with a mean PDA diameter of 2.4±1.1 mm, and 10 of 25 (40%, P=0.573), with a mean diameter of 2.5±0.6 mm (P=0.698), of the beractant treated infants. During the first week of life, RVP/Systolic Arterial Blood Pressure (SAP) was slightly lower in the poractant alfa (64±20%) than in the beractant group (78±26%, P=0.048). Of the infants with any PDA in the first week of life, 8 of 15 (53%) of the infants in the poractant alfa and 14 of 14 (100%, P=0.0039) of the infants in the beractant group were treated with indomethacin or surgical ligation for significant PDAs during their NICU hospitalization. In addition, 5 infants in the beractant group developed hemodynamically significant PDAs after the first week. Poractant alfa treated infants required less respiratory support in the first 3 days of life than those treated with beractant (6). Thus, there was a difference in the PDA management and hemodynamics in infants treated with poractant alfa, compared with beractant that was associated with improvement in respiratory status.
To determine whether there was a direct hemodynamic effect of surfactant on PDAs, we assessed PDA hemodynamics before (5 min baseline) and 20 to 30 min after the second dose of poractant alfa and beractant administration in 16 infants with RDS and PDAs (Table 4). The second or third dose of surfactant was administered for a mean airway pressure ⩾6 cm H2O and FiO2>30%. A portion of these data were previously reported.8 In the poractant alfa and beractant treated infants, PDA size (1.9±0.8 vs 1.9±0.8 mm, respectively, P=0.901), mean blood flow velocity (1.0±0.8 vs 0.8±0.5 m s–1, respectively, P=0.883) and calculated flow (123±119 vs 137±107 cc min–1, respectively, P=0.654) were similar, and did not change significantly from baseline with surfactant administration. Similarly, RVP (35±12 vs 39±13 mm Hg, P=0.555) and RVP/SAP (71±24 vs 87±14%, P=0.352) in infants treated with poractant alfa and beractant were similar, and did not change significantly with surfactant administration. Thus, in the first days of life, neither surfactant appeared to have a significant direct affect on PDA patency or on the hemodynamic effect.
Discussion
The primary finding of this study is a description of the interaction between pulmonary function and PDA hemodynamics in very premature infants with RDS, treated with poractant alfa or beractant. This is a highly selected population of very premature infants with RDS requiring mechanical ventilation; infants that were at greatest risk for common morbidities of prematurity, including hemodynamically significant PDAs. While early echocardiograms at 2 to 7 days showed a similar frequency and size of PDAs in each group, fewer infants in the poractant alfa group were treated with indomethacin or surgical ligation than in the beractant group. Medical treatment of significant PDAs tended to be earlier in the poractant alfa treated infants, corresponding to a significantly lower RVP/Sys Art BP ratio than in the beractant group. These differences were associated with a more rapid and sustained improvement in respiratory function in the poractant alfa group, allowing more elective extubations at 48 and 72 h than in the beractant group.6 We did not demonstrate a direct surfactant effect on PDA closure or PDA hemodynamics by echocardiographic evaluation following the second dose of poractant alfa or beractant. Since PDAs tended to be treated earlier in the poractant alpha group, yet there were more PDAs treated in the beractant group, it is unlikely that early treatment of PDAs that would have close spontaneously, accounted for the lower number of PDAs treated in the poractant alfa group. Furthermore, since the number and size of PDAs seen in the echocardiograms performed at 2 to 7 days were similar in the two groups, there appears to be other factors responsible for persistence of the PDAs in the beractant than in the poractant alfa group. We believe the difference in pulmonary function or need for persistent mechanical ventilation was directly or indirectly responsible for the difference in PDAs treated in the two groups.
We speculate that the improved pulmonary status in the poractant alfa group allowed more PDA closures than in the beractant group. Either less aggressive clinical management of PDAs in infants on CPAP or nasal cannula oxygen or improved pulmonary status facilitating PDA closure may explain the differences in PDAs treated in the two groups. Although we performed serial echocardiograms to monitor PDA closure and remain as objective as possible, PDA treatment was not blinded to the open label surfactant administered. We believe that our study is the most comprehensive, prospective echocardiographical evaluation available of PDAs, comparing the interaction between the effects of two different surfactant preparations and PDA hemodynamics in very premature infants with RDS. We included an evaluation of the effects of surfactant in the first week of life and a limited evaluation of the acute effect (first hour after surfactant administration) for two surfactant preparations. To our knowledge, there is no similar study. Our data support the hypothesis that therapies that induce a sustained improvement in respiratory function and require less mechanical ventilation may be associated with a lower incidence of hemodynamically significant PDAs.
