Abstract
Objective:
To investigate whether maternal migraine was associated with preterm birth.
Study Design:
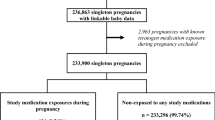
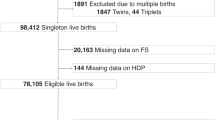
Case–control sample within a population-based study of risk factors for cerebral palsy (CP). Infants without CP were matched for gestational age with those with CP. Maternal migraine was self-identified at first prenatal visit, most in the first trimester.
Result:
Infants without CP born to women with migraine had a higher rate of preterm birth (odds ratio (OR)=3.5, 95% confidence interval (CI) 1.5, 8.5), as did infants who died in the perinatal period (OR=7.3, 95% CI 0.98, 54), the difference marginal for nominal statistical significance. In all outcome groups, infants of women with migraine had a higher observed rate of suboptimal intrauterine growth. In term infants, the rate of maternal migraine was higher in those with CP than in controls (OR=2.18, 95% CI 0.92, 5.25). Pre-eclampsia was reported more frequently in women with migraine who gave birth to a child with CP or a perinatal death, particularly in those born preterm; OR=5.1 (1.3, 20) and OR=2.9 (1.1, 7.6), respectively, but not in women giving birth to a control whether term or preterm.
Conclusion:
Maternal migraine, as self-reported early in pregnancy, was associated with preterm birth in survivors without CP and in infants who died in the perinatal period. The combination of maternal migraine and pre-eclampsia was associated with CP and perinatal death. The association of maternal migraine with outcomes of pregnancy warrants further study.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Lateef TM, Merikangas KR, He J, Kalaydjian A, Khoromi S, Knight E et al. Headache in a national sample of American children: prevalence and comorbidity. J Child Neurol 2009; 24: 536–543.
Lipton RB, Bigal ME . The epidemiology of migraine. Am J Med 2005; 118 (Suppl 1): 3S–10S.
Contag SA, Mertz HL, Bushnell CD . Migraine during pregnancy: is it more than a headache? Nat Rev Neurol 2009; 5: 449–456.
Schurks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T . Migraine and cardiovascular disease: systematic review and meta-analysis. BMJ 2009; 339: b3914.
Del Sette M . Migraine and cerebrovascular risk. Neurol Sci 2010; 31 (Suppl 1): S127–S128.
MacClellan LR, Giles W, Cole J, Wozniak M, Stern B, Mitchell BD et al. Probable migraine with visual aura and risk of ischemic stroke: the stroke prevention in young women study. Stroke 2007; 38: 2438–2445.
Bushnell CD, Jamison M, James AH . Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. BMJ 2009; 338: b664.
Banhidy F, Acs N, Horvath-Puho E, Czeizel AE . Pregnancy complications and delivery outcomes in pregnant women with severe migraine. Eur J Obstet Gynecol Reprod Biol 2007; 134: 157–163.
Facchinetti F, Allais G, Nappi RE, D’Amico R, Marozio L, Bertozzi L et al. Migraine is a risk factor for hypertensive disorders in pregnancy: a prospective cohort study. Cephalalgia 2009; 29: 286–292.
Sanchez SE, Qiu C, Williams MA, Lam N, Sorensen TK . Headaches and migraines are associated with an increased risk of preeclampsia in Peruvian women. Am J Hypertens 2008; 21: 360–364.
Simbar M, Karimian Z, Afrakhteh M, Akbarzadeh A, Kouchaki E . Increased risk of pre-eclampsia (PE) among women with the history of migraine. Clin Exptl Hypertension 2010; 32: 159–165.
Craici IM, Wagner SJ, Hayman SR, Garovic VD . Pre-eclamptic pregnancies: an opportunity to identify women at risk for future cardiovascular disease. Womens Health (Lond Engl) 2008; 4: 133–135.
Nyholt DR, Gillespie NG, Merikangas KR, Treloar SA, Martin NG, Montgomery GW . Common genetic influences underlie comorbidity of migraine and endometriosis. Genet Epidemiol 2009; 33: 105–113.
Blair E, Liu Y, Cosgrove P . Choosing the best estimate of gestational age from routinely collected population-based perinatal data. Paediatr Perinat Epidemiol 2004; 18: 270–276.
Blair EM, Liu Y, de Klerk NH, Lawrence DM . Optimal fetal growth for the Caucasian singleton and assessment of appropriateness of fetal growth: an analysis of a total population perinatal database. BMC Pediatr 2005; 5: 13.
Olesen C, Steffensen FH, Sorensen HT, Nielsen GL, Olsen J . Pregnancy outcome following prescription for sumatriptan. Headache 2000; 40: 20–24.
Kallen B, Lygner PE . Delivery outcome in women who used drugs for migraine during pregnancy with special reference to sumatriptan. Headache 2001; 41: 351–356.
Soldin OP, Dahlin J, O’Mara DM . Triptans in pregnancy. Ther Drug Monit 2008; 30: 5–9.
McElrath TF, Hecht JL, Dammann O, Boggess K, Onderdonk A, Markenson G et al. Pregnancy disorders that lead to delivery before the 28th week of gestation: an epidemiologic approach to classification. Am J Epidemiol 2008; 168: 980–989.
