Abstract
Objective:
Delayed cord clamping (DCC) may be beneficial in very-preterm and very-low-birth-weight infants.
Study Design:
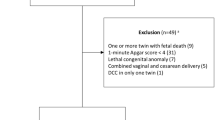
This study was a randomized unmasked controlled trial. It was performed at three centers of the NICHD (National Institute of Child Health and Human Development) Neonatal Research Network. DCC in very-preterm and very-low-birth-weight infants will result in an increase in hematocrit levels at 4 h of age. Infants with a gestational age of 24 to 28 weeks were randomized to either early cord clamping (<10 s) or DCC (30 to 45 s). The primary outcome was venous hematocrit at 4 h of age. Secondary outcomes included delivery room management, selected neonatal morbidities and the need for blood transfusion during the infants’ hospital stay.
Result:
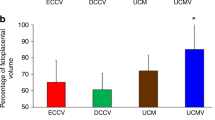
A total of 33 infants were randomized: 17 to the immediate cord clamping group (cord clamped at 7.9±5.2 s, mean±s.d.) and 16 to the DCC (cord clamped at 35.2±10.1 s) group. Hematocrit was higher in the DCC group (45±8% vs 40±5%, P<0.05). The frequency of events during delivery room resuscitation was almost identical between the two groups. There was no difference in the hourly mean arterial blood pressure during the first 12 h of life; there was a trend in the difference in the incidence of selected neonatal morbidities, hematocrit at 2, 4 and 6 weeks, as well as the need for transfusion, but none of the differences was statistically significant.
Conclusion:
A higher hematocrit is achieved by DCC in very-low-birth-weight infants, suggesting effective placental transfusion.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Dunn PM . Postnatal placental transfusion. Dev Med Child Neurol 1996; 8: 607–608.
Usher RH, Shephard M, Lind J . The blood volume of the newborn infant and placental transfusion. Acta Paediatr Scand 1963; 52: 497–512.
Oh W, Blankenship W, Lind J . Further study of neonatal blood volume in relation to placental transfusion. Ann Pediatr 1966; 207: 147–159.
Usher RH, Lind J . Blood volume of the newborn premature infant. Acta Paediatr Scand 1965; 54: 419–431.
Lindercamp O, Nelle KM, Zilow EP . The effect of early and late cord clamping on blood viscosity and other hemorheological parameters parameters in full-term neonates. Acta Paediatr 1992; 81: 745–750.
Nelle M, Zilow EP, Bastert G, Linderkamp O . Effect of Leboyer childbirth on cardiac output, cerebral and gastro-intestinal blood flow velocities in full term neonates. Am J Perinatol 1995; 12: 212–216.
Oh W, Lind J, Gessner IH . Circulatory and respiratory adaptation to early and late cord clamping in newborn infants. Acta Paediatr Scand 1966; 55: 17–25.
Oh W, Oh MA, Lind J . Renal function and blood volume in newborn infant related to placental transfusion. Acta Paediatr Scand 1966; 55: 197–210.
Oh W, Wallgren G, Hanson JS, Lind J . The effects of placental transfusion on respiratory mechanics of normal term infants. Pediatrics 1967; 40: 6–12.
Usher RH, Saigal S, O’Neill A, Surainder Y, Chua L-B . Estimation of red blood cell volume in premature infants with and without respiratory distress syndrome. Biol Neonate 1975; 26: 241–248.
Kinmond S, Aitchison TC, Holland BM, Jones JG, Turner TL, Wardrop CA . Umbilical cord clamping and preterm infants: a randomized trial. BMJ 1993; 306: 172–175. 12.
Aladangady N, McHugh S, Aitchison TC, Wardrop CAJ, Holland BM . Infants’ blood volume in a controlled trial of placental transfusion at preterm delivery. Pediatrics 2006; 117: 93–98.
Rabe H, Wacker A, Hülskamp G, Hörnig-Franz I, Schulze-Everding A, Harms E et al. A randomized controlled trial of delayed cord clamping in very low birth weight preterm infants. Eur J Pediatr 2000; 159: 775–777.