The need to evaluate responses to different surfactant preparations and timing of the evaluations is important in the evaluations of hemodynamic responses to surfactant preparations. For example, the cerebral blood flow response to a prophylactic first surfactant dose of beractant or poractant alfa decreased cerebral blood flow whereas cerebral blood flow increased following a second dose of beractant and did not change with the second dose of poractant alfa.8, 9 We speculated that the unifying hypothesis was that the cerebral blood flow responses mirrored the acute increases or decreases in pCO2 associated with surfactant administration.8, 9 Differences in surfactant preparations, volume and timing of administration probably explain the widely different cerebral blood flow responses to surfactant. Previous studies reported that cerebral blood flow decreased,10, 11, 12, 13 increased9, 14, 15, 16, 17, 18 and remained unchanged19, 20, 21, 22, 23, 24 following various surfactant preparations, administered under varying conditions. Thus, as with the cerebral circulation, we believe that the differential pulmonary effects of beractant and poractant alfa may be responsible for indirect effects on PDAs and PDA hemodynamics.
The rapid onset of action of poractant alfa in improving lung compliance and oxygenation, compared with beractant, reduced the need for mechanical ventilation in premature infants with RDS.6, 25 Improved oxygenation may increase PDA closure rates.26 Higher levels of positive pressure mechanical ventilation in the beractant group, compared with the poractant alfa group, may have stimulated a chronic inflammatory response that has been associated with development of chronic lung disease and PDAs through activation of the inflammatory cascade and prostaglandin synthesis.27, 28 Our findings are analogous to improved pulmonary status and lesser need for PDA treatment in infants treated with early caffeine treatment,29 where no direct effect of caffeine on periductal ductal smooth muscle constriction was demonstrable.30
The primary weaknesses of this study were the small sample size, open label design and high rate of PDAs in the beractant group. This is a highly selected population of very premature infants who were mechanically ventilated for RDS, infants with the greatest risk of developing the morbidities of prematurity, including PDAs and chronic lung disease. Our observation extends the findings of Malloy et al.5 who also found a lower incidence of PDAs in infants treated with poractant alfa, compared with beractant-treated infants.
In conclusion, this is a comprehensive, prospective, hemodynamic study examining the interaction of two animal-derived surfactant preparations on PDAs and PDA hemodynamics in very premature infants with RDS. There were fewer significant PDAs requiring medical or surgical treatment in infants treated with poractant alfa, than in those treated with beractant. The differences in PDA treatment and hemodynamics were associated with a differential effect on respiratory support. The infants treated with poractant alfa required less mechanical ventilatory support than those treated with beractant. Neither poractant alfa nor beractant had direct hemodynamic effects on PDAs or PDA hemodynamics following the second surfactant dose in infants with severe RDS. We speculate that the difference in PDAs was due to an indirect differential effect of these surfactant preparations on pulmonary function and associated PDA closure. Further studies will be needed to confirm our observation and clarify this relationship.
References
Hoekstra RE, Jackson JC, Myers T, Frantz ID, Stern ME, Powers WF et al. Improved neonatal survival following multiple doses of bovine surfactant in very premature neonates at risk for respiratory distress syndrome. Pediatrics 1991; 88: 10–18.
Moen A, Rootwelt T, Robertson B, Curstedt T, Hall C, Saugstad OD . Hemodynamics and tissue blood flow after porcine surfactant replacement in surfactant-depleted newborn piglets. Pediatr Res 1996; 40: 215–224.
Clyman RI, Jobe A, Heymann M, Ikegami M, Roman C, Payne B et al. Increased shunt through the patent ductus arteriosus after surfactant replacement therapy. J Pediatr 1982; 100: 101–107.
Heldt GP, Pesonen E, Merritt TA, Elias W, Sahn DJ . Closure of the ductus arteriosus and mechanics of breathing in preterm infants after surfactant replacement therapy. Pediatr Res 1989; 25: 305–310.
Malloy CA, Nicoski P, Muraskas JK . A randomized trial comparing beractant and poractant treatment in neonatal respiratory distress syndrome. Acta Paediatr 2005; 94: 779–784.
Fujii AM, Patel SM, Allen R, Doros G, Guo CY, Testa S . Poractant alfa and beractant treatment of very premature infants with respiratory distress syndrome. J Perinatol (in press).
Young TE, Mangum B . NeoFAX, 16th edn. 2003. Acorn Publishing, Inc. Raleigh, NC.
Fujii AM, Bailey J, Doros G, Sampat K, Sikes NC, Mason MJ et al. Effects of beractant and poractant administration on cerebral hemodynamics. J Neonatal-Perinatal Med 2009; 2: 27–34.
Kaiser JR, Gauss CH, Williams DK . Surfactant administration acutely affects cerebral and systemic hemodynamics and gas exchange in very low birth weight infants. J Pediatr 2004; 144: 809–814.
Cowan F, Whitelaw A, Wertheim D, Silverman M . Cerebral blood flow velocity changes after rapid administration of surfactant. Arch Dis Child 1991; 66: 1105–1109.
Schipper JA, Mohammad GI, van Straaten HLM, Koppe JG . The impact of surfactant replacement therapy on cerebral and systemic circulation and lung function. Eur J Pediatr 1997; 156: 224–227.
Rey M, Segerer H, Kiessling C, Obladen M . Surfactant bolus instillation: effects of different doses on blood pressure and cerebral blood flow velocities. Biol Neonate 1994; 66: 16–21.
Murdoch E, Kempley ST . Randomized trial examining cerebral haemodynamics following artificial or animal surfactant. Acta Paediatr 1998; 87: 411–415.