Hamed SA . The vascular risk associations with migraine: relation to migraine susceptibility and progression. Atherosclerosis 2009; 205: 15–22.
Gudmundsson LS, Aspelund T, Scher AI, Thorgeirsson G, Johannsson M, Launer LJ et al. C-reactive protein in migraine sufferers similar to that of non-migraineurs: the Reykjavik Study. Cephalalgia 2009; 29: 1301–1310.
Bockowski L, Sobaniec W, Zelazowska-Rutkowska B . Proinflammatory plasma cytokines in children with migraine. Pediatr Neurol 2009; 41: 17–21.
Rotton WN, Sachtleben MR, Friedman EA . Migraine and eclampsia. Obstet Gynecol 1959; 14: 322–330.
Lee J, Croen LA, Backstrand KH, Yoshida CK, Henning LH, Lindan C et al. Maternal and infant characteristics associated with perinatal arterial stroke in the infant. JAMA 2005; 293: 723–729.
Cindrova-Davies T . Gabor Than Award Lecture 2008: pre-eclampsia—from placental oxidative stress to maternal endothelial dysfunction. Placenta 2009; 30 (Suppl A): S55–S65.
Stam AH, Haan J, van den Maagdenberg AM, Ferrari MD, Terwindt GM . Migraine and genetic and acquired vasculopathies. Cephalalgia 2009; 29: 1006–1017.
Castro MJ, Stam AH, Lemos C, de Vries B, Vanmolkot KR, Barros J et al. First mutation in the voltage-gated Nav1.1 subunit gene SCN1A with co-occurring familial hemiplegic migraine and epilepsy. Cephalalgia 2009; 29: 308–313.
Cnattingius S, Mills JL, Yuen J, Eriksson O, Salonen H . The paradoxical effect of smoking in preeclamptic pregnancies: smoking reduces the incidence but increases the rates of perinatal mortality, abruptio placentae, and intrauterine growth restriction. Am J Obstet Gynecol 1997; 177: 156–161.
Aamodt AH, Stovner LJ, Hagen K, Brathen G, Zwart J . Headache prevalence related to smoking and alcohol use. The Head-HUNT Study. Eur J Neurol 2006; 13: 1233–1238.
Wallis AB, Saftlas AF . Untangling an epidemiological knot: migraine and preeclampsia. Am J Hypertens 2008; 21: 245.
Stagnaro-Green A, Chen X, Bogden JD, Davies TF, Scholl TO . The thyroid and pregnancy: a novel risk factor for very preterm delivery. Thyroid 2005; 15: 351–357.
Badawi N, Kurinczuk JJ, Keogh JM, Alessandri LM, O’Sullivan F, Burton PR et al. Antepartum risk factors for newborn encephalopathy: the Western Australian case-control study. BMJ 1998; 317: 1549–1553.
Ellis M, Manandhar N, Manandhar DS, Costello AM . Risk factors for neonatal encephalopathy in Kathmandu, Nepal, a developing country: unmatched case-control study. BMJ 2000; 320: 1229–1236.
Badawi N, Felix JF, Kurinczuk JJ, Dixon G, Watson L, Keogh JM et al. Cerebral palsy following term newborn encephalopathy: a population-based study. Dev Med Child Neurol 2005; 47: 293–298.
Levine RJ, Vatten LJ, Horowitz GL, Qian C, Romundstad PR, Yu KF et al. Pre-eclampsia, soluble fms-like tyrosine kinase 1, and the risk of reduced thyroid function: nested case-control and population based study. BMJ 2009; 339: b4336.
Wainscott G, Sullivan FM, Volans GN, Wilkinson M . The outcome of pregnancy in women suffering from migraine. Postgrad Med J 1978; 54: 98–102.
Maggioni F, Alessi C, Maggino T, Zanchin G . Headache during pregnancy. Cephalalgia 1997; 17: 765–769.
Acknowledgements
The authors are grateful to the National Health and Medical Research Council of Australia for support, and to Linda Watson and Jan de Groot for their valuable contributions to data extraction and management. This study was supported by the National Health and Medical Research Council of Australia under Program grant no. 353514, approved by the Princess Margaret Hospital/King Edward Memorial Hospital Ethics Committee, the Confidentiality of Health Information Committee of the WA Department of Health and by individual hospital and regional ethics committees where required.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Blair, E., Nelson, K. Migraine and preterm birth. J Perinatol 31, 434–439 (2011). https://doi.org/10.1038/jp.2010.148
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.148
Keywords
This article is cited by
-
The Impact of Parental Migraine on Children
Current Pain and Headache Reports (2020)
-
Agreement of self-reported physician diagnosis of migraine with international classification of headache disorders-II migraine diagnostic criteria in a cross-sectional study of pregnant women
BMC Women's Health (2013)
-
Triptan safety during pregnancy: a Norwegian population registry study
European Journal of Epidemiology (2013)
-
Italian guidelines for primary headaches: 2012 revised version
The Journal of Headache and Pain (2012)
-
Migraine in women: the role of hormones and their impact on vascular diseases
The Journal of Headache and Pain (2012)