Abstract
Study Objective:
This study evaluated peripheral vasoconstriction in extremely low birth weight (ELBW) infants when body temperature decreased during the first 12 h of life.
Study Design:
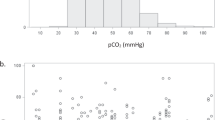
An exploratory, within-subjects design with 10 ELBW infants. Abdominal and foot temperatures were measured every minute. Peripheral vasoconstriction (abdominal>peripheral temperature by 2 °C) and abdominal–peripheral temperature difference were also evaluated. Results:Abdominal and peripheral temperatures were significantly correlated within each infant. One 880 g infant exhibited isolated peripheral vasoconstriction; a 960-g infant had abdominal temperatures >1 °C higher than peripheral temperatures. Eight smaller infants exhibited no peripheral vasoconstriction and spent most of their observations with peripheral greater than abdominal temperatures. In eight infants, mean temperature difference was significantly higher when abdominal temperature was <36.5 °C.
Conclusion:
Most ELBW infants did not exhibit peripheral vasoconstriction during their first 12 h of life, despite low temperatures. ELBW infants’ vasomotor control may be immature during this period.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Knobel R, Holditch-Davis D . Themoregulation and heat loss prevention after birth and during neonatal intensive-care unit stabilization of extremely-low-birth weight infants. J Obstet Gynecol Neonatal Nurs 2007; 36: 280–287.
Thomas K . Preterm infant thermal responses to caregiver differ by incubator control mode. J Perinatol 2003; 23: 640–645.
Buetow K, Klein S . Effect of maintenance of ‘normal’ skin temperature on survival of infants of low birth weight. Pediatrics 1964; 34: 163–170.
Day R, Caliguiri L, Kamenski C, Ehrlich F . Body temperature and survival of premature infants. Pediatrics 1964; 34: 171–181.
Hazan J, Maag U, Chessex P . Association between hypothermia and mortality rate of premature infant—revisited. Am J Obstet Gynecol 1991; 164: 111–112.
Vohra S, Grent G, Campbell V, Abbott M, Whyte R . Effect of polyethylene occlusive skin wrapping on heat loss in very low birth weight infants at delivery: a randomized trial. J Pediatr 1999; 134: 547–551.
Hull D, Smales O . Heat production in the newborn. In: Sinclair J (ed). Temperature Regulation and Energy Metabolism in the Newborn. Gurne & Stratton: New York, 1978. pp 129–156.
Houstek J, Vizek K, Pavelka S, Kopecky J, Krejcova E, Hermanska J . Type II iodothyronine 5′-deiodinase and uncoupling protein in brown adipose tissue of human newborns. J Clin Endocrinol Metab 1993; 77: 382–387.
Lyon A, Pikaar M, Badger P, McIntosh N . Temperature control in very low birthweight infants during first five days of life. Arch Dis Child Fetal Neonatal Ed 1997; 76: F47–F50.
Horns K . Comparison of two microenvironments and nurse caregiving on thermal stability of ELBW infants. Adv Neonatal Care 2002; 2 (3): 149–160.
Mok Q, Bass C, Ducker D, McIntosh N . Temperature instability during nursing procedures in preterm neonates. Arch Dis Child 1991; 66: 783–786.
Bailey J, Rose P . Temperature measurement in the preterm infant: a literature review. J Neonatal Nurs 2000; 6: 28–32.
Simbrunner G . Temperature measurements and distribution of temperatures throughout the body in neonates. In: Okken A, Koch J (eds). Thermoregulation of Sick and Low Birth Weight Neonates. Springer-Verlag Berlin: Germany, 1995. pp 53–62.
Harpin VA, Rutter N . Development of emotional sweating in the newborn infant. Arch Dis Child 1982; 57: 691–695.
Sanders M, Allen M, Alexander G, Yankowitz J, Graeber J, Johnson TR et al. Gestational age assessment in preterm neonates weighing less than 1500 grams. Pediatrics 1991; 88: 542–546.
Longin E, Gerstner T, Schaible T, Lenz T, Konig S . Maturation of the autonomic nervous system: differences in heart rate variability in premature vs term infants. J Perinat Med 2006; 34 (4): 303–308.
Gournay V, Drouin E, Roze JC . Development of baroflex control of heart rate in preterm and full term infants. Arch Dis Child Fetal Neonatal Ed 2002; 86 (3): F151–F154.
Allen MC . Assessment of gestational age and neuromaturation. Ment Retard Dev Disabil Res Rev 2005; 11: 21–33.
Osborn DA, Evans N, Kluckow M . Hemodynamic and antecedent risk factors of early and late periventricular/intraventricular hemorrhage in premature infants. Pediatrics 2003; 112: 33–39.
Paulson O, Strandgaard S, Edvinsson L . Cerebral autoregulation. Cerebrovasc Brain Metab Rev 1990; 2: 161–192.
Kehrer M, Blumenstock G, Ehehalt S, Goelz R, Poets C, Schoning M . Development of cerebral blood flow volume in preterm neonates during the first two weeks of life. Pediatr Res 2005; 58: 927–930.
Meek J, Tyszczuk L, Elwell C, Wyatt J . Cerebral blood flow increases over the first three days of life in extremely preterm neonates. Arch Dis Child Fetal Neonatal Ed 1998; 78: F33–F37.
Acknowledgements
We thank the parents of the infants in this study for consenting to the study, as they anticipated the arrival of their preterm infant and the nurses, respiratory therapists, and doctors that worked with these infants at Pitt County Memorial Hospital in Greenville, NC. I also thank Dr Virginia Neelon, Dr Suzanne Thoyre, and John White for their thoughtful contributions to this study. Funding support was provided by National Service Research Award, 1F31 NR09143 from the National Institute of Nursing Research, NIH; American Nurses Foundation: Nurses Charitable Trust District V FNA Scholar Research Grant; and Foundation of Neonatal Research and Education Grant.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Knobel, R., Holditch-Davis, D., Schwartz, T. et al. Extremely low birth weight preterm infants lack vasomotor response in relationship to cold body temperatures at birth. J Perinatol 29, 814–821 (2009). https://doi.org/10.1038/jp.2009.99
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.99
Keywords
This article is cited by
-
Facial thermal response to non-painful stressor in premature and term neonates
Pediatric Research (2023)
-
A method for improving semantic segmentation using thermographic images in infants
BMC Medical Imaging (2022)
-
Body temperature instability and respiratory morbidity in the very low birth weight infant: a multiple case, intensive longitudinal study
BMC Pediatrics (2020)
-
Primary healthcare worker knowledge related to prenatal and immediate newborn care: a cross sectional study in Masindi, Uganda
BMC Health Services Research (2014)
-
Les températures cutanées locales mesurées en pratique clinique sont-elles prédictives de la température cutanée moyenne chez le nouveau-né prématuré ?
Revue de médecine périnatale (2013)