Skov L, Bell A, Greisen G . Surfactant administration and the cerebral circulation. Biol Neonate 1992; 61: 31–36.
Fahnenstich H, Schmidt S, Spaniol S, Kowalewski S . Relative changes in oxyhemoglobin, deoxyhemoglobin and intracranial blood volume during surfactant replacement therapy in infants with respiratory distress syndrome. Dev Pharmacol Ther 1991; 17: 150–153.
Dorrepaal CA, Benders MJNL, Steendijk P, van de Bor M, van Bel F . Cerebral hemodynamics and oxygenation in preterm infants after low- vs. high-dose surfactant replacement therapy. Biol Neonate 1993; 64: 193–200.
van Bel F, de Winter PJ, Wijnands HBG, van de Bor M, Egberts J . Cerebral and aortic blood flow velocity patterns in preterm infants receiving prophylactic surfactant treatment. Acta Paediatr 1992; 81: 504–510.
Skov L, Hellström-Westas L, Jacobsen T, Greisen G, Svenningsen NW . Acute changes in cerebral oxygenation and cerebral blood volume in preterm infants during surfactant treatment. Neuropediatrics 1992; 23: 126–130.
Jorch G, Rabe H, Garbe M, Michel E, Gortner L . Acute and protracted effects of intratracheal surfactant application on internal carotid blood flow velocity, blood pressure and carbondioxide tension in very low birth weight infants. Eur J Pediatr 1989; 148: 770–773.
Roll C, Knief J, Horsch S, Hanssler L . Effect of surfactant administration on cerebral haemodynamics and oxygenation in premature infants—a near infrared spectroscopy study. Neuropediatrics 2000; 31: 16–23.
Nuntnarumit P, Bada HS, Yang W, Korones SB . Cerebral blood flow velocity changes after bovine natural surfactant instillation. J Perinatol 2000; 20: 240–243.
Bell AH, Skov L, Lundstrøm KE, Saugstad OD, Greisen G . Cerebral blood flow and plasma hypoxanthine in relation to surfactant treatment. Acta Paediatr 1994; 83: 910–914.
Rabe H, Jorch G . Cerebral hemodynamics in perinatal pharmacology. Dev Pharmacol Ther 1991; 17: 128–132.
Edwards AD, McCormick DC, Roth SC, Elwell CE, Peebles DM, Cope M et al. Cerebral hemodynamic effects of treatment with modified natural surfactant investigated by near infrared spectroscopy. Pediatr Res 1992; 32: 532–536.
Saugstad OD, Halliday HL, Robertson B, Speer CP . Replacement therapy with porcine natural surfactant—current status and future challenges. Biol Neonate 1993; 64: 269–278.
McMurphy DM, Heymann MA, Rudolph AM . Developmental changes in constriction of the ductus arteriosus: responses to oxygen and vasoactive agents in the isolated ductus arteriosus of the fetal lamb. Pediatr Res 1972; 6: 693.
Naik AS, Kallapur SG, Bachurski CJ, Jobe AH, Michna J, Kramer BW et al. Effects of ventilation with different positive end-expiratory pressures on cytokine expression in the preterm lamb lung. Am J Respir Crit Care Med 2001; 164: 494–498.
Watterberg KL, Scott SM, Backstrom C, Gifford KL, Cook KL . Links between early adrenal function and respiratory outcome in preterm infants: airway inflammation and patent ductus arteriosus. Pediatrics 2000; 105: 320–324.
Schmidt B, Roberts RS, Davis P, Doyle LW, Barrington KJ, Ohlsson A et al. Caffeine therapy for apnea of prematurity. N Engl J Med 2006; 354: 2112–2121.
Clyman RI, Roman C . The effects of caffeine on the preterm sheep ductus arteriosus. Pediatr Res 2007; 52: 167–169.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Dr Fujii was supported by an unrestricted research grant from Dey LP, Napa, CA and Chiesi Farmaceutici Spa, Parma, Italy. The remaining authors declare no conflict of interest.
The funders had no involvement in study design, in data collection, analysis/interpretation of the data, in the writing of the paper or in the decision to submit the paper for publication.
Rights and permissions
This work is licensed under the Creative Commons Attribution-NonCommercial-No Derivative Works 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Fujii, A., Allen, R., Doros, G. et al. Patent ductus arteriosus hemodynamics in very premature infants treated with poractant alfa or beractant for respiratory distress syndrome. J Perinatol 30, 671–676 (2010). https://doi.org/10.1038/jp.2010.21
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.21
Keywords
This article is cited by
-
Risk stratification of hemodynamically significant patent ductus arteriosus by clinical and genetic factors
World Journal of Pediatrics (2023)
-
Porcine versus bovine surfactant therapy for RDS in preterm neonates: pragmatic meta-analysis and review of physiopathological plausibility of the effects on extra-pulmonary outcomes
Respiratory Research (2020)
-
Have we been down this road before?
Journal of Perinatology (2010)
-
Is there really a clinical difference in surfactant preparations?
Journal of Perinatology (2010)