Abstract
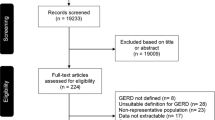
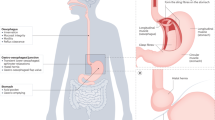
A global evidence-based consensus has defined gastroesophageal reflux disease (GERD) as ‘a condition, which develops when the reflux of stomach contents causes troublesome symptoms and/or complications.’ The manifestations of GERD can be divided into esophageal and extraesophageal syndromes, and include vomiting, poor weight gain, dysphagia, abdominal or substernal/retrosternal pain, esophagitis and respiratory disorders. The extraesophageal syndromes have been divided into established and proposed associations: established would include cough, laryngitis, asthma and dental erosion ascribable to reflux, whereas proposed associations would include pharyngitis, sinusitis, idiopathic pulmonary fibrosis and recurrent otitis media. Uninvestigated patients with esophageal symptoms without evidence of esophageal injury would be considered to have asymptomatic esophageal syndromes, whereas those with demonstrable injury are considered to have esophageal syndromes with esophageal injury. Therefore, this allows symptoms to define the disease but permits further characterization if mucosal injury is found. Within the syndromes with associated injury are reflux esophagitis, stricture, Barrett's esophagitis and adenocarcinoma. This review will address definitions of GER and GERD-associated symptoms and treatment options.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Vandeplas Y, Sacre-Smits L . Continuous 24-h esophageal monitoring in 285 asymptomatic infants 0–15 moths old. J Pediatr Gastroenterol Nutr 1987; 6: 220–224.
Gustafsson PM, Tibbling L . 24-h oesophageal two-level pH monitoring in healthy children and adolescents. Scand J Gastroenterol 1988; 23: 91–94.
J Rudolph CD, Mazur LJ, Liptak GS, Baker RD, Boyle JT, Colletti RB et al. Guidelines for evaluation and treatment of gastroesophageal reflux in infants and children: recommendations of the North American Society for Pediatric Gastroenterology and Nutrition. Pediatr Gastroenterol Nutr 2001; 32: S1–31.
Vakil N, van Zanten SV, Kahrilas P, Dent J, Lones R, the Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based concensus. Am J Gastroenterol 2006; 101: 1900–1920.
Nelson SP, Chen EH, Syniar GM, Christoffel KK . Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Pediatric Practice Research Group. Arch Pediatr Adolesc Med 1997; 151: 569–572.
Nelson SP, Chen EH, Syniar GM, Christoffel KK . One-year follow-up of symptoms of gastroesophageal reflux during infancy. Pediatric Research Practice Group. Pediatrics 1998; 102: E67.
Stanghellini V . Relationship between upper gastrointestinal symptoms and lifestyle, psychosocial factors and co-morbidity in the general population: Results from the domestic/international gastroenterology surveillance study [DIGEST]. Scand J Gastrenterol Suppl 1999; 231: 29–37.
Dent J, El-Serag HB, Wallander MA, Johansson S . Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2005; 54 (5): 710–717.
Werlin SL, D'Souza BJ, Hogan WJ, Dodds WJ, Arndorfer RC . Sandifer syndrome: an unappreciated clinical entity. Dev Med Clin Neurol 1980; 22: 374–378.
Herbst JJ, Johnson DG, Oliveros MA . Gastroesophageal reflux with protein losing enteropathy and clinical clubbing. Am J Dis Child 1976; 130: 1256–1258.
Hassall E . Barrett's esophagus: new definitions and approaches in children. J Pediatric Gastroenterol Nutr 1993; 16: 345–364.
Hu FZ, Preston RA, Post JC, White GJ, Kikuchi LW, Wang X et al. Mapping of a gene for severe pediatric gastroeshageal reflux to chromosome 13q14. JAMA 2000; 284: 325–334.
Seibert JJ, Byrne WJ, Euler AR, Latture T, Leach M, Campbell M . Gastroesophageal reflux-the acid test: scintigraphy or the pH probe? AJR Am J Roentgenol 1983; 140: 1087–1090.
Meyers WF, Roberts CC, Johnson DG, Herbst JJ . Value of tests for evaluation of gastroesophageal reflux in children. J Pediatr Surg 1985; 20: 515–520.
Chen MY, Ott DJ, Sinclair JW, Wu WC, Gelfrand DW . Gastroesophageal reflux disease: correlation of esophageal pH testing and radiographic findings. Radiology 1992; 185 (2): 483–486.
Buts JP, Barudi C, Moulin D, Claus D, Cornu G, Otte JB . Prevalence and treatment of silent gastroesophageal reflux in children with recurrent respiratory disorders. Eur J Pediatr 1986; 145: 396–400.
Malfroot A, Vandenplas Y, Verlinden M, Piepsz A, Dab I . Gastroesophageal reflux and unexplained chronic respiratory disease in infants and children. Pediat Pulmonol 1987; 3: 208–218.