Mercer JS, McGrath MM, Hensman A, Silver H, Oh W . Immediate and delayed cord clamping in infants born between 24 and 32 weeks: a pilot randomized controlled trial. J Perinatol 2003; 23: 466–472.
Mercer JS, Vohr BR, McGrath MM, Padbury JF, Wallach M, Oh W . Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late onset sepsis: a randomized, controlled trial. Pediatrics 2006; 117 (4): 1434–1435.
Rabe H, Reynolds G, Diaz-Rossello J . Early versus delayed umbilical cord clamping in preterm infants. Cochrane Database Systematic Review 2004; 4, Article number: CD003248.
Rabe H, Reynolds G, Diaz-Rossello J . A systematic review and meta-analysis of a brief delay in clamping the umbilical cord of preterm infants. Neonatology 2008; 93: 138–144.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1500. J Pediatr 1978; 92: 529–534.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis: therapeutic decisions based upon clinical staging. Ann Surg 1978; 187: 1–7.
Ultee CA, van der Deure J, Swart J, Lasham C, van Baar AL . Delayed cord clamping in preterm infants delivered at 34 36 week's gestation: a randomised controlled trial. Arch Dis Child 2008; 93 (1): F20–F23.
Kurtzberg J, Laughlin M, Graham ML, Smith C, Olson J, Halperin E et al. Cord blood as a source of hematopoietic stem cells for transplantation into unrelated recipients. New Engl J Med 1996; 325: 167–170.
Haneline LS, Marshall KP, Clapp DW . The highest concentration of primitive hematopoietic progenitor cells in cord blood is found in extremely premature infants. Pediatr Res 1996; 39: 820–825.
Hosono S, Mugishima H, Fujita H, Hosono A, Okada T, Takahashi S et al. Blood pressure and urine output during the first 120 hours of life in infants born at less than 29 weeks gestation related to umbilical cord milking. Arch Dis Child 2009; 94: F328–F331.
Hosono S, Mugishima H, Fujita H, Hosono A, Minato M, Okada T et al. Umbilical cord milking reduces the need for red cell transfusions and improves neonatal adaptation in infants born at less than 29 weeks gestation: a randomized controlled trial. Arch Dis Child 2008; 93: F14–F19.
Tolosa JN, Park DH, Eve DJ . Mankind's first natural stem cell transplant. J Cell Mol Med 2010; 14: 488–495.
Acknowledgements
The National Institutes of Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) provided grant support for the Neonatal Research Network's Delayed Cord Clamping Study. Data collected at the participating sites of the NICHD Neonatal Research Network (NRN) were transmitted to RTI International, the Data Coordinating Center (DCC) for the network, which stored, managed and analyzed the data for this study. On behalf of the NRN, Dr W Kenneth Poole (DCC principal investigator) and Scott McDonald (DCC statistician) had full access to all the data in the study and take responsibility for the integrity of the data and for accuracy of the data analysis. We are indebted to our medical and nursing colleagues and to the infants and their parents who agreed to take part in this study. The following investigators, in addition to those listed as authors, participated in this study: NRN Steering Committee Chair—Alan Jobe, MD, PhD, University of Cincinnati; Brown University, Women and Infants Hospital of Rhode Island (U10 HD27904)—Angelita Hensman, BSN RNC; Case Western Reserve University, Rainbow Babies and Children's Hospital (U10 HD21364, M01 RR80)—Michele C Walsh, MD, MS; Nancy S Newman, BA RN; Eunice Kennedy Shriver National Institute of Child Health and Human Development—Linda L Wright, MD; Elizabeth M McClure, Med; RTI International (U01 HD36790)—Abhik Das, PhD; Betty Hastings; Jeanette O’Donnell Auman, BS; Carolyn Petrie Huitema, MS; Scott E Schaefer, MS; Kristin Zaterka-Baxter, RN; and University of Alabama at Birmingham Health System and Children's Hospital of Alabama (U10 HD34216, M01 RR32)—Monica V Collins, RN BSN MaEd; Shirley S Cosby, RN BSN.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Oh, W., Fanaroff, A., Carlo, W. et al. Effects of delayed cord clamping in very-low-birth-weight infants. J Perinatol 31 (Suppl 1), S68–S71 (2011). https://doi.org/10.1038/jp.2010.186
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.186