Abstract
Objective:
To determine oxygen saturation (SpO2) trends in healthy preterm newborns during the first 15 min after birth and to ascertain factors affecting SpO2 changes during that period.
Study Design:
An observational study was conducted. Preterm newborns with gestational age (GA) less than 35 weeks, who did not require oxygen supplementation during the first 15 min of life, were enrolled. Pulse oximetry was applied to the right hand immediately after birth. SpO2 data were recorded continuously every 2 s and were then transferred to a Microsoft Excel spreadsheet for analysis. The time to reach a stable SpO2 ⩾85 or ⩾90% was described by the Kaplan–Meier method and compared using log-rank test.
Result:
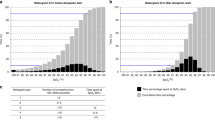
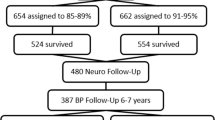
A total of 102 preterm newborns were eligible, of whom 27 were excluded, resulting in 75 newborns enrolled into the study with a median (range) GA of 35 (29 to 35) weeks, median (range) birth weight of 2390 (1270 to 2990) g and median (range) Apgar scores at 1 and 5 min of 9 (5 to 10) and 10 (7 to 10), respectively. There was a gradual increase in SpO2 with time. The median (interquartile range, IQR) SpO2 at 2, 3, 4, 5 and 6 min was 77% (72 to 92), 84% (75 to 94), 88% (80 to 94), 90% (79 to 95) and 95% (85 to 97), respectively. Newborns with a lower GA seemed to have lower SpO2 values. The median (IQR) time to reach a stable SpO2 ⩾85 or ⩾90% was 4 (3 to 6) and 5 (3 to 57) min, respectively. The mode of delivery was a significant factor affecting SpO2; infants delivered by cesarean section had a significantly lower SpO2 and took a longer time to reach SpO2 ⩾85% compared with those delivered by vaginal delivery (HR=1.96, 95% CI=1.11 to 3.49; P=0.02). All enrolled newborns had no serious complications and they survived to discharge.
Conclusion:
SpO2 in preterm newborns gradually increased with time. Approximately half of the preterm newborns had an SpO2 <90% during the first 5 min of life. Infants delivered by cesarean section had a lower SpO2 than those delivered by vaginal delivery.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
House JT, Schultetus RR, Gravenstein N . Continuous neonatal evaluation in the delivery room by pulse oximetry. J Clin Monit 1987; 3 (2): 96–100.
Dimich I, Singh PP, Adell A, Hendler M, Sonnenklar N, Jhaveri M . Evaluation of oxygen saturation monitoring by pulse oximetry in neonates in the delivery system. Can J Anaesth 1991; 38 (8): 985–988.
Toth B, Becker A, Seelbach-Gobel B . Oxygen saturation in healthy newborn infants immediately after birth measured by pulse oximetry. Arch Gynecol Obstet 2002; 266 (2): 105–107.
Kamlin CO, O'Donnell CP, Davis PG, Morley CJ . Oxygen saturation in healthy infants immediately after birth. J Pediatr 2006; 148 (5): 585–589.
Rabi Y, Yee W, Chen SY, Singhal N . Oxygen saturation trends immediately after birth. J Pediatr 2006; 148 (5): 590–594.
Mariani G, Dik PB, Ezquer A, Aguirre A, Esteban ML, Perez C et al. Pre-ductal and post-ductal O2 saturation in healthy term neonates after birth. J Pediatr 2007; 150 (4): 418–421.
Sendak MJ, Harris AP, Donham RT . Use of pulse oximetry to assess arterial oxygen saturation during newborn resuscitation. Crit Care Med 1986; 14 (8): 739–740.
Kopotic RJ, Lindner W . Assessing high-risk infants in the delivery room with pulse oximetry. Anesth Analg 2002; 94 (1 Suppl): S31–S36.
Dawson JA, Kamlin CO, Wong C, te Pas AB, O'Donnell CP, Donath SM et al. Oxygen saturation and heart rate during delivery room resuscitation of infants <30 weeks' gestation with air or 100% oxygen. Arch Dis Child Fetal Neonatal Ed 2009; 94 (2): F87–F91.
Spector LG, Klebanoff MA, Feusner JH, Georgieff MK, Ross JA . Childhood cancer following neonatal oxygen supplementation. J Pediatr 2005; 147 (1): 27–31.
Vento M, Asensi M, Sastre J, Lloret A, Garcia-Sala F, Vina J . Oxidative stress in asphyxiated term infants resuscitated with 100% oxygen. J Pediatr 2003; 142 (3): 240–246.
Vento M, Sastre J, Asensi MA, Vina J . Room-air resuscitation causes less damage to heart and kidney than 100% oxygen. Am J Respir Crit Care Med 2005; 172 (11): 1393–1398.
Tan A, Schulze A, O'Donnell CP, Davis PG . Air versus oxygen for resuscitation of infants at birth. Cochrane Database Syst Rev 2005; (2): CD002273.
International Liaison Committee on Resuscitation. 2005 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendation. Part 7; Neonatal Resuscitation. Resuscitation 2005; 67: 293–303.
American Heart Association. Newborn resuscitation guidelines. Circulation 2005; 112 (Suppl): IV-188–IV-195.
Escrig R, Arruza L, Izquierdo I, Villar G, Saenz P, Gimeno A et al. Achievement of targeted saturation values in extremely low gestational age neonates resuscitated with low or high oxygen concentrations: a prospective, randomized trial. Pediatrics 2008; 121 (5): 875–881.
Wang CL, Anderson C, Leone TA, Rich W, Govindaswami B, Finer NN . Resuscitation of preterm neonates by using room air or 100% oxygen. Pediatrics 2008; 121 (6): 1083–1089.
Acknowledgements
We thank Professor Dr Amnuay Thithapandha and Professor Aroonwan Preutthipan for their valuable comments and suggestions, and to Sam Ormond for editing the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Nuntnarumit, P., Rojnueangnit, K. & Tangnoo, A. Oxygen saturation trends in preterm infants during the first 15 min after birth. J Perinatol 30, 399–402 (2010). https://doi.org/10.1038/jp.2009.178
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2009.178
Keywords
This article is cited by
-
Oxygen saturation centiles in healthy preterm neonates in the first 10 min of life: a prospective observational study
European Journal of Pediatrics (2023)
-
A critical appraisal of tools for delivery room assessment of the newborn infant
Pediatric Research (2021)
-
Neuroinflammation in preterm babies and autism spectrum disorders
Pediatric Research (2019)