Ostrom KM, Jacobs JR, Merritt RJ, Murray RD . Decreased regurgitation with a soy formula containing added soy fiber. Clin Pediatr 2006; 45: 29–36.
Vandenplas Y, Sacre L . Milk-thickening agents as a treatment for gastroesophageal reflux [published erratum appears in Clin Pediatr 1987; 26: 148]. Clin Pediatr 1987; 26: 66–68.
Bailey DJ, Andres JM, Danek GD, Pineiro-Carero VM . Lack of efficacy of thickened feeds as treatment for gastroesophageal reflux. J Pediatr 1987; 110: 187–189.
Orenstein SR, Magill HL, Brooks P . Thickening of infant feedings for therapy of gastroesophageal reflux. J Pediatr 1987; 110: 181–186.
Khoshoo V, Edell D, Thompson A, Rubin M . Are we overprescribing anitreflux medications for infants with regurgitation? Pediatrics 2007; 120 (5): 946–949.
Vanderhoof JA, Moran RA, Harris CL, Merkel KL, Orenstein SR . Efficacy of a prethickened infant formula: a multicenter, double blind, randomized placebo-controlled parallel group trial in 104 infants with symptomatic gastroesophageal reflux. Clin Pediatr 2003; 42: 483–495.
Vandenplas Y, Sacre-Smits L . Seventeen-hour continuous esophageal pH monitoring in the newborn: evaluation of the influence of position in asymptomatic and symptomatic babies. J Pediatr Gastroenterol Nutr 1985; 4 (3): 356–361.
Tobin JM, McCloud P, Cameron DJS . Posture and gastroesophageal reflux: a case for left lateral positioning. Arch Dis Child 1997; 76: 254–258.
Meyers WF, Herbst JJ . Effectiveness of positioning therapy for gastroesophageal reflux. Pediatrics 1982; 69 (6): 768–772.
van Wijk MP, Benninga MA, Dent J, Lontis R, Goodchild L, McCall LM et al. Effect of body position changes on postprandial gastroesophageal reflux and gastric emptying in the healthy premature neonate. J Pediatr 2007; 151 (6): 560–561.
Corvatlia L, Rotatori R, Ferlini M, Aceti A, Ancora G, Faldella G . The effect of body positioning on gastroesophageal reflux in premature infants: evaluation by combined impedance and pH monitoring. J Pediatr 2007; 151 (6): 591–596e1.
Sabesin SM, Berlin RG, Humphries TJ, Bradstreet DC, Walton-Bowen KL, Zaidi S . Famotidine relieves symptoms of gastroesophageal reflux disease and heals erosions and ulcerations. Results of a multicenter, placebo-controlled, dose ranging study. USA Merck Gastroesophageal Reflux Disease Study Group. Arch Intern Med 1991; 151 (12): 2394–2400.
Wolfe MM, Sachs G . Acid Suppression: optimizing therapy for gastroduodenal ulcer healing, gastroesophageal reflux disease, and stress-related erosive syndrome. Gastroeneterology 2000; 118: S9–S31.
Cucchiara S, Gobio-Casali L, Balli F, Magazzu GS, Staiano A, Astofli R et al. Cimetidine treatment of reflux esophagitis in children: an italian multicentric study. J Pediatr Gastroenterol Nutr 1989; 8 (2): 150–156.
Simeone D, Caria MC, Miele E, Staiano A . Treatment of childhood peptic esophagitis: a double blind placebo-controlled trial of nizatidine. J Pediatr Gastroenterol Nutr 1997; 25 (1): 51–55.
Chiba N, De Gara CJ, Wilkinon JM, Hunt RH . Speed of healing and symptom relief in grade II to IV gastroesophageal reflux disease: a metanalysis. Gastroenterology 1997; 112 (6): 1798–1810.
Barron JJ, Tan H, Spalding J, Bakst AW, Singer J . Proton pump inhibitor utilization patterns in infants. J Pediatr Gastroenterol Nutr 2007; 45: 421–427.
Omari TI, Haslam RR, Lundborg PS, Davidson GP . Effect of omeprazole on acid gastroesophageal reflux and gastric acidity in preterm infants with pathological acid reflux. J Pediatr Gastroenterol Nutr 2007; 44: 41–44.
Moore DJ, Tao B, Lines DR, Hirte C, Heddle ML, Davidson GP . Double-blind placebo-controlled trial of omeprazole in irritable infants with gastroesophageal reflux. J Pediatr 2003; 143: 219–223.
Hibbs AM, Lorch SA . Metochlopramide for the treatment of gastroesophageal reflux disease in infants. A systematic review. Pediatrics 2006; 118: 746–752.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bhatia, J., Parish, A. GERD or not GERD: the fussy infant. J Perinatol 29 (Suppl 2), S7–S11 (2009). https://doi.org/10.1038/jp.2009.27
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.27
Keywords
This article is cited by
-
A meta-analysis of outcomes after open and laparoscopic Nissen’s fundoplication for gastro-oesophageal reflux disease in children
Pediatric Surgery International (2011)