Abstract
Objective:
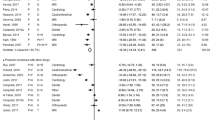
The ideal combination of premedication for neonatal tracheal intubation has not been established. The aim of this preliminary study was to compare the intubation conditions between propofol and midazolam as premedication for tracheal intubation in neonates.
Study Design:
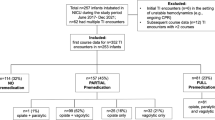
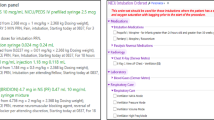
A double-blinded, randomized, controlled trial was performed, and 20 preterm neonates (28 to 34 week) underwent tracheal intubation following the use of remifentanil associated to either propofol (n=10) or midazolam (n=10). Intubation conditions were scored according to a four-point scale.
Result:
According to the main outcome measured (identification of a 50% difference in the intubation conditions), there were no differences regarding the number of attempts and the overall intubation conditions among the groups (P=1.00).
Conclusion:
Both combinations of premedications have no differences regarding the quality of intubation, which could be of clinical interest. Besides midazolam, propofol could be a valid alternative as hypnotic for premedication for endotracheal intubation in neonates.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Carbajal R, Eble B, Anand KJS . Premedication for tracheal intubation in neonates: confusion or controversy? Semin Perinatol 2007; 31 (5): 309–317.
Silva YP, Gomez RS, Marcatto JDO, Maximo TA, Barbosa RF, Simões e Silva AC . Morphine versus remifentanil for intubating preterm neonates. Arch Dis Child Fetal Neonatal Ed 2007; 92: 93–94.
Penido MG, Garra R, Sammartino M, Silva YP . Remifentanil in neonatal intensive care and anaesthesia practice. Acta Paediatr 2010; 99 (10): 1454–1463.
Welzing L, Kribs A, Huenseler C, Eifinger F, Mehler K, Roth B . Remifentanil for InSurE in preterm infants: a pilot study for evaluation of efficacy and safety aspects. Acta Paediatr 2009; 98: 1419–1420.
Greenwood CS, Colby CE . Pharmacology review: premedication for endotracheal intubation of the neonate: what is the evidence? Neoreviews 2009; 10: 31–35.
Lagercrantz H, Changeux JP . The emergence of human consciousness: from fetal to neonatal life. Pediatr Res 2009; 65: 255–260.
Lagercrantz H, Changeux JP . Basic consciousness of the newborn. Semin Perinatol 2010; 34: 201–206.
Attardi DM, Paul DA, Tuttle DJ, Greenspan JS . Premedication for intubation in neonates. Arch Dis Child Fetal Neonatal Ed 2000; 83: F161.
Kumar P, Denson SE, Mancuso TJ, Committee on Fetus and Newborn, Section on Anesthesiology and Pain Medicine. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics 2010; 125: 608–615.
Papoff P, Mancuso M, Caresta E, Moretti C . Effectiveness and safety of propofol in newborn infants. Pediatrics 2008; 121: 448.
Viby-Mogensen J, Engbaek J, Eriksson L, Gramstad L, Jensen E, Jensen FS et al. Good clinical research practice (GCRP) in pharmacodynamic studies of neuromuscular blocking agents. Acta Anaesthesiol Scand 1996; 40: 59–74.
Lawrence J, Alcock D, McGrath P, Kay J, MacMurray SB, Dulberg C . The development of a tool to assess neonatal pain. Neonatal Netw 1993; 12: 59–66.
Ambuel B, Hamlett KW, Marx CM, Blumer JL . Assessing distress in pediatric intensive care environments: the COMFORT scale. J Pediatric Psychol 1992; 17: 95–105.
Duncan HP, Zurick NJ, Wolf AR . Should we reconsider awake neonatal intubation? A review of the evidence and treatment strategies. Paediatr Anaesth 2001; 11: 135–145.
Shah V, Ohlsson A . The effectiveness of premedication for endotracheal intubation in mechanically ventilated neonates: a systematic review. Clin Perinatol 2002; 29: 535–554.
Lago P, Garetti E, Merrazi D, Pieragostini L, Ancora G, Pirelli A et al. Guidelines for procedural pain in the newborn. Acta Paediatr 2009; 98: 932–939.
Allegaert K, Peeters MY, Verbesselt R, Tibboel D, Naulaers G, de Hoon JN et al. Inter-individual variability in propofol pharmacokinetics in preterm and term neonates. Br J Anaesth 2007; 99: 864–870.
Ghanta S, Abdel-Latif ME, Lui K, Ravindranathan H, Awad J, Oei J . Propofol compared with morphine, atropine, and suxamethonium regimen as induction agents for neonatal endotracheal intubation: a randomized, controlled trial. Pediatrics 2007; 119: 1248–1255.
Marsh DF, Hodkinson B . Remifentanil in paediatric anaesthetic practice. Anaesthesia 2009; 64: 301–308.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Penido, M., de Oliveira Silva, D., Tavares, E. et al. Propofol versus midazolam for intubating preterm neonates: a randomized controlled trial. J Perinatol 31, 356–360 (2011). https://doi.org/10.1038/jp.2010.135
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2010.135
Keywords
This article is cited by
-
Evaluation of the safety of using propofol for paediatric procedural sedation: A systematic review and meta-analysis
Scientific Reports (2019)
-
Remifentanil: applications in neonates
Journal of Anesthesia (2